Omskæring - PICO 2 Anæstesi
Omskæring - PICO 2 Anæstesi
Review information
Authors
Styrelsen for Patientsikkerhed
1
1
18-Dec-2019
[Empty affiliation]
Citation example: SfP. Omskæring - PICO 2 Anæstesi. Cochrane Database of Systematic Reviews [Year], Issue [Issue].
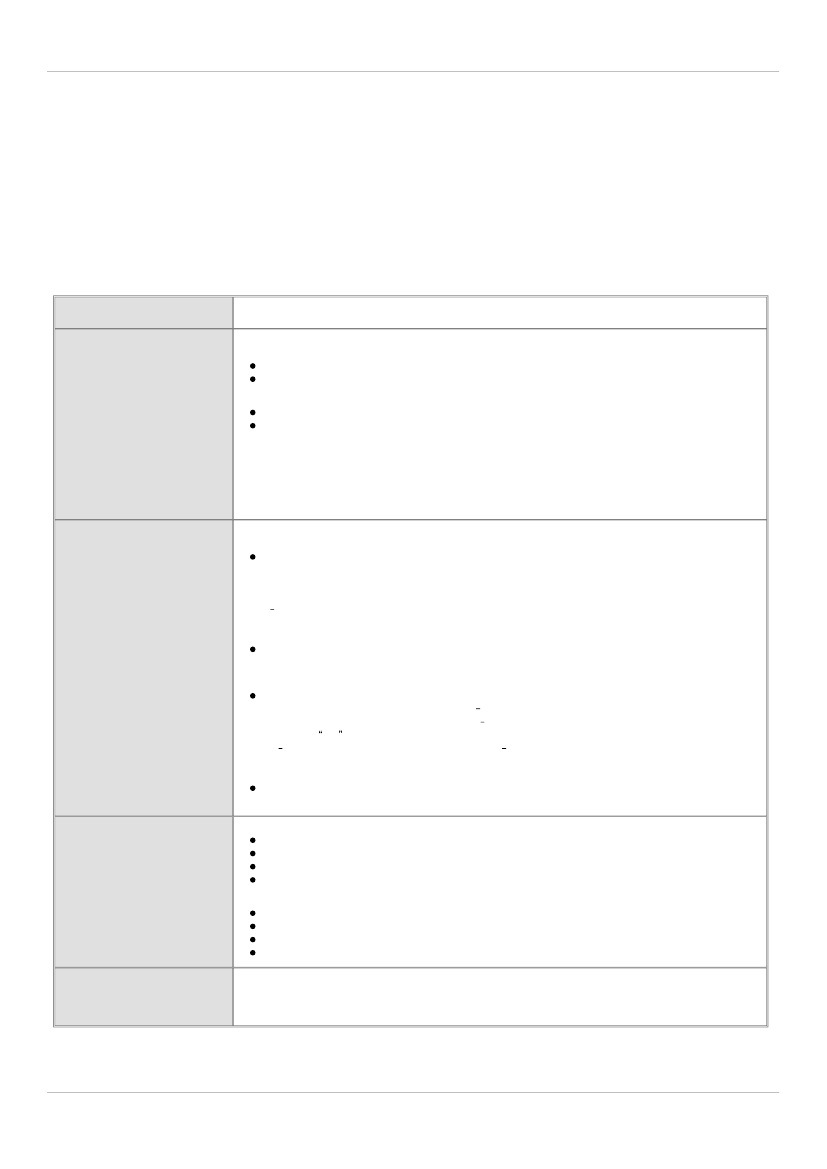
Characteristics of studies
Characteristics of included studies
Ahiskalioglu 2018
Methods
Participants
Study design:
Randomized controlled trial
Study grouping:
Parallel group
Baseline Characteristics
Intervention 1
Age:
79 ± 2.90 years
Duration of surgey:
28.69 ± 6.17 min
kontrol 1
Age:
5 ± 3.31 years
Duration of surgey:
28.82 ± 5.56 min
Included criteria:
The study included a total of 140 ASA I-II children aged between 5and 12 years old who underwent
elective phimosis and circumcisionsurgery
Excluded criteria:
Children with severe systemic disease, previous neuro-logical or spinal disorder, coagulation anomaly,
allergy against local an-esthetics, local infection at blocksite or witha history of premature birthwere excluded from the study
Pretreatment:
There were no significant differences between the two groups interms of age, height, weight, ASA class,
and duration of operation
Interventions
Intervention Characteristics
Intervention 1
Description:
Caudal block was performed by ultrasound guided in Group U. Aftersterilization of the region and USG
with sterile plastic cover and gel, thesacral hiatus was visualized at the level of the sacral cornus at the out of plane
via the lineer transducer of Esaote MyLab30 (Florence, Italy) ul-trasound machineat18 MHz depth and gain was
adjusted tooptimal vi-sual quality (Fig. 2). When the inserted needle reached the center of theultrasound image, a
20 22 gauge caudal needle (Epican® Paed caudalB·Braun Melsungen AG) was inserted at the transverse view using
theout-of-plane technique (Fig. 3). After confirming the absence of anyblood or cerebrospinalfluid in the aspiration,
the caudal solution calcu-lated as0.5 ml/kg wasinjected with hemodynamic and ECG monitoring.
Dose:
Caudal solution was prepared as 0.125% levobupivacaine(Chirocaine 50 mg/10 ml ampule, Nycomed Pharma
AS, Norway) plus10 mcg/kg morphine (total volume: 0.5 ml/kg), and was administeredto both groups.
kontrol 1
Description:
Caudal block was performed in Group C by conventional method.The sacral cornus and the sacral hiatus
were palpated. After sterilizationof the region, a 20 22 gauge caudal needle (Epican® Paed caudalB·Braun
Melsungen AG) was inserted into the skin with a 60 80 degreeangle and until the sacrococcygeal ligament was
passed with a pop feeling (puncture of the sacrococcygeal ligament). Then, the angle oftheneedle wasreduced
to20 30 degrees and inserted further for an ad-ditional 2 3 mm, entering into the sacral canal. After confirming the
ab-sence of any blood or cerebrospinalfluid in the aspiration, the caudalsolution calculated as 0.5 ml/kg was injected
with hemodynamic andECG monitorin
Dose:
Caudal solution was prepared as 0.125% levobupivacaine(Chirocaine 50 mg/10 ml ampule, Nycomed Pharma
AS, Norway) plus10 mcg/kg morphine (total volume: 0.5 ml/kg), and was administeredto both groups.
Outcomes
Serious adverse events
Outcome type:
DichotomousOutcome
Reporting:
Fully reported
Direction:
Lower is better
Data value:
Endpoint
Adverse events
Outcome type:
DichotomousOutcome
Reporting:
Fully reported
Direction:
Lower is better
Data value:
Endpoint
Notes
One hundred-thirty four children, American Society of Anesthesiologists I-II, between the ages of 5 and 12, scheduled for
elective phimosis and circumcision surgery
Risk of bias table
Review Manager 5.3
1