Udvalget for Fødevarer, Landbrug og Fiskeri 2011-12
FLF Alm.del Bilag 287
Offentligt
1
ContentExecutive Summary ............................................................................................................................. 3Foreword .............................................................................................................................................. 4Acknowledgements .............................................................................................................................. 5Introduction .......................................................................................................................................... 61. Opening of the conference / welcoming address ............................................................................. 72. Setting the scene – challenges and opportunities ............................................................................. 73. The antimicrobial resistance threat (MRSA, ESBL, CPE) .............................................................. 84. Best Practices ................................................................................................................................... 95. Antimicrobial resistance – ............................................................................................................. 10Socio-economic and health consequences ......................................................................................... 106. Workshops ..................................................................................................................................... 11Workshop 1 – Stop the overuse of antimicrobials in both humans and animals – Rational use 11Workshop 2 – Reduce the use of Critically Important Antimicrobials in humans and animals 12Workshop 3 – Data collection and surveillance of antimicrobial resistance and antimicrobialconsumption in humans and animals ......................................................................................... 127. Presentation of main points from workshop discussions ............................................................... 138. Closing of the conference .............................................................................................................. 14Annex I – Workshop 1 material ......................................................................................................... 15Annex II – Workshop 2 material........................................................................................................ 20Annex III – Workshop 3 material ...................................................................................................... 24Annex IV – Notes from workshop discussions .................................................................................. 33Annex V – List of participants ........................................................................................................... 42
2
Executive SummaryIn Europe and globally resistance towards lifesaving antimicrobials is a growing problem. Theincreasing development of resistance against antimicrobials is a major threat to human and animalhealth as it is the cause of significant morbidity and mortality in Europe and in the rest of the world.It results in immense costs for the society in many ways.The Danish Presidency finds it worrying that more than 25,000 EU citizens die each year due toinfections caused by resistant bacteria, and that still more bacteria continue to develop resistance.Existing antimicrobials are currently losing their efficiency and the development of new effectiveantimicrobials is not keeping pace with the development of the resistant bacteria.Antimicrobial treatment is an essential basis for both our health and our medical progress, andantimicrobials are indispensable when treating different diseases such as pneumonia and bacterialabdominal infections, and in connection with major surgery. If antimicrobials lose their effect, welose a fundamental basis for modern society.To combat antimicrobial resistance (AMR) immediate action is needed, and the conference held inCopenhagen 14 – 15 March 2012 has sought to inspire to such action.The conference included plenary sessions and workshops, each addressing the challenges ofantimicrobial resistance and possible means of tackling the microbial threat through reviews andoverviews, the exchange of best practices and subsequent debates on possible solutions.The ideas presented at the conference have contributed to the drafting of Council conclusions whichwill be presented for adoption by the ministers of health at the meeting of the Employment, SocialPolicy, Health and Consumer Affairs Council (EPCSO) on 22 June 2012.
“Actionis the real measure of intelligence.”Napoleon Hill (Author, 1883-1970)
3
ForewordA matter of life or deathAntimicrobials have saved millions of human lives since the 1940sand are successfully used inmany health related areas for both humans and animals. The use of antimicrobials has become anintegrated precondition for modern life to such a degree that most people do not spare it a thought.But the very use of antibiotics includes the potential for bacteria to develop resistance. The moreantimicrobials we use – the more resistant bacteria we get. And this is exactly what is happeningbefore our very eyes. More than 25,000 European citizens die each year due to infections involvingresistant bacteria.It goes without saying that we need to take action in order to stop the development of antimicrobialresistance. We need joint action across sectors and across borders. We need to focus on prudent andrestricted use of antimicrobials; we need to save critically important antimicrobials for specificuses; and we need everyone to be aware of the importance of this matter.We need joint action now and therefore the Danish Presidency has made it a key priority to focus onantimicrobial resistance, including organizing this conference where experts and officials have hadthe opportunity to discuss this important matter and to share knowledge and best practices.The conference generated many innovative and feasible ideas that we are pleased to present in thisreport.The ideas brought forth during the conference have contributed to the drafting of Councilconclusions which will be presented for adoption by the ministers of health at the meeting of theEmployment, Social Policy, Health and Consumer Affairs Council (EPCSO) on 22 June 2012.It is time for joint action – it is literally a matter of life or death!
Mette GjerskovMinister for Food, Agricultureand Fisheries
Astrid KragMinister for Health
4
AcknowledgementsThe conference was organised in close collaboration between the Danish Ministry of Health and theDanish Ministry of Food, Agriculture and Fisheries, including experts from the Danish Medicinesand Health Authority, Statens Serum Institut and the Danish Veterinary and Food Administrationand with assistance from experts from the Technical University of Denmark (DTU).The Danish Presidency of the Council of the EU would like to thank the European Commission,Directorate General Health and Consumers (DG SANCO), for co-financing the conference.In addition, we would like to thank the European Centre for Disease Prevention and Control(ECDC) for sponsoring the participation of members from relevant ECDC networks.
5
IntroductionOn 14- 15 March 2012, the DanishPresidency hosted the conference,CombatingAntimicrobial Resistance – Time for JointAction,which focused on the increasingglobal threat of antimicrobial resistance andthe use of antimicrobials from a „One Health‟perspective.The conference took place at the Bella Centrein Copenhagen and gathered approximately300 experts and civil servants from EUMember States, candidate countries and EEAcountries, the European Commission, EUagencies and other stakeholder organizationsand institutions.The conference moderator was journalist andClimate Director of Monday Morning, PerMeilstrup.The starting point for the discussions at theconference was that a holistic approachencompassing both human and veterinarymedicine is relevant because of the linksbetween disease in animals and health inhumans.In order to prevent further increase ofantimicrobial resistance we need to takeaction now, ensuring treatment for bothhumans and animals in the future.The main focus of the conference was todiscuss ways to:-Improve data collection andsurveillance of antimicrobial use andresistance for both animals andhumans throughout the EUStop overuse of antimicrobials inhumans and animals with focus on arational useReduce the use of critically importantantimicrobials in humans and animals
-
-
Based on these three main focus areas, theconference included plenary sessions andworkshops, which addressed the challenges ofantimicrobial resistance and possible meansof tackling the microbial threat throughreviews and overviews, the exchange of bestpractices and subsequent debates on possiblesolutions.The aim of the conference was to raiseawareness of the microbial threat andmotivate Member States and stakeholders toinstigate joint action.The following is the editorial reproduction ofthe conference.
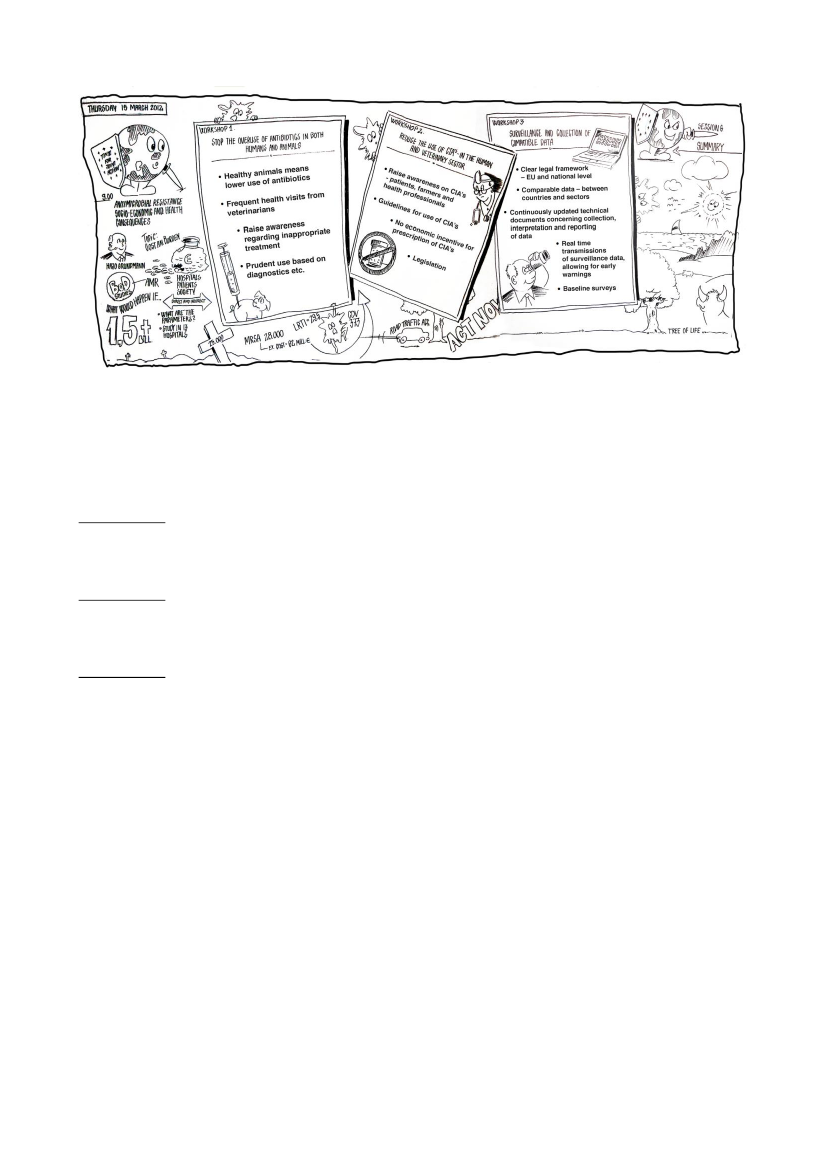
Visualizations of the conference by Jørn Nielsen, Creative Support
6
1. Opening of the conference / welcomingaddressHer Royal Highness Crown Princess Maryopened the conference by stressing that theproblem of antimicrobial resistance is a threatto the health and wellbeing of humans andanimals, and thus a matter of great concern.The continuous misuse and overuse ofantimicrobials are contributing to an increaseddevelopment of resistance to antimicrobialswhich every year leads to the death ofthousands of people. Her Royal Highnesswelcomed the conference and the focus on theescalating problem of antimicrobial resistance– underlining the necessity of focusing onprudent use and raising awareness of the needof limiting the use of certain antimicrobials todire cases.The Danish Minister for Food, Agricultureand Fisheries, Mette Gjerskov, and the actingDanish Minister for Health, Pia Olsen Dyhr,welcomed the participants to the conference.They emphasized the problem ofantimicrobial resistance and the need forfeasible solutions.Minister Gjerskov pointed out thatantimicrobial resistance is a serious problemin both the human health sector and theagricultural sector, and that we therefore mustlook to both sectors for solutions using the
„One Health‟ approach. This calls for us tocommunicate, share and cooperate and it iscrucial that everyone contributes withknowledge from their specific area ofexpertise. Minister Gjerskov urged everyoneto talk, share and learn from one another andlast but not least to take joint action.Acting minister Olsen Dyhr highlighted theaim of the conference, i.e. to raise furtherawareness of AMR and to create a forum forEU Member States and EU institutions todiscuss durable action-oriented solutions. Forthis purpose three workshops had beenorganised, each dealing with one of thespecific focus areas of the conference, whichwould give participants an opportunity toexchange thoughts and ideas on possibleactions for implementation at national and/orEuropean level.Following the ministers, there was a video-address by Mr. John Dalli, Commissioner forHealth and Consumer Policy, followed by apresentation by Dr. Martin Seychell, DeputyDirector-General. DG SANCO, EuropeanCommission. Both speakers underlined theseriousness of antimicrobial resistance andelaborated on the Commission‟s focus in thefield, especially the Commission‟s five yearAction Plan on antimicrobial resistance,which was launched in November 2011.
2. Setting the scene – challenges andopportunitiesDr. Margaret Chan, Director-General of theWorld Health Organisation (WHO) presentedan overview of the global problem ofantimicrobial resistance. Worldwide largerquantities of antibiotics are used in healthyanimals than in unhealthy humans and this iscause for great concern.
Dr. Chan emphasized how the EU andindividual countries can and have contributedto finding solutions to address the problem ofantimicrobial resistance. Dr. Chan highlightedsurveillance as a significant tool, andacknowledged the remarkable ways that theEU has moved forward, as reflected in severalnetworks for surveillance, not least the workof the European Centre for DiseasePrevention and Control (ECDC) in so quickly7
conducting risk assessments of the spread ofNDM-1 producing bacteria within Europe.Furthermore Dr. Chan acknowledgedmeasures taken by both Denmark and otherEU countries in achieving low domesticantibiotic consumptionReferring in particular to the EUCommissions 5-year action plan, Dr. Chanstressed that the EU is seeking solutionswhich include actions in line with those inthe WHO‟s European strategic action plan onAMR, launched last year.Dr. Marc Sprenger, Director of the ECDCgave a presentation on European challengeson antimicrobial resistance from a „OneHealth‟ perspective.Antimicrobial resistance is a threat to patientsafety due to limited options for treatment,thus resulting in increased duration of hospital
stays, patient morbidity and mortality, and Dr.Sprenger emphasised that each year, 25 000deaths in EU countries are directlyattributable to multidrug-resistant infections.Dr. Sprenger stressed the importance of aprudent use of antibiotics and underlined thateveryone is responsible with a reference toboth human and veterinary medicine and the„One Health‟ perspective.It was underlined that awareness is important,and in this context the European AntibioticAwareness Day, November 18, washighlighted.Dr. Sprenger concluded with three focalpoints essential to tackling the AMRchallenges:- Prudent use of antimicrobials- Infection control- New antibiotics
3. The antimicrobial resistance threat(MRSA, ESBL, CPE)1Jan Kluytmans, Professor in Microbiologyand Infection Control at the Amphia hospital,Breda, Netherlands, provided an overview ofthe microbial threat with emphasis on thehuman problem of MRSA and ESBL,including the zoonotic aspect. Under theheadline „MRSA and ESBL – A tale ofhumans, animals and antibiotics‟ ProfessorJan Kluytmans gave us an overview of thecurrent situation in Europe regardingantimicrobial use and antimicrobialresistance, specifying that most antibiotics areused in animals and that most animals thatreceive antibiotics are healthy. And this thenleads to consequences; MRSA and ESBL.1
Professor Kluytmans elaborated on MRSA,including livestock associated MRSA, whichmay be adapting to humans, and ESBL, whichis increasing everywhere, and concluded byencouraging participants to take home themessage of the need for a „One Health‟approach.Timothy Walsh, Professor in MedicalMicrobiology and Infectious Diseases at theCardiff University School of Medicine, theUK, spoke specifically about the globalemergence of Carbapenemases, including thedistribution of NDM-12that has greatpotential of becoming a worldwide publichealth problem.
Methicillin-resistantStaphylococcus aureus(MRSA),Extended-spectrum beta-lactamase (ESBL), Carbapenemase-producing Enterobacteriaceae (CPE)
2
New Delhi metallo-β-lactamase-1 (NDM-1)
8
With reference to a new WHO publication(2012) "The evolving threat of antimicrobialresistance - Options for action", ProfessorWalsh highlighted the need for- Surveillance of antimicrobial resistance anduse- Rational antimicrobial use and regulation,- Focus on antimicrobial use in animalhusbandry- Infection prevention and control- Fostering innovations, and- Political commitment.4. Best PracticesThis session was aimed at inspiring topossible actions through presentations on bestpractices from different Member States andsectors.The session was opened by Dr Niels Frimodt-Møller, Professor and MD at Department ofClinical Microbiology at Hvidovre Hospital,Denmark, who presented different initiativestaken in the health care sector to reduceantimicrobial resistance in Denmark and inthe EU. These included:• Implementation of prudent userecommendations and initiatives inmost EU Member States and severalthird-countries•Major advances in the understandingand awareness of the antibioticresistance threat among governments,health care professionals and thegeneral publicSuccess in significantly reducingantibiotic consumption throughcampaigns and interventions
Furthermore it was pointed out that if we areto tackle AMR in a comprehensive manner,environmental aspects also needs to beconsidered.Professor Walsh concluded by stressing thatinitiatives must be global, transparency mustbe mandatory and as money is an issue,perhaps global funds should be used forsurveillance on AMR. Coordinatedinternational surveillance is desperatelyneeded.
in the UK, presented the British experienceswith management of MRSA. This included areview of the national intervention strategiesfor England, Northern Ireland, Scotland andWales for managing and reducing healthcareassociated infections.The UK National Health Service hassuccessfully reduced meticillin-resistant Staphylococcus aureus (MRSA)bloodstream infections, and Dr. Hopkinsconcluded that health policy may contributeto reduce HCAI. In the future studies will beconducted to assess the impact of nationalinterventions.Frank Møller Aarestrup, Professor andresearch manager at the Division forEpidemiology and Microbial Genomics, theNational Food Institute at the TechnicalUniversity of Denmark, continued the sessionby giving a presentation on the Danishexperiences on applying surveillance data andmonitoring to reduce the use ofantimicrobials.Professor Aarestrup spoke of Danish actionstaken to reduce consumption in animals andhumans since the mid 1990‟s, and underlinedthat effective actions have included elementssuch as non profit, restrictions and controlmeasures based on monitoring ofconsumption.9
•
Dr. Susan Hopkins from the UCL Division ofinfection and Immunity, HCAI3and AMRDepartment at the Health Protection Agency3
Healthcare Associated Infections
Professor Aarestrup specified that futureactions should include focus on targeting theworst antimicrobials, preventing diseases andalways combining surveillance with choseninterventions.Vincent Jarlier, Professor in Microbiologyand Infection Control at the Pitie-Salpetrierehospital, France, presented the Frenchexperiences with successfully decreasing anumber of infections concerning ESBL andMRSA.To close the session, Nicolaj Nørgaard,Director of the Pig Research Centre (VSP),
Agriculture and Food Council, Denmark,presented the voluntary efforts made by theDanish agriculture industry, for instance thevoluntary ban on use of Cephalosporins fromJuly 2010 with the aim of reducing potentialrisk of resistance in human pathogens.Mr Nørgaard stated that the reduced use ofantimicrobials has not had impact on theDanish position in the pork market and hasonly had minor impact on productivity andeconomics. Furthermore „the yellow card‟scheme and the awareness of AMR of theDanish pig producers have had great effect inreducing consumption of Antimicrobials.
Visualizations of the conference by Jørn Nielsen, Creative Support
5. Antimicrobial resistance –Socio-economic and health consequencesHajo Grundmann, Professor at the Centre forInfectious Disease Epidemiology, NationalInstitute for Public Health, the Netherlands,started the second day of the conference bygiving a presentation on the socio-economicand health consequences of antimicrobialresistance, under the headline “cost andburden of antibiotic resistance: Thepopulation attributable fraction in Europe”.Professor Grundmann gave a review of thedirect and indirect costs compared to theperspectives; hospital, patient and society.
Professor Grundmann concluded by stressing,among other things, that:- No studies have so far addressed cost andburden from all relevant perspectives.- Current figures from the ECDC are based onmultiple assumptions.- Most studies determine risk estimates forsingle pathogens/infections in single centresand do not provide population-basedestimates.In conclusion, Professor Grundmann foundthat additional studies are required to providea more comprehensive estimate of the socio-economic impacts of AMR; studies includingmore pathogens and more infections.
10
Visualizations of the conference by Jørn Nielsen, Creative Support
6. WorkshopsOn the second day of the conference threeworkshops were conducted:Workshop 1: Stop the overuse ofantimicrobials in both humans and animals –Rational useWorkshop 2: Reduce the use of criticallyimportant antimicrobials in humans andanimalsWorkshop 3: Data collection and surveillanceof antimicrobial resistance and antimicrobialconsumption in humans and animalsTo guide the discussions material had beenprepared and distributed prior to theworkshop sessions, see annex I-III. Thematerial included a short introduction to thesubject, background information andquestions, concerning both the human healthsector and the veterinary sector, to facilitatethe workshop table discussions.Workshop 1–Stop the overuse ofantimicrobials in both humans and animals –Rational useThe workshop was chaired by JørgenSchlundt, DVM, Ph.D, and Director of the
National Food Institute at the TechnicalUniversity of Denmark, who also acted asrapporteur.There were approximately 85 participants inthe workshop.Introductory presentations were given byDominique Monnet, Senior Expert, theEuropean Centre for Disease Prevention andControl (ECDC) and by Annette ClevelandNielsen, Ph.D., Chief Veterinary Advisor, theDanish Veterinary and Food Administration(DVFA), on how to stop the overuse ofantimicrobials in humans and animals,respectively, with a focus on rational use andactions which have shown effectiveness.The introductory presentations were followedby table discussion in groups consisting ofapproximately 10 participants. The mainquestion for the discussion was: How can wereduce overuse of antimicrobials and ensureprudent use in both humans and animals?After the table discussions, the groupspresented the main points of their discussionsin workshop plenary.
11
Workshop 2– Reduce the use of CriticallyImportant Antimicrobials in humans andanimalsThe workshop was chaired by Kåre Mølbak,Ph.D., Department Director atEpidemiological Surveillance, the NationalInstitute for Health Data and Disease Control,Denmark, who also acted as rapporteur.There were approximately 55 participants inthis workshop.Introductory presentations were given byChristina Greko, Ph.D. and AssociateProfessor from the department of AnimalHealth and Antimicrobial Strategies, theNational Veterinary Institute, Sweden, onreducing the use of critically importantantimicrobials – veterinary medicine, and byJenny Dahl Knudsen, Senior HospitalPhysician, MD, Dr.M.Sci., Department ofClinical Microbiology, CopenhagenUniversity Hospital, Denmark, speaking onantimicrobial treatments with a minimum riskof resistance – and critical importantantimicrobials.The introductory presentations were followedby table discussion in groups ofapproximately 10 participants. The mainquestion for the discussion was: What are thepossible options for reduction and control ofthe use of critically important antimicrobialsin the human and the veterinary field?After the table discussions, the groupspresented the main points of their discussionsin workshop plenary.
Workshop 3– Data collection andsurveillance of antimicrobial resistance andantimicrobial consumption in humans andanimalsThe workshop was co-chaired by ProfessorFrank Møller Aarestrup and Robert Skov,MD, Head of Bacteriologic Surveillance andInfection Control, the National Institute forHealth Data and Disease Control, Denmark.Robert Skov also acted as rapporteur.There were approximately 120 participants inthis workshop. The workshop was dividedinto two main groups; so that approximately30 persons discussed surveillance onconsumption and approximately 90 personsdiscussed the surveillance on resistanceIntroductory presentations were given byHerman Goossens, Professor of Microbiologyat the University of Antwerp and Director ofthe Department of Clinical Pathology of theUniversity Hospital, Belgium, and by KariGrave, Professor and coordinator of theESVAC project at the European MedicinesAgency.Both presentations concerned consumption ofantimicrobial agents, as the resistance threathad been presented the day before.The introductory presentations were followedby table discussions in groups ofapproximately 10 participants. The mainquestion for the discussion was: How can westrengthen surveillance and improve datacollection throughout the EU?After the table discussions, the groupspresented the main points of their discussionsin workshop plenary, cf. annex III.
12
7. Presentation of main points fromworkshop discussionsThe main points from each workshop plenarysession were presented in conference plenaryby each workshop rapporteur in turn.The following summarize the main pointsfrom the three workshop discussions and donot necessarily represent a common viewshared by all participants but seek to reflectthe scope of the discussions.
See annex IV for the notes from workshopdiscussions.
Workshop 1 –Stop the overuse of antimicrobials in both humans and animals – Rational useHealthy animal production systems means reduced need for antimicrobialsStrengthen veterinarians position:- Increase importance of consultancy role and preventive role of veterinarian- Mandatory regular health visits from veterinarians- Veterinarians income based on health consulting work, not from sale of antimicrobialsGood examples promoting prudent use of antimicrobials in humans in EU Member StatesDevelop and strengthen guidelines at national level: in hospitals, primary health care sector,long term care institutions and at herd level of food production animalsNational legislation and enforcement to prevent Over the Counter sales of antimicrobialsRaise awareness of inappropriate treatment and sales without prescriptions
Workshop 2 –Reduce the use of critically important antimicrobials in humans and animalsThe need to educate and raise awareness: patients, farmers, health professionalsGuidelines are needed!- Common European, but adapted to local situations- Avoid off-label use of critically important antimicrobialsLegislation- For example ban of 3rd and 4th generation cephalosporins for food production animals- Analyse consequences and possibilities of enforcement- EU regulation will be important to support initiatives at Member State-levelThere should be no economic incentive of prescribing critically important antimicrobials forboth veterinarians and doctorsMonitoring of use, including indications for prescribing, via audits or supervisionImportance of microbiological surveillance, standard methods, building laboratory capacity
13
Workshop 3 –Data collection and surveillance of antimicrobial resistance and antimicrobialconsumption in humans and animalsClear legal framework(with existing frameworks EFSA/EMA/ESVAC/ECDC /EARS-Net/ESAC-Net)--EU levelNational level
Continuously updated technical documents (for consumption/resistance/human/veterinarian)- Clear definitions- Data collection/interpretation and ReportingComparable data- Between countries- Within SectorsReal time Reporting- Surveillance data- Early warning (use of existing frameworks)Baseline surveys- Some by point prevalence – some repeatedly•Selected pathogens•Indicator bacteria from Normal flora•Use the existing EFSA modelObstacles- Risk of blame- Financial constrains
8. Closing of the conferenceThe Danish Minister for Food, Agricultureand Fisheries Mette Gjerskov closed theconference and stressed the need for a jointeffort to tackle the problem of antimicrobialresistance.Minister Gjerskov highlighted thecommitment of the Danish Presidency tocombating antimicrobial resistance
Addressing the challenges of antimicrobialresistance – taking actions at EU level as wellas Member State level – is of paramountimportance in order to ensure effectiveantimicrobials in the future.On behalf of the Danish Presidency MinisterGjerskov warmly thanked the participants andspeakers for participating in the Conferenceand ensuring fruitful discussions and ideas forfuture actions.
14
Annex I– Workshop 1 material
Workshop 1Stop the overuse of antimicrobials in both humans and animals – Rational use1. IntroductionTreatment with antimicrobials is in many cases essential for human and animal health, but overuseof antimicrobials can lead to antimicrobial resistance (AMR) resulting in lost efficacy of treatmentand thereby complicate disease or even lead to death.Because some types of antimicrobial resistance can be transferred between bacteria, thedevelopment of antimicrobial resistance in any kind of bacteria may constitute a problem.In the EU an estimated number of 25,000 people die each year due to infections involving resistantbacteria with extra costs of 1.5 billion Euros yearly due to increased healthcare expenses andproductivity losses4.There is a need to agree on risk management interventions regarding overuse of antimicrobials inboth the human and animal sector.Overuse can be defined as unnecessary use of antimicrobials such as:for infections not caused by bacteria, orfor bacterial infections curable without antimicrobials, orunnecessary prophylactic/preventive use of antimicrobials
Overuse often arises from:Lack of proper diagnosis, for instance treating viral infections with antimicrobials or treatingwith a less or non-efficacious antimicrobial due to lack of diagnosis of the disease andbacteria involved.Non-prudent use and not following dosage and treatment period.Flock medication (water or feed) of animals in whole sections or stables thus inevitably alsotreating healthy animals.Preventive or prophylactic treatment of both animals and humans.Prescription of unnecessary broad spectrum antimicrobialsDoctors and veterinary practitioners relying on sales of antimicrobials for a significant partof their income.Lack of vaccination strategies, prevention strategies and infection control precautions inboth sectors.
4
http://ecdc.europa.eu/en/publications/Publications/0909_TER_the_Bacterial_Challange_Time_to_React.pdf
15
2. Basis for discussion2.1 Questions regarding the veterinary sectorHow is an incentive structure that will minimize continuous/preventive medication of flocks ofanimals created?Continuous antimicrobial treatment occurs probably because of lack of microbiological diagnosis orlack of preventive measures such as vaccination or hygienic precautions (all-in all-out productionetc.).Diagnostic testing:- How do you ensure justification for choosing either flock or individual treatment by currentdiagnostic testing and epidemiological descriptive data (mortality rate etc.)?Reducing the number of treated animals without jeopardizing animal welfare:- Establishing legislation on the period of validity of a prescription following a vetconsultation?- No flock medication in whole sections/stables, but only to separated diseased animals?Reducing the need for treatment and giving the best animal treatment with respect to humanhealth concerns:- By an incentive structure favouring vaccination strategies for instance by price regulation?- By vet advice on preventive management strategies (AI/AO, use of sick pens, alternatives toantimicrobial treatment etc.)?- Establishing national animal species treatment guidelines for production animals and bestpractice manuals, knowledge groups etc.How are systems to decouple the vets prescription practices from profits from sales ofantimicrobials established?Antimicrobial overuse has been shown to be linked to a system that allows the veterinarian to makean income from selling antimicrobials.- Establishing a one to one relationship between farmer and vet?- Introducing minimum annual herd health consultations with focus on preventive veterinarystrategies?- Allow/enforce legislation on a realistic and increased payment of vet services?- Enforce legislation on separate charge for consultations and for medication, no profit fromsales and no return payment.- Which changes in the pharmacy structure will be needed, if the vet no longer sells medicine,but only prescribes it?16
What are the major obstacles to categorize herds with respect to antimicrobial consumption?Benchmarking of antimicrobial consumption at herd level has been used to decrease antimicrobialoveruse.- Can herd categorization relative to antimicrobial consumption be based on individualrecords from the veterinarian or is some sort of herd monitoring necessary?- Is herd categorization relative to antimicrobial consumption possible for all animal species(which species are most important)?2.2 Questions regarding the human sectorHow can prescriptions of antimicrobials be reduced by doctors in the primary healthcare sector?Auditing of primary care physicians has been shown to both reduce antimicrobial use and improveprudent use. Rapid diagnostic microbiology testing has also been shown to improve prudent use ofantimicrobials.- Implement regular auditing of antimicrobial use in primary health care?- Establish national guidelines for rational use of antimicrobials based on diagnostics?- Implement use of point of care laboratory tests (bedside tests) for use by generalpractitioners?- Introduce reimbursement as an instrument for reduction of antimicrobial use; “medical”taxes, e.g. pricing of antimicrobials, taxes on use of generics?- Educate and employ regional risk managers monitoring antimicrobial prescription activity ofGP‟s, with regular feedback and benchmarking?- Enforce education/best practice manuals of professionals and patients concerning treatmentof infectious diseases, especially which infections can be treated with antimicrobials, and howto dose?How can the use of antimicrobials in the healthcare sector be reduced?Overuse in hospitals, especially of broad-spectrum antimicrobials, has been shown to select forresistant bacteria that can spread among patients, i.e. cause hospital epidemics, which result inprolonged hospitals stay and increased mortality.- Update and implement national guidelines for antimicrobial therapy in the hospital sector?- Focus and prioritize rational use e.g. only after laboratory testing, and a prescribed course oftreatment should be re-evaluated by a specialist within 24/48 hours or as soon as the test resultis available?- Discuss relevance of campaigns; are campaigns cost effective in relation to reduction ofantimicrobial consumption?
17
Which instruments can be used to ensure that legislation on antimicrobials labelled “prescriptiononly” is followed?It has been shown that up to 15-20 % of antimicrobial use in some European countries is due toover-the-counter sales without prescription.- Which changes in the organisation of pharmacy structure or organisation are needed?(Centralised registration of pharmacies/pharmacists; Permits for pharmacies/pharmacistpositions/education of pharmacists)- Implement monitoring, quality assurance, auditing, control of pharmacy sales; control visits;reporting on sales with/without prescription?- Implement rules for the pharmaceutical industry‟s influence on pharmacy sales?
3. Background informationAs every use of antimicrobials gives rise to development of resistant bacteria, unnecessary overusegive rise to unnecessary loads of resistant bacteria, which threatens efficacy of treatment in bothhumans and animals and increased mortality rates in humans infected with resistant bacteria.Specifically patients infected with S. typhimurium resistant to ampicillin, chloramphenicol,streptomycin, sulfonamide and tetracycline were approximately 5 times more likely to die, whereaspatients infected with quinolone resistant S. typhimurium were approximately 10 times more likelyto die than the general population. It should be noted that patients infected with totally sensitive S.typhimurium are only 2 times more likely to die than the general population5. Studies have alsoindicated that the use of antimicrobials for food animals is a major contributing factor for theselection and dissemination of resistantSalmonella6and recently the increasing use ofantimicrobials,particularly fluoroquinolones, in humanshas been shown to be associated with anincrease in incidence of infections caused by drug-resistantSalmonella7.Present EU recommendationsHumansCouncil recommendations on prudent use and health care associated infections in the human sectorare part of the Community strategy against AMR8. Specific strategies such as strengthening thesurveillance systems, control implementation, preventive measures, education etc. have beenreported from 18 Member States (MS) and 6 MS are preparing such strategies. Councilrecommendations from June 2009 aim at strategies and specific proposals to improve patient safetyin healthcare systems9.
5
Helms M, Vastrup P, Gerner-Smidt P, Mølbak K. Ugeskrift for Laeger. 2003 Jan 13;165(3):235-9); Helms M, Vastrup P, Gerner-Smidt P, Mølbak K., Emerg Infect Dis. 2002 May; 8(5):490-5 Excess mortality associated with antimicrobial drug-resistantSalmonella typhimurium.; Helms M, Simonsen J, Molbak K., J Infect Dis. 2004 Nov 1;190(9):1652-4. Epub 2004 Sep 21.6Emborg, H.D., Vigre, H., Jensen, V.F.et al.(2007). Tetracycline consumption and occurrence of tetracycline resistance inSalmonellatyphimurium phage types from Danish pigs. Microb. Drug Resist.; 13: 289-294.7Koningstein M, Simonsen J, Helms M, Mølbak K. (2010). The interaction between prior antimicrobial drug exposure and resistancein human Salmonella infections J Antimicrob Chemother, 17 May, doi:10.1093/jac/dkq1765Communication from the Commission of 20 June 2001 on a Community strategy against antimicrobial resistance (COM(2001) 333final, Volume 1 –not published in the Official Journal).9Council Recommendation of 9 June 2009 on patient safety including the prevention and control of healthcare-associated infections(OJ L 1541, 3.7.2009, p. 1)
18
AnimalsSince 2006 the EU has banned the use of antibiotic growth promoters (AGP) in feed and this shouldreduce the consumption of antimicrobials, if this is not compensated with an increase in therapeuticuse. Medicated feed is only available on prescription from a veterinarian and can only be producedin authorised and controlled premises10.MS medicine agencies adopted a strategic plan on antimicrobial usage11, which supports CVMP‟s12strategy on antimicrobials (AM). Currently the Commission has started a referral procedure on allquinolones and fluoroquinolones used for food producing animals, aiming at a prudent use of theseantibiotics in MS13.In applications for marketing authorisations of veterinary medical products for food-producingspecies, applicants are requested to address AMR issues and limitations to development of AMRwhen using the medical product14.Use of AM to controlSalmonellais prohibited in poultry (Commission Regulation (EC) No1177/2006) and other measures to controlSalmonellaare expected to reduce both Salmonellaprevalence and AMR strains, whereas control programmes forSalmonellain pigs andCampylobacterin poultry are lacking.
1011
Council Directive 90/167/eec (Medicated feed directive )Heads of Medicines Agency (HMA) Strategic Plan on antimicrobial issue, June 2010. In November 2011, HMA revised theStrategic Plan and adopted ”HMA Action Plan on antimicrobial issues12Committee for Medicinal Products for Veterinary Use (CVMP)13Link to EMA:www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/veterinary/referrals/Quinolones_containing_medicinal_products/vet_referral_000039.jsp&mid=WC0b01ac05800986a114International Cooperation on Harmonisation of Technical Requirements for Registration of Veterinary Medicinal Products;VICH GL27 (Antimicrobial Resistance: Pre-Approval), December 2003
19
Annex II– Workshop 2 material
Workshop 2Reduce the use of Critically Important Antimicrobials in humans and animals1. IntroductionCritically Important Antimicrobials (CIAs) have been defined first by the WHO for humans andlater by OIE for veterinary use. The primary parameter was scarcity of therapeutic alternatives fortreatment of serious diseases.In recent discussions three main classes have been identified as antimicrobials for which specialprecautions should be taken in order to maintain their efficacy for the future:1) Fluoroquinolones (widely used in both human and veterinary medicine)2) Cephalosporins (widely used in both human and veterinary medicine)3) Carbapenems (only authorised for human use)Antimicrobial resistance against the CIAs is particularly worrying, as they are “the last resort”treatment for a number of very serious diseases. A strictly prudent use of CIAs should therefore beagreed internationally as resistant bacteria can spread via global movements of persons, animals,and food products. The goal could be to reduce the use of CIAs to the lowest possible level whilemaintaining the option for necessary, lifesaving treatments.There is a need to agree on risk management interventions regarding the use of CIAs for humansand animals. A number of possible options and practises exist in individual EU member states, andthese have the potential to greatly affect the efficacy of CIAs for the future and may beimplemented without big public sector investments in databases, surveillance systems, etc.
2. Basis for discussions2.1 Conditions for use of CIAQ.1: Should there be certain conditions for use of CIAs?Statements for discussion:General conditions:CIAs should only be used for treatment of serious cases, which have responded poorly, orare expected to respond poorly, to other classes of antimicrobials.If CIA treatment is initiated due to serious health condition prior to the result of asusceptibility test, the treatment should be re-evaluated immediately after the test result isavailable, and amended if necessary.CIAs should only be used in combination with diagnostic/susceptibility tests.Duration of treatment should be limited to the minimum required time for cure of diseases.20
The use of products with combinations of active substances in situations where productswith a single active substance would be enough, unnecessarily increases selection pressurefor antibiotic resistance and should be avoided.Preventative use of CIAs (e.g. pre-surgery or metaphylactic treatment of patients/animals inthe incubation phase) should be minimised and always be carefully considered andpreserved for specific circumstances.Carbapenems should not be introduced into the veterinary field.Off label use of CIAs should be strongly discouraged.
Regarding use of CIAs in humans:CIAs should only be used in hospitals. Do CIAs have a role in general practise at all? This isin particular relevant for fluoroquinolones, which today at least in some countries are widelyused for treatment of uncomplicated urinary tract infections and for travel prophylaxis.Carbapenems should only be used in human therapy if the infection is caused (or in veryserious cases suspected to be caused) by multi-resistant bacteria.
Regarding use of CIAs in animals (Fluoroquinolones and 3rd and 4th generationcephalosporins):Fluoroquinolones should be used ONLY after a diagnostic/susceptibility test showing thatthere is no other treatment option.Fluoroquinolones should only be used in flock treatments when individual treatment is notpossible (e.g. poultry production) and only in serious incidents when no other option isavailable.3rd and 4th generation cephalosporins should be restricted to avoid preventative treatmentand flock treatment as far as possible.
2.2 Restricted use of CIA’s in human and animalsQ.2: Which actions should be taken to ensure restricted use of CIAs in humans and animals?Statements for discussion:Treatment guidelines for choice of correct antimicrobial for relevant diseases (and animalproduction forms) should be developed on national/international level, and implemented inall member states. The national guidelines should take internationally recognised code ofpractice of rational and prudent use of antimicrobials into account.The national guidelines should be communicated effectively to the prescribers.When authorising CIAs, doses should be selected considering AMR related risks. In case ofexisting products where data on dose selection are sparse, doses should be reviewed and incase they are too low (e.g. compared to other products containing the same active substance)this should be addressed by the competent authority.21
The competent authorities should ensure that distribution of antibiotics follow strict rulesand that no antibiotic can be bought without a prescription from a diagnosing doctor or vet.Doctors and vets should have no economic incentive to prescribe antibiotics, i.e. theirpayment should be related to diagnosing the clinical condition rather than to the prescriptionof antibiotics (neither amount nor frequency).Contracts between a doctor/vet/farmer and distributors/manufacturers of medicines shouldbe prohibited, i.e. no return-payment to influence the choice of/preference for certainproducts should be allowed.Advertisement of CIAs should not be directed to animal owners or patients.
2.3 Monitoring data and control measures to ensure a restricted use of CIA’sQ.3: Which basic monitoring data and control measures are necessary to ensure restricteduse/compliance with guidelines?Statements for discussion:In each country the use patterns of CIAs should be analysed via surveillance of data ofdoctors, vets, clinics, hospital sections and farmers (diagnosis and animal species).If CIA-use is above certain defined levels, the competent authority could inspect and adviceon options for reduction.For prescribers and users of CIAs (farmers, clinics and hospitals) a system of documentationand own check should be installed and this could be audited by a competent authority.The competent authority could have an inspection team that would visit farms, vets, etc toinvestigate correct use, documentation of medicine use, illegal medicine supply etc.Emergence of resistance to CIAs in pathogenic and indicator bacteria should be monitoredand the need for interventions should be continuously evaluated (The EuropeanCommission, EFSA, ECDC, Community Reference Laboratory, National ReferenceLaboratories and routine laboratories).
3. Background informationThe use of CIAs selects for resistance in bacteria in both humans and animals. The resistance isgenerated in both pathogenic bacteria and commensal bacteria of the normal flora. Several of theresistance mechanisms are transferable between bacterial species, thus leading to dissemination ofresistance especially in antibiotic containing environments. This may reduce the treatment optionsfor serious infections in humans and animals.Reports of increased resistance against CIAs in life-threatening bacterial diseases in humans haveemerged from many places in Europe. Most of the problems with resistance in human medicine arerelated to use of antimicrobials in humans, and must be managed by measures applied to the use ofantimicrobials in humans. However, resistance in zoonotic and other transferred bacteria may be aresult of the veterinary use of antimicrobials; hence there is a need for prudent use in veterinarymedicine as well.22
For animals, fluoroquinolones and some cephalosporins are also critically important, efficaciousand valuable antimicrobials to treat serious animal diseases. If such antimicrobials lose their activityor are no longer available for the treatment of animal diseases, antimicrobial therapy of somediseases will be complicated and may result in animal welfare and public health concerns, andeconomical losses.
23
Annex III– Workshop 3 material
Workshop 3Data collection and surveillance of antimicrobial resistance and antimicrobial consumptionin humans and animals
1. IntroductionThe aim of this workshop was to generate ideas and recommendations to improve data collectionand strengthen surveillance of antimicrobial consumption and antimicrobial resistance (AMR) inhumans and animals throughout the EU.Accurate and comparable data on antimicrobial consumption and resistance in both humans andanimals is an important prerequisite to visualize the extent of the problem of AMR and toimplement targeted measures to combat resistance. Such data will further provide the EU and theindividual Member States (MS) with fundamental tools to enable them to take concrete action tocombat antimicrobial resistance and to measure the effect of these actions.Organisations like the World Health Organisation (WHO), the Codex Alimentarius and the WorldOrganisation for Animal Health (OIE) have prepared guidelines on monitoring and surveillance ofantimicrobial consumption and AMR in humans, animals and food. These guidelines contain usefulinformation and advice on strategies and practical implementation.Several programs e.g. EARS-Net, EFSA, ESAC-Net and ESVAC are already running in Europewith the purpose of collecting accurate and comparable data from all MS. However, at present,participation by MS in most of these programs is voluntary and as a result, data are not reported byall MS. There is therefore a need for political initiatives to bring about the implementation of theseprograms in all MS.Furthermore, it is not certain that all the data from these programs are completely adequate orcomparable. The purpose of this workshop was therefore to discuss what constitutes optimalsurveillance and data collection and how this can be most easily and efficiently achieved by all MS.In addition, there is a need to determine how the results of surveillance can best be communicatedto relevant stakeholders so that they may be encouraged to take appropriate action to curtail orarrest the development of AMR.
2. Basis for discussions2.1 Surveillance and collection of comparable data on antimicrobial consumption in humansand animalsQ.1: What is the optimal level of surveillance of antimicrobial consumption?What is needed to optimize the present surveillance programs on consumption?What should the next level be and what are the obstacles to achieve this level?24
Veterinary medicine (ESVAC)- In regard to consumption data on farm level, animal species and age group?- In regard to antimicrobial sub groups/substances?- In regard to indications and/or diagnosis?Human medicine (ESAC)- With regard to continue the collecting overall sales data at package level?- With regard to the number of bed days an age group?- In regard to antimicrobial sub groups/substances?- In regard to information on indications and/or diagnosis?- In regard to human consumption data for the individual general practice and hospital(department level)?Should consumption of antimicrobial agents to companion animals be included insurveillance programs?Should consumption of antimicrobial agents for other purposes (e.g. plants) be included insurveillance programs
Q.2: How do we get all Member States included?How do we get all the Member States to collect data on consumption in the human and veterinaryfield and to not only provide these data to the ECDC, EFSA and EMA but also use them at anational level?What are the obstacles preventing collection and reporting of data to ESAC or ESVAC,respectively?What kind of tools and incentives would support a continuous EU wide surveillance ofantimicrobial consumption?Should the goal be commitments by MS or should surveillance and reporting be mandatoryfor Member States?
Q.3: How can we present data in a way to facilitate action?How should data be presented to stakeholders and the general public, both at a national level andinternationally, in order to visualize the situation and enable and facilitate action?To ensure the exchange of comparable data between Member States – should it bemandatory to report national data on consumption to ESAC and ESVAC, respectively?What are the prerequisites for comparing data on antimicrobial resistance and antimicrobialconsumption in real-time?How do we develop integrated surveillance and reporting of the data on consumption fromthe human and veterinary sector in order to facilitate an integrated approach?
25
2.2 Surveillance and collection of comparable data on antimicrobial resistance in humans andanimalsQ.1: What is the optimal level of surveillance of resistance?What is needed to optimize the present surveillance programs?What should the next level be and what are the obstacles to achieve this level?- In regard to resistance data on animal species, age group and bacteria species?- In regard to resistance data among bacteria isolated from community or hospitalacquired infections?- In regard to which antimicrobial agents that should be tested?- In regard to specific pathogens / resistance mechanisms (MRSA, ESBL, CPE, incl.NDM-1)- In regard to phenotype or genotype?- In regard to methodology (MIC, disk diffusion, clinical breakpoints/cut off values)Should antimicrobial resistance in companion animals be included in surveillance programs?
Q.2: How do we get all Member States included?How do we get all the Member States to collect data on antimicrobial resistance in the human andveterinary field and to not only provide these data to the ECDC and EFSA but also use them atnational level?What are the obstacles preventing collection and reporting of data?What kind of tools and incentives would support a continuous EU wide surveillance ofantimicrobial resistance?Should the goal be commitments by Member States or should surveillance and reporting bemandatory for Member States?
Q.3: How can we present data in a way to facilitate action?How should data be presented to stakeholders and the general public, both at a national level andinternationally, in order to visualize the situation and enable and facilitate action?To ensure the exchange of comparable data between Member States – should it bemandatory to report the data that are available?Should we establish an early warning and reaction system for specific resistancemechanisms?What are the prerequisites for comparing data on antimicrobial resistance and antimicrobialconsumption in real-time?How do we develop integrated surveillance and reporting of the data on AMR from thehuman and veterinary sector, respectively, in order to facilitate an integrated approach?26
3. Background informationIn the following please find a short status on each of the programs ESAC-Net, EARS-Net, EFSAand ESVAC.European Surveillance of Antimicrobial Consumption Network (ESAC-Net)Status on ESAC-Net prepared by Klaus Weist
The European Surveillance of Antimicrobial Consumption Network (ESAC-Net, formerly ESACproject) is a Europe-wide network of national surveillance systems, providing European referencedata on antimicrobial consumption. ESAC-Net collects and analyses data on antimicrobialconsumption from 28 EU and EEA/EFTA countries, both in the community and in the hospitalsector15.The coordination of ESAC-Net was transferred from the University of Antwerp, Belgium, to theEuropean Centre for Disease Prevention and Control (ECDC) in July 2011. ESAC-Net continues tocollect and analyse data from EU and EEA/EFTA countries, both in the community (primary care)and in the hospital sector, and thus provides independent, reference information on antimicrobialconsumption in Europe.The data sources for ESAC-Net are national sales and reimbursement data, including informationfrom national drug registers. The WHO Anatomical Therapeutic Chemical (ATC) classificationsystem is used for the allocation of antimicrobials into groups. Data on antimicrobial consumptionwill be collected at the product level for antibacterials for systemic use (ATC group J01),antimycotics for systemic use (ATC group J02), antimycobacterials (ATC group J04), and antiviralsfor systemic use (ATC group J05). In addition, data on a few other antimicrobials outside of ATCgroup J are also collected.The national networks upload their data to The European Surveillance System (TESSy) at ECDC ona yearly basis. The first data call for 2010 EU reference data was performed in January 2012. Afteruploading, each country approves its own data and the results are made available from the ECDCwebsite. Antimicrobial consumption data are expressed as a number of WHO Defined Daily Doses(DDD) per 1,000 inhabitants and per day. Complementary to this measurement unit, the number ofpackages per 1,000 inhabitants and per day is also reported depending on the availability of data onpackages. Since the ATC/DDD system cannot take into account changes in package content,information on packages is deemed to improve the understanding and interpretation of differencesin the levels and trends in antimicrobial consumption observed between and within countries. Forthe denominator, population data from EUROSTAT, or from national statistical reports, are used.When consumption data do not cover the whole population, countries provide data on thepopulation covered by antimicrobial consumption surveillance data.To maintain and facilitate data reporting, ECDC ensures:
15
http://ecdc.europa.eu/en/activities/surveillance/ESAC-Net/Pages
27
Validation of community and hospital sector data, analysis of the trends in antimicrobialconsumption overall and in the different ATC groups;Public access to information on antimicrobial consumption in Europe through an ESAC-Netinteractive database;Timely information and feedback to EU Member States and EEA/EFTA countries onindicators of antimicrobial consumption. These indicators provide a basis for monitoring theprogress of EU Member States and EEA/EFTA countries towards prudent use ofantimicrobials.
Cooperation of ESAC-Net and ECDC with the European Food Safety Agency (EFSA) and theEuropean Medicines Agency (EMA) on the integrated use and reporting of data on consumption ofand resistance to antimicrobial agents in humans, animals and food in the EU is currently underway.European Antimicrobial Resistance Surveillance Network (EARS-Net)Status on EARS-Net prepared by Ole Heuer and Liselotte Diaz Högberg
The European Antimicrobial Resistance Surveillance Network (EARS-Net) is a network of nationalsurveillance systems providing European reference data on antimicrobial resistance for publichealth purposes. EARS-Net is the largest publicly funded system for surveillance of antimicrobialresistance in Europe16. The coordination of EARS-Net was transferred from the Dutch NationalInstitute of Public Health and the Environment (RIVM) to the European Centre for DiseasePrevention and Control (ECDC) in January 2010.How are the data collected and processed?Antimicrobial susceptibility test results are collected by national surveillance networks from clinicallaboratories in the participating countries. At present, more than 900 public health laboratoriesserving over 1400 hospitals are providing data to EARS-Net. The participating hospitals andlaboratories provide services to an estimated population of 100 million European citizens.The national surveillance networks upload their data to The European Surveillance System (TESSy)at ECDC on a yearly basis. After uploading, each country approves its own data and the results aremade available from the ECDC website. In order to facilitate data reporting, ECDC provides:Validation of antimicrobial susceptibility data reported by the countries;Analysis of trends in the occurrence of antimicrobial resistance over time and betweendifferent countries and regions;External quality assessment (EQA) and protocols on testing methods to improve theconsistency and quality of the data.
Which surveillance data are collected?Since the network started in 1999, the participating laboratories have collected antimicrobialresistance data on approximately 500,000 invasive bacterial isolates. EARS-Net performssurveillance of antimicrobial susceptibility in seven bacterial pathogens of public healthimportance:16
28
Streptococcus pneumoniaeStaphylococcus aureusEnterococcus faecalisEnterococcus faeciumEscherichia coliKlebsiella pneumoniaePseudomonas aeruginosa
In addition, EARS-Net collects denominator data on laboratory/hospital activity.How are the data made available?EARS-Net results represent an important source of information on antimicrobial resistance forpolicy makers, scientists, doctors and the public. These results are made available through:TheEARS-Net interactive databaseproviding user friendly display of selected results invarious downloadable formats, such as tables, figures, and maps17TheEARS-Net annual reportswith interpretations and conclusions regarding trends in theoccurrence of antimicrobial resistance across Europe18,Scientific publications in peer review journals.
Monitoring of AMR in zoonotic and indicator bacteria from humans, animals and food in theEU (EFSA)Status on EFSA prepared by Pierre-Alexandre Beloeil and Pia Mäkelä
Bacterial resistance to antimicrobials occurring in food-producing animals can spread to people viafood-borne routes but also by environmental routes, such as surface water, and by direct animalcontact. The monitoring of antimicrobial resistance (AMR) in zoonotic and commensal bacteria inhumans, food-producing animal reservoirs and food thereof is a pre-requisite for the understandingof the development and dissemination of AMR and the identification of the emergence specificpatterns of resistance. Under the existing European Union (EU) legislation, Member States arerequired to establish monitoring systems of AMR in the major food-producing animal species(poultry, turkeys, pigs and cattle) and related meat. The AMR monitoring in zoonotic Salmonellaand Campylobacter is mandatory, while that in indicator commensal E. coli and enterococci is madeon a voluntary basis. The European Food Safety Authority (EFSA) has been assigned a key role incollecting the data reported by the EU Member States and in monitoring AMR in animals and foodat EU level.On a yearly basis, EFSA analyses the AMR data reported by Member States and publishes an EUSummary Report displaying an overview of the levels of resistance for the zoonotic Salmonella,Campylobacter, and indicator E. coli and enterococci, monitored in animal species and food at bothMember State and EU levels. AMR is interpreted using harmonised epidemiological cut-off values(ECOFFs) in order to early detect reduced susceptibility. Temporal trends in the occurrence ofresistance are also followed and analysed, to detect changes over time. Additionally, a move1718
http://ecdc.europa.eu/en/activities/surveillance/EARS-Net/database/Pages/database.aspxhttp://ecdc.europa.eu/en/activities/surveillance/EARS-Net/publications/Pages/documents.aspx
29
towards an integrated approach in the monitoring of resistance has started since 2009, whenresistance data from zoonotic Salmonella and Campylobacter collected and analysed by theEuropean Centre for Disease Prevention and Control (ECDC) from human cases of salmonellosisand campylobacteriosis have been included in the EU Summary Report, and an attempt made atjointly analysing them in conjunction with those deriving from animals and food.In order to enhance the comparability of data reported to EFSA, technical specifications on themonitoring and reporting of AMR in animals and food have been developed and published in 2007and 2008. These specifications cover the sampling strategies to be used for the selection of isolates,the methods for susceptibility testing, the panel of antibiotics to be used and also the criteria todefine resistance. As observed in the last reporting years, data transmitted to EFSA are now mostlyobtained through standardised dilution methods, and reporting of MIC distributions has madepossible to interpret the occurrence of resistance using both epidemiological cut-off values and,when a comparison with human data was made, clinical breakpoints used in human medicine.The main general findings conclusions of data collection and analyses at EU level are thatresistance to antimicrobials was commonly found in isolates from humans, animals and food,although disparities in the occurrences of resistance were frequently observed between MemberStates. High resistance levels were recorded to ampicillin, tetracyclines and sulphonamides inSalmonella isolates from human cases, while resistance to third-generation cephalosporins andfluoroquinolones, both critically important antimicrobial groups for human medicine, remained low.In Salmonella and indicator E. coli isolates from fowl, pigs, cattle and meat thereof, resistance totetracyclines, ampicillin and sulphonamides was also commonly found, while resistance to third-generation cephalosporins was low. Moderate to high levels of ciprofloxacin resistance wasobserved in Salmonella and indicator E. coli isolates from fowl, broiler meat and pigs. InCampylobacter isolates from human cases, resistance to ampicillin, ciprofloxacin, nalidixic acid andtetracyclines was high, while resistance to erythromycin, a critically important antimicrobial, wasrecorded at a low level. High resistance to ciprofloxacin, nalidixic acid and tetracyclines was alsoobserved in Campylobacter isolates from fowl, broiler meat, pigs and cattle, whereas erythromycinresistance was at lower levels. Among the indicator enterococci isolates from animals and food,resistance to tetracyclines and erythromycin was commonly detected.As a next step, EFSA is in the process of moving from the traditional reporting of aggregated datato isolate-based data, thus improving the level of granularity of the data submitted and the potentialanalyses that can be conducted. AMR isolate based data enable to analyse and report on the multi-resistance by investigating co-resistance patterns and identifying emerging new multi-resistancepatterns. Moreover, it is expected that the more detailed information that will become available withreporting at isolate level could be used to better characterise the occurrence of AMR in particulardefined animal populations so that this information could also be linked to antimicrobialconsumption data. In collaboration with European Medicine Agency (EMA), which is in charge ofmonitoring consumption of antimicrobials in animals, the intention is indeed to analyse therelationship between antimicrobial use and antimicrobial resistance in animals.
30
European Surveillance of Veterinary Antimicrobial Agents (ESVAC)Status on ESVAC prepared by Kari Grave, Jordi Torren & David Mackay
The European Surveillance of Veterinary Antimicrobial Consumption (ESVAC) project waslaunched by the European Medicines Agency in September 200919, following a request from theEuropean Commission to develop a harmonised approach for the collection and reporting of data onthe sales of antimicrobial agents in animals from the Member States (MSs). The major deliverablesto be delivered by the ESVAC project as described in the terms of references (TOR) from theCommission wereTo identify the existing data/surveillance systems established for collection of sales and useof antibacterial drugs in the Member StatesTo develop a harmonised approach for the collection and reporting of data based on nationalsales figures combined with estimations of usage in at least major groups of species(poultry, pigs, veal, other ruminants, pets and fish);To collect the data from Member States and manage the data base;To draft a summary annual report with the data from Member States.
An appendix to the terms of reference sets out the following intended uses for the collected data onusage of veterinary antimicrobial agents:To aid interpretation of patterns and trends regarding antibacterial resistanceTo serve as a basis for risk profiling and risk assessment regarding antibacterial drugresistance.To serve as a basis for setting risk-management priorities.To serve as a basis for evaluating the effectiveness of control measures being implemented.To aid in identifying emerging use of antibacterial drugs, e.g. of specific drug classes suchas critically important antibiotics.To aid in comparing usage of antibacterial drugs between and within countries, and betweentime periods, etc.To assess the spread and effects of environmental pollution through use of antibacterialdrugs.To serve as a basis for focused and targeted research and development.
In response to the TOR already existing data on the sales of veterinary antimicrobial agents fromthe 9 European countries (of which 8 were EU/EEA countries) that had already establishedsurveillance programs were collected and reported in a harmonised manner20. This included thedevelopment of a population correction unit (PCU) in order to normalize the annual sales figures ineach country by the animal demographics. PCU is the estimated weight at treatment of livestockand of slaughtered animals in the relevant year and serves as a proxy for the animal population.
19
European Medicines Agency, 2009 .European Surveillance of Veterinary Antimicrobial Consumption.(http://www.ema.europa.eu/ema/index.jsp?curl=pages/regulation/document_listing/document_listing_000302.jsp&murl=menus/regulations/regulations.jsp&mid=WC0b01ac0580153a00)20European Medicines Agency, 2011. Trends in the sales of veterinary antimicrobial agents in nineEuropean countries (2005-2009); EMA/238630/2011.(http://www.ema.europa.eu/docs/en_GB/document_library/Report/2011/09/WC500112309.pdf)
31
During the first part of the pilot phase (2010-2012) an ESVAC protocol and data collection form inorder to ensure standardized data were developed and tested together with experts from the MSs aswell as with three MSs collecting data on veterinary antimicrobials agents for the first time. Inparallel, the ESVAC data program for the logical validation of the data in terms of standardizationhas been developed and tested and the ESVAC data base is established.The ESVAC project has now collected harmonised and detailed data on sales of veterinaryantimicrobial agents at package level for 2010 by use of the ESVAC data collection from 19EU/EEA countries that volunteered to participate in the pilot study. Of these 17 are MSs, and thesales data from these represent a coverage of the major food animal species (cattle, pigs, poultry,sheep and goat) in the MSs close to 75 %. The data will be published the second half of 2012. It isexpected to increase the numbers of MSs providing data for 2011 by at least three countries. Incontrast to the aggregated data, the data collected according to the template will for example giveinformation on administration form such as premixes and differ between herd and individualtreatment; these data will allow for a more in-depth analysis of the sales of veterinary antimicrobialagents in the EU. However, in order to perform proper risk analysis data by species are required.It should be emphasised that many of the MSs are collecting the data for the first time and that it isgenerally acknowledged that it takes at least three years to establish a valid baseline; consequentlythe 2010 data should not be used alone as a basis for setting management priorities, but shouldalways be complemented by data from other sources.According the ESVAC project plan the collecting of data by animal species from the MSs will beimplemented in 2014. In order to prepare for this, an ad hoc working group consisting of expertsfrom the MSs has recently been nominated with the task to propose a model on how to establish asustainable surveillance program for the collection of standardized and representative data byspecies.Furthermore, in order to take into account the differences in the dosing and the number of treatmentdays for the veterinary antimicrobial agents when reporting the data by species an ad hoc workinggroup of experts from the MSs has been established and is asked to propose technical units ofmeasurement applicable for analysing surveillance data.
32
Annex IV –Notes from workshop discussionsThe contents of this annex summarises the workshop discussions and is a condensed list of the ideasthat were brought forward in connection with the group discussions. The ideas below do not reflecta common view shared by all participants.
Workshop 1The following questions were the basis of the discussions:1. How is an incentive structure that will minimize continuous/preventive medication of flocksof animals created?2. How are systems to decouple the veterinarians prescription practices from profits from salesof antimicrobials established?3. What are the major obstacles to categorize herds with respect to antimicrobial consumption?4. How can prescriptions of antimicrobials be reduced by doctors in the primary healthcaresector?5. How can the use of antimicrobials in the healthcare sector be reduced?6. Which instruments can be used to ensure that legislation on antimicrobials labeled“prescription only” is followed?General statementsAntibiotics in animal health should only be used in the context of biosecurity, good nutrition, goodhousing, herd health plans and vaccinations being in place.All sectors should work together.One way forward could be to expand the existing AMR-Working Group in the European-Commission on the veterinary side to include the human side. This would support the „One-Health‟approach, i.e. experts from each Member State, to enforce implementation of the Commissionsaction plan on AMR in the EU.Questions regarding the veterinary sectorHow is an incentive structure that will minimize continuous/preventive medication of flocks ofanimals created?Possible initiatives:Healthy animal production systems are needed. Healthy animals equal lower use ofantibioticPreventive treatment should be avoided; Metaphylaxis/flock medication should be reducedThere is a need for guidelines for the treatment in certain speciesTo reach the goal of responsible use a combination of data collections (on farm level), bestpractice guides and restriction policies are neededIncensement of the importance of consultancy role and preventive role of veterinarians33
Mandatory frequent health visit from vets should be encouraged. Veterinarians should basetheir income from health consulting work and not from sale of antibioticsEnsure the professional independency of the veterinarians
Obstacles:No or small economic incentive for producers to have better production systemsIn some countries farmers cannot access antibiotic drugs from pharmaciesThe veterinarians buy the drugs from the industry and store itA change in rules needs to be followed by change in logistics
How are systems to decouple the vets prescription practices from profits from sales ofantimicrobials established?Enforcement!Regular visits of veterinariansCooperation with the industry in the development of new drugs should be strengthen;Develop and strengthen national level guidelines for rational use of antimicrobials based ondiagnostics and develop fast track procedure for their adoptionAnother option: Important to have inspections and surveillance systems of veterinarians -not a requirement to decouple veterinarian prescription from economic incentives as long asyou have a good and very effective surveillance systems. (Different opinions around thetable!)
What are the major obstacles to categorize herds with respect to antimicrobial consumption?Obstacles:Reporting systems not reliableLack of political willingnessLack of good surveillance systems
Initiatives:Guidelines on how to start surveillance programmes should be encouragedThe systems should be usable for both veterinarians and farmers
Questions regarding the human health sectorHow can prescriptions of antimicrobials be reduced by doctors in the primary healthcare sector?Initiatives:Permanent Working Party standards and guidelines, NETHMAP, inspections (NL)Good examples are important for promoting prudent use in other EU countriesVisit different countries to get inspired by best practices34
Guidelines should be made for primary health sector and for the hospital sectorGuidelines should be set at EU level but with special parts for each MSLaboratory test (bed side) should be developed and used much more and be a part of theguidelinesReinforce and reorganise the curriculum of medical staff at university level to include AMRand infection prevention and control all along their coursesDevelop and strengthen at national level guidelines for rational use of antimicrobials basedon diagnostics and develop fast track procedure for their adaptationAuditing including considerations according to quality indicatorsIncentive systems to regulate antibiotic use by general practitionersBetter control of antibiotic use in the long term care institutions, which use a lot ofantibiotics. Infection control in long term care institutionsReinforce infection control – hand hygiene in primary care (children‟s institutions, schools,long term care institutions)
How can the use of antimicrobials in the healthcare sector be reduced?Focus on hygiene and prudent use to diminish transmissionReinforce prevention and control of infection in healthcare settingsThrough the European Antibiotic Awareness Day, reinforce and make it systematic toaddress communication and awareness among the healthcare professionals (in all healthcaresettings)
Which instruments can be used to ensure that legislation on antimicrobials labeled “prescriptiononly” is followed?Enforcement of national legislation to prevent over-the-counter sales of antibiotics!Raise awareness among the public about the problems of sales without prescriptions,including internet salesRaise awareness about the problems for the individual arising from inappropriate treatmentwith antibioticsEU-legislation against under-the-table sales; better enforcement of rules/finesEnforce prescription only sales of antibioticsGuidelines for practitionersTraining and education for pharmacistsSocio-economic-cultural factors explaining over the counter sales of antibiotics
Obstacles:Economic incentives for pharmacies to sell prescription drugs in some countries - antibioticscan then be sold illegallyNo enforcement of present laws. You only dispense what the doctor ordered
35
Workshop 2The following three questions were the basis of the discussions:1. Should there be certain conditions for use of CIAs?2. Which actions should be taken to ensure restricted use of CIAs in humans and animals?3. Which basic monitoring data and control measures are necessary to ensure restricteduse/compliance with guidelines?Framing the situationThe concept of CIAs is developing as resistance is increasingSecond line drugs (cephalosporins) are used as first line treatment, and colistin as the lastresort- Colistin/polymyxin needs to be includedIn some countries, little difference between practices in the primary health care system andin hospitals- Important to focus on primary health care with overuse of fluoroquinolones andcarbapenemsOften little microbiological supportThere should be certain conditions for the use of CIA‟s
Q 1: Should there be certain conditions for use of CIAs?CIA‟s should be used in combination with microbiological diagnosis and sensitivity testsAllowed for early empirical treatment of severe infections, expected to respond poorly toother classes of antimicrobialsIn animals: CIAs may be limited to few situations of acute illness- Carbapenems should not be used for animalsIn general practice: CIAs has a very limited role to playIn general, do not use CIAs as prophylaxis
ActionsNeed to educate and raise awareness- Patients, farmers, health professionalsGuidelines are needed!- European, but adapted to local situations- Avoid off-label use of CIAsLegislation may be necessary, e.g., ban of 3rd and 4th generation cephalosporins for foodanimals- Analyse consequences and possibilities of enforcement- EU regulation will be important to support initiatives at the MS level36
There should be no economic incentive of prescribing CIAs for both veterinarians andmedical doctors
ImplementationMonitoring of the use including indications to prescribe- Audits, supervision, ”yellow cards”Importance of microbiological surveillance, standard methods, support to build laboratorycapacity
Workshop 3The following questions were the basis of the discussion:1.2.3.4.5.6.What is the optimal level of surveillance of antimicrobial consumption?How do we get all Member States included (consumption)?How can we present data in a way to facilitate action (consumption)?What is the optimal level of surveillance of resistance?How do we get all Member States included (resistance)?How can we present data in a way to facilitate action (resistance)?
Q.1: What is the optimal level of surveillance of antimicrobial consumption?Need EU-standards for human consumption data collection and denominatorsAge groupIndications
Focus on the most critical firstConsumption data on animal species, age group, production type, sub groups/substancesshould be achievedIndication and/or diagnosis should be considered both as an animal health indicator and foractions at the national level; at this state not a high priority on the EU level
Q.2: How do we get all Member States included (consumption)?Need EU legislation for collecting data by animal speciesShould be harmonised legal basis for top-down surveillance; e.g. harmonised with ESVAClegislationMedia campaigns
Q.3: How can we present data in a way to facilitate action (consumption)?Need for a common legal basis on what to report to ESVAC. There must be free hand forthe countries on how system should be build37
Also national legal framework is necessary for collection in order to obtain harmonized dataon species level- National action plans
There should be a possibility for adoption to national structure:- Collection of all veterinary prescriptions- Recording of each prescription and indication- Recording public data base or- Recording privately on practice level
Data must be fully available for national reporting, and should be analyzed nationally;statistically relevant by the scientifically competent body/authority data should be reportedwith transparencyManagement actions are a national matter; possible actions for improvement of the datacollection systems should be identified (e.g. benchmarking of herds)Data quality – is all reported. Is medicated feed registered? And transport? It is necessary todescribe carefully the distributions systems and find methods to validateCapacity building: organizing meeting with countries that have extensive experience inbottom-up systems
Prerequisites for comparing data on resistance and consumptionData on consumption should be in harmonized with resistance data- That is as a minimum on species level, but for some species also on production typelevel, e.g. broilers vs. layers and in the future veal calves vs. dairy cattleIntegrated surveillance and reporting on data from human veterinary fieldIt is necessary to harmonize the measures, e.g. defining an equivalent to the DDD for theveterinary field; also harmonizing of the denominatorAlso, more than one measure is necessary for each field depending on the purpose of thecomparison, to facilitate correct interpretation
Q.4: What is the optimal level of surveillance of resistance?Need absolutely clear definitions and collection of quantitative dataHuman surveillance of resistance- Bacterial species to include (EARS-Net pathogens extended by: Acinetobacter,S.pyogenes, Haemophilus influenzae (invasive) gastro-enteritis pathogens(Salmonella, Campylobacter) and Helicobacter pylori- Hospitals, community, age groups (children), indications (LRTI, UTI, Blood, Skin andsoft tissue)38
- Denominators- Ad hoc screening of emerging resistances in healthy humans / groups at risk- Also monitoring in healthy humans also different syndromes/disease – hospitalenvironment- Phenotypic and genotypicAnimal surveillance of resistance- Animal/food isolation as close to the consumer as possible - Both food and pets- Indicators covering the whole line – vet – food – human – environment – set up fromVet/food could be implemented in human sector – E. coli/Enterococci – descriptionof the load of AMR from food to consumers- Stratification of monitoring animal species, production typesRisk based approach for identifying the most critical points for prioritizing the focus –especially for indicator organisms- What is the major hazard to humans (MRSA, CPE, and ESBL)?- Which kind of the animal/food production is most risky?- Where is the highest consumption?Recommendation 1:Suggest to EFSA to include E. coli as an additional pathogen that represent an important reservoirfor multiple resistance determinants.Recommendation 2:Carry out cross- sectional (human and animal) baseline and repeated surveys to representativelycollect isolates (E. coli) from both habitats and explore occurrence of AMR genes.Q.5: How do we get all Member States included (resistance)?High level of transparency – sharing of data – but this is difficult in daily life (especially inhuman sector)Important from the beginning to have a clear goal of a monitoring programming that includeagreement on dataflow and ownership (e.g. as the EU baseline studies)Need harmonizationMandatory to participate and reportLegislation should define the key elementAll partners need to see the benefitGood communicationGood IT-systems39
Financial constraints (AMR surveillance programme should at least for some countries besupported by: i.e. DG-SANCO grants)Expansion to other countries of current systemsAdaptation of current systems started before harmonisationPolice function or help when not compliant (Feedback on the results/report: what is theoutcome, what improvements can be achieved: gives motivation) – AVOID BLAMENeed for a stringent legislationLong term vision with funding (by EU or countries?)Commitments at all levels, EU, countries with prove of outcomeMedia campaigns
Q.6: How can we present data in a way to facilitate action (resistance)?Early warningEstablish a similar system as the rapid early system on food borne outbreaks. This is theultimate goalIn the beginning start on establishing expert groups in MS, who should look on data anddecide which actions to be taken. They should link up on ECDC, who should be those todecide in the endQuick publicationsCombine reporting of consumption data and resistanceCommon database needed. All MS needs an electronic database system for central datarecording. Data must be comparableGood IT-systemsTo obtain integrated surveillance we need a system to monitor the same bacteria on both thevet and human sidesThe focus must be based on known zoonoses and indicator-bacteria as a starting point. Onthe long term the choice of bacteria to monitor can be changeableResistance data should be presented with e.g. economical costs / outcome to speak louderfor politiciansTrends in resistance should be presented for each pathogenWe recommend to include the representatives of the each antimicrobial groups , dependingon bacterial speciesCombined reports for actions to tighten the cooperation between medical and veterinaryauthorities in each Member State
40
The existing EWRS reporting should be utilized (extend EWRS for AMR). The veterinaryand medical reference labs are expected to cooperate closely and regularly exchange AMR-data collected by their field-laboratoriesMedia campaigns
41
Annex V– List of participantsSurnameAndersonAndreasenAppelBarfodBay-SmidtBeechinorBjerrumBorgBoshevskaBuettnerBuhotBødkerCampos MarquésCarnwallCarruthChristensenClariciDasDe BoerDobbenburghDuque EscolarEdlundFirst nameJamesMargitBerndBoJanGabrielLarsMichaelGolubinkaSabinaChristopheTrineJoséMagnusRebaSophieAlexandraSaradaEllenO.A. (Rens)EvaCharlottaMinistry/institutionDanish Association of the PharmaceuticalIndustry/GlaxoSmithKlineDr.Pig Research Centre, Danish Agriculture and Food CouncilProf.Federal Institute for Risk AssessmentMrRADS, AmgrosMrFVMDr.Irish Medicines BoardProf.Copenhagen UniversityDr.Ministry of HealthDr.Institute of Public HealthDr.Federal Veterinary OfficeDr.FVEMrs/Ms Ministry of Food, Agriculture and FisheriesDr.Instituto de Salud Carlos IIIMrMinistry for Rural AffairsProf.Georgetown UniversityMrs/MsDr.Mrs/MsMrs/MsMrMrs/MsProf.The Danish Veterinary AssociationFederal Ministry of HealthStanding Committee of European Doctors (CPME)Ministry of Health, Welfare and SportAUVFEFACMedical Products AgencyTitleMrCountryWorkshopUnited Kingdom Workshop 1DenmarkGermanyDenmarkDenmarkIrelandDenmarkMaltaFYR MacedoniaSwitzerlandBelgiumDenmarkSpainSwedenUnited States ofAmericaDenmarkGermanyBelgiumNetherlandsNetherlandsBelgiumSwedenWorkshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 142
SurnameFodeFortineauFrimodt-MøllerFrimodt-møllerGeilHansenHedinHuovinenJanelmJankovenkoJorsalKantardjjievKisielieneKleinaKohlKolbergKollarKolmosKraujaKruseKruseKutsarLarsenLarssonLopezLundström
First namePederOlivierNielsNielsKåreMadsAnnaPenttiAnitaSvetlanaSven ErikTodorIevaBirutaHenrietteMartinEszterHans JørnIntaHildeThomasKuuloLeneBengtAntonioJenny
TitleDr.Dr.Prof.Prof.MrDr.Dr.Dr.Mrs/MsMrs/MsMrProf.Mrs/MsMrMrs/MsMrDr.Prof.Mrs/MsDr.MrDr.Mrs/MsDr.MrDr.
Ministry/institutionDanish Agency for Science, Technology and InnovationSociété Nationale Des Groupements VétérinairesHvidovre HospitalHvidovre HospitalDanish Permanent Representation to the EUDanish Medical OrganisationReAct - Action on Antibiotic Resistance, Uppsala UniversityNational Institute of Health and WelfareMinistry of Health and Social AffairsPermanent Representation of Estonia to the EUNational Veterinary Institute, Technical University of DenmarkNational Centre Infectious and Parasitic DiseasesMinistry of Health of the Republic of LithuaniaMinistry of Health of the Republic of LatviaDanish Association for the Veterinary Pharmaceutical IndustryNordic CouncilMinistry of Rural DevelopmentOdense University HospitalMinistry of Agriculture, Republic of LatviaWorld Health Organization, Regional Office for EuropeDanish Veterinary and Food AdministrationHealth BoardNordic Council of Ministers secretariatSwedish Board of AgricultureSpanish Agency for Medicines and Health Care ProductsSwedish Animal Health Service
CountryDenmarkFranceDenmarkDenmarkDenmarkDenmarkSwedenFinlandSwedenEstoniaDenmarkBulgariaLithuaniaLatviaDenmarkNorwayHungaryDenmarkLatviaDenmarkDenmarkEstoniaDenmarkSwedenSpainSweden
WorkshopWorkshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 143
SurnameMeijeringMichalikMijovicMonnetMorenoMuchlMøllerNielsenNijlandNørrungO' BrienPallesenPanovskiPedersonPentlerPerrellaPetersenPokludovaPresecki StankoRabschRiesenfeld ÖrnRäsänenSafranySantolini
First nameAlbertLiliannaGordanaDominique LSørenRobertKristianAnnetteRenskeBirgitDeclanLarsNikolaRobertJennyAlessandraTimLucieAleksandraWolfgangIngerLeenaNabilJulien
Ministry/institutionMinistry of EL&IMinistry of HealthInstitute of Public HealthEuropean Centre for Disease Prevention and Control (ECDC)Institute for Rational PharmacotherapyFederal Ministry of HealthNational Veterinary Institute, DTUThe Danish Veterinary and Food AdministrationEmbassy of the Kingdom of the NetherlandsFaculty of Health and Medical SciencesIFAH-EuropeStatens Serum InstitutInstitute of microbiology and parasitology, Medical Faculty-Skopje, Ministry of HealthMrEuropean Public Health and Agriculture ConsortiumMrs/Ms Nordic CouncilDr.Ministry of HealthMrThe Danish Veterinary and Food AdministrationMrs/Ms Institute for State Control of Veterinary Biologicals andMedicinesMrs/Ms KBC ZagrebDr.Robert Koch InstituteDr.The National Board of Health and WelfareDr.Ministry of Agriculture and ForestryMrEuropean Commission, DG Health / ConsumersDr.DG for Food/Ministry for Food, Agriculture and Fisheries
TitleDr.Mrs/MsDr.Dr.MrDr.Dr.Dr.Mrs/MsDr.MrMrProf.
CountryNetherlandsPolandMontenegroEU/EuropeDenmarkAustriaDenmarkDenmarkNetherlandsDenmarkBelgiumDenmarkFYR MacedoniaEU/EuropeDenmarkItalyDenmarkCzech RepublicCroatiaGermanySwedenFinlandEU/EuropeFrance
WorkshopWorkshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 144
SurnameSchlundtSchneiderSkjoldagerStaesSvetlinTörnekeUdsenVan DyckVan HengelVermeerschVillarWagenaarWellsteedWisellZdovcØstergaardHellebrekersSurnameAeschlimannAgersøAzanowskyBarbaraBarnes
First nameJørgenThomasArneBartAntonKarolinaCamillaKoenArjonKatieJuan S.JaapSallyKarinIrenaKnudLudoFirst nameAndreasYvonneJean-michelChristopherBrendan
TitleDr.Dr.
Ministry/institutionNational Food Institute, Technical University of DenmarkFederal Ministry of Food, Agriculture and Consumer Protection
CountryDenmarkGermanyDenmarkBelgiumSloveniaSwedenDenmarkEU/EuropeEU/EuropeBelgiumEU/EuropeNetherlandsUnited KingdomSwedenSloveniaDenmarkNetherlandsCountrySwitzerlandDenmarkFranceMaltaBelgium
WorkshopWorkshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1Workshop 1WorkshopWorkshop 2Workshop 2Workshop 2Workshop 2Workshop 245
MrThe Danish Veterinary AssociationMrs/Ms Member of the EP - Committee on Public HealthMrMinistry of Agriculture, Forestry and Food VeterinaryAdministration of the Republic of SloveniaDr.Medical Products AgencyMrs/Ms Danish Consumer Council/BEUCDr.European Commission, DG Health / ConsumersDr.European Commission, DG Health / ConsumersMrs/Ms Federal Agency for the Safety of the Food ChainMrEAPAProf.Faculty of Veterinary MedicineMrs/Ms Department of HealthDr.Swedish Institute For Communicable DiseasesDr.Veterinary Faculty of Ljubljana, National Veterinary InstiuteMrProf.TitleDr.Dr.Dr.Dr.MrDanish Veterinary and Food AdministrationRoyal Dutch Veterinary AssociationMinistry/institutionResearch Station Agroscope ALPNational Food Institute, Technical University of DenmarkDirection générale de la santé, Ministère de la santéMater Dei HospitalEFPIA
SurnameBattistiBiresBlackyBøggildCarsCavaleriCizmanConnollyCostaDahlDe GraefDe SmetEganEspeisseFeketéné BöröczFriisGrekoGuardabassiHenriksenHeraHolmHonkanen-buzalski
First nameAntonioJozefAlexanderHenrikOttoMarcoMilanEibhlinAnaJanEvelyneKrisJohnOlivierKarolinaChristianChristinaLucaPerAlfredAnjaTuula
Ministry/institutionIZS Latium and TuscanyState Veterinary and Food AdministrationMedical University of Vienna, Austrian Reference Center fornosocomial infections and antimicrobial resistanceDr.National Board of HealthProf.ReAct- Action on Antibiotic Resistance, Uppsala UniversityDr.European Medicines Agency (EMA)Prof.university Medical CentreDr.Department of HealthMrs/Ms General Directorate of HeathMrDanish Agriculture and Food CouncilDr.AMCRADr.European Commission, DG Health & ConsumersDr.NRL AMR (CVRL)Dr.EPRUMADr.National Center for EpidemiologyProf.Danish Medicine AgencyDr.National Veterinary Institute (SVA)Dr.Department of Veterinary Disease Biology, Faculty of Health andMedical Sciences, University of CopenhagenDr.Danish Veterinary and Food AdministrationProf.Institute for State Control of Veterinary Biologicals andMedicinesDr.Danish Medicines AgencyProf.Finnish Food Safety Authority Evira
TitleDr.Prof.Dr.
CountryItalySlovakiaAustriaDenmarkSwedenEU/EuropeSloveniaIrelandPortugalDenmarkBelgiumEU/EuropeIrelandFranceHungaryDenmarkSwedenDenmarkDenmarkCzech RepublicDenmarkFinland
WorkshopWorkshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2
46
SurnameHugasIannazzoIuliaJanosiKaesbohrerKarlsmoseKluytmansKnudsenKontopidouKristensenLeijdekkersLiebanaMackayMatthiessenMølbakNagtzaamOrandOrholmPetersenPicardReichertRimdeikaRoenneSchwarz
First nameMartaStefaniaCohenSzilardAnnemarieSusanneJanJennyFloraBrianFlorisErnestoDavidLineKåreMartinusJean-PierreMarianneNilsJean MichelPaulRytisToveChristine
TitleDr.Dr.Dr.Dr.Dr.Mrs/MsProf.Dr.Dr.MrMrDr.Dr.Dr.Dr.MrDr.Mrs/MsDr.MrMrProf.Dr.Dr.
Ministry/institutionEuropean Food Safety Authority (EFSA)Minister of HealthNational Sanitary Veterinary and Food Safety AuthorityCentral Agricultural OfficeFederal Institute for Risk AssessmentEURL-AR (DTU Food)Amphia Hosp./St. Elisabeth Hosp./TweeSteden Hosp./VUmcCopenhagen University Hospital, Hvidovre HospitalHELLENIC CDCPStatens Serum InstitutMinistry of Economic Affairs, Agriculture and InnovationEuropean Food Safety Authority (EFSA)European Medicines Agency (EMA)European Commission , DG Research & InnovationStatens Serum InstitutEuropean Commission, DG Health & ConsumersFrench Agency for Veterinary Medicinal ProductsDanish Medicines AgencyStatens Serum InstitutMinistry of Food, Agriculture and Fisheries, General Directoratefor FoodLaboratoire National de SanteEuropean Wound Management AssociationNational Board of HealthBVL Federal Office of Consumer Protection and Food SafetyGermany
CountryEU/EuropeItalyRomaniaHungaryGermanyDenmarkNetherlandsDenmarkGreeceDenmarkNetherlandsEU/EuropeEU/EuropeEU/EuropeDenmarkEU(EuropeFranceDenmarkDenmarkFranceLuxembourgLithuaniaDenmarkGermany
WorkshopWorkshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2
47
SurnameSturmaSzilágyiSøltoftVan der JagtVan Der KampVirolainen-julkunenYvesZasepaDamjanovaOsekPeduzziYilmaz
First nameJanEmeseHeidiKatinkaJolandaAnniSalesMagdalenaIvelinaJacekElisabettaSemra
TitleMrDr.Mrs/MsMrs/MsMrs/MsDr.MrMrs/MsDr.Dr.Dr.Dr.
Ministry/institutionNational Institute of Public HealthOffice of the Chief Medical OfficerStatens Serum InstitutCouncil of the European UnionMinistry of Health Welfare and SportMinistry of Social Affairs and HealthDanish Medical AssociationMinistry of Agriculture and Rural DevelopmentNational Center for EpidemiologyNational Veterinary Research InstituteSwiss Federal Office of Public HealthMinistry of Food Agriculture and Livestook/Compatent otorite
CountryCzech RepublicHungaryDenmarkBelgiumNetherlandsFinlandDenmarkPolandHungaryPolandSwitzerlandTurkey
WorkshopWorkshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2Workshop 2/3BWorkshop 2/3BWorkshop 2/3BWorkshop 2/3B
SurnameBorrielloAasmäeBekmanBruchChristiansenCibinDamianDamsoerDewulf
First namePeterPiretHenkMarcelPerVeronicaMariaJohannJeroen
TitleProf.Mrs/MsMrDr.MrDr.Dr.MrProf.
Ministry/institutionVeterinary Medicines DirectorateMinistry of Agriculture Republic of EstoniaProduct board Livestock, Meat and EggsMinistry of HealthMinistry of Food, Agriculture and FisheriesIstituto Zooprofilattico Sperimentale delle Venezie"Cantacuzino" National Institute of Research-Development forMicrobiology and ImmunologyMinistry of HealthAMCRA
CountryUnited KingdomEstoniaNetherlandsLuxembourgDenmarkItalyRomaniaAustriaBelgium
WorkshopWorkshop (3A)Workshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3A48
SurnameGarvanGoossensGraveGötzHardeggerHopkinsInácioJensenLaursenMarottaMijtenMinneMunoz MaderoMuscolo
First nameCarolineHermanKariHans-JoachimMarkusSusanPatríciaVibekeMajaElenaErikDriesCristinaLuisa AnnaAdeleObermayrEugenProkopiakDorotaRasmussenEsbenRauloSaaraRennNickRubio Montejano ConsueloSevensterJanSmeraldiCamillaSogelJelenaSteinbakkMartinTörnChristina
TitleMrs/MsProf.Prof.Dr.Dr.Dr.Mrs/MsDr.Dr.Dr.Dr.MrMrs/MsMrs/MsMrMrs/MsMrDr.Dr.Mrs/MsDr.Mrs/MsMrs/MsDr.Mrs/Ms
Ministry/institutionDepartment of Agriculture, food and MarineUniversity Hospital AntwerpEuropean Medicines Agency (EMA)Bundesverband Praktizierender TierärzteSwiss Federal Office for AgricultureHealth Protection AgencyMinistry of AgricultureDTU FødevareinstituttetStatens Serum InstitutItalian Medicines AgencyCOPA-COGECA (Boerenbond)Federal Agency for Medicines and Health ProductsSpanish Medicinal AgencyItalian Medicines AgencyAgency for Safety in Healthcare (AGES)Ministry of Agriculture and Rural DevelopmentDanish Veterinary and Food AdministrationFinnish Food Safety AuthorityVeterinary Medicines DirectorateSpanish Medicinal AgencyMinistry of Economic Affairs, Agriculture and InnovationEuropean Food Safety Authority (EFSA)Veterinary and Food BoardNorwegian Institute of Public HealthThe Swedish Board of Agriculture
CountryIrelandBelgiumEU/EuropeGermanySwitzerlandUnited KingdomPortugalDenmarkDenmarkItalyBelgiumBelgiumSpainItalyAustriaPolandDenmarkFinlandUnited KingdomSpainNetherlandsEU/EuropeEstoniaNorwaySweden
WorkshopWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3A49
SurnameValintelieneVan Den BrinkVindelWasylWeistZhelyazkovZotaKoningsteinKremerKristensenSchonZagrebnevieneSurnameAarestrupAjufoAspevallBaggesenBarkbuBabovicBeloeilBertrandBjeragerBreck
First nameRolandaRinkeElisabethDariuszKlausPaskalLaviniaMaikeKristinAllanJosephGalinaFirst nameFrankJustinOlleDorteKjerstiTatjanaPierre-AlexandreSophieGitteKarin
Ministry/institutionInstitute of HygieneNOS NewsWorld Organisation for Animal Health (OIE)National Veterinary Research InstituteEuropean Centre for Disease Prevention and Control (ECDC)Ministry of agriculture and food, Bulgarian food safety agencyNational Centre for Surveillance and Control of CommunicableDiseasesMrs/Ms RIVMMsWorld Health Organization, Regional Office for EuropeMrDanish Association of the Pharmaceutical IndustryDr.Agriculture/Laboratoire de Médecine Vétérinaire de l'EtatMrs/Ms Centre for Communicable Diseases and AIDSTitleProf.Dr.Dr.Dr.Mrs/MsMrs/MsDr.Ministry/institutionTechnical University of DenmarkDanish Veterinary and Food AdministrationSwedish Institute for Communicable Disease ControlNational Food Institute, The Technical University of DenmarkNorwegian Food Safety Authority, Head OfficeVeterinary AdministrationEuropean Food Safety Authority (EFSA)
TitleDr.MrDr.Dr.Dr.Prof.Mrs/Ms
CountryLithuaniaNetherlandsFrancePolandEU/EuropeBulgariaRomaniaNetherlandsWHO/EuropeDenmarkLuxembourgLithuaniaCountryDenmarkDenmarkSwedenDenmarkNorwayMontenegroEU/EuropeBelgiumDenmarkDenmark
WorkshopWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3AWorkshop 3A/BWorkshop 3A/BWorkshop 3A/BWorkshop 3A/BWorkshop 3A/BWorkshopWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3B50
Dr.Institute of Public HealthMrs/Ms Danish Veterinary and Food AdministrationMrs/Ms The Danish Veterinary and Food Administration
SurnameBrtkovaBrådenmarkBukovski-SimonoskiButayeCoignardDalsgaardDanuserDe FrutosDumpisEgervärnFlorekGierczynskiGiessenGomesGrundmannHaldHammerumHenglHerrera LeónHopkinsHryniewiczIvanovaJanevskiJarlierJernberg
First nameAndreaAnnaSuzanaPatrickBrunoAndersJürgCristinaUgaMariaKarolinaRafalArjenCarlosHajoTineAnetteBrigitaSilviaKatieWaleriaKateBlazhoVincentCecilia
TitleMsDr.Prof.
Ministry/institutionState Veterinary and Food InstituteNational Food AdministrationUniversity Hospital for Infectious Diseases "Dr Fran Mihaljevic"ZagrebProf.CODA-CERVADr.Institut de Veille Sanitaire (InVS)Prof.University of CopenhagenDr.Swiss Federal Veterinary OfficeMrs/Ms Ministry of Agriculture, Food and Environment AffairsDr.Pauls Stradins University HospitalMrs/Ms National Food AgencyMrs/Ms General Veterinary InspectorateDr.National Institute of Public Health - National Institute of HygieneDr.National Institute of Public Health and the EnvironmentDr.Prof.Dr.Dr.Mrs/MsMrs/MsDr.Prof.Mrs/MsMrMrDr.Ministry of Health / Directorate-General of HealthUniversity Medical Centre GroningenNational Food Institute, DTUStatens Serum InstitutCroatian Food AgencyInstitute of Health Carlos III.Health Protection AgencyNational Medicines InstituteNational Center of Infectious and Parasitic DiseasesFood and Veterinary AgencyAssistance Publique - Hôpitaux de ParisSwedish Institute for Communicable Disease Control
CountrySlovakiaSwedenCroatiaBelgiumFranceDenmarkSwitzerlandSpainLatviaSwedenPolandPolandNetherlandsPortugalNetherlandsDenmarkDenmarkCroatiaSpainUnited KingdomPolandBulgariaFYR MacedoniaFranceSweden
WorkshopWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3B51
SurnameKarpiskovaKoeferLe HelloLeventLo Fo WongLohmanJankovicLópezLundMuchMulhernNielsenO‟ConnorPantostiPeetsoPeran SalaSaez LlorenteSahinSchweickertSelderinaSideroglouSigmundsdottirSiitonenSkov
First nameRenataJosefSimonBelkisDaniloIvanaGemaArvePeterMichaelEvaLisaAnnalisaRitaRosaJose LuisGüzinBirgittaSolvitaTheologiaGudrunAnjaRobert
TitleDr.Prof.Dr.Dr.Dr.Dr.
Ministry/institutionNational Institute of Public HealthVetmeduni ViennaInstitut PasteurMinistry of Health, Refik Saydam National Public Health AgencyWorld Health Organization Regional Office for EuropeMinistry of Agriculture-Veterinary Directorate
CountryCzech RepublicAustriaFranceTurkeyWHO/EuropeCroatiaSpainNorwayAustriaIrelandDenmarkIrelandItalyEstoniaEU/EuropeSpainTurkeyGermanyLatviaGreeceIcelandFinlandDenmark
WorkshopWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3B52
Mrs/Ms Ministry of Agriculture, Food and Environment AffairsDr.Dr.Dr.Dr.MsDr.Dr.Mrs/MsMrMrs/MsDr.Dr.Mrs/MsDr.Dr.Dr.Norwegian Veterinary InstituteAustrian Agency for Health and Food SafetyHealth Service ExecutiveStatens Serum InstitutFood Safety AuthorityIstituto Superiore di SanitàHealth BoardEuropean Commission, DG Health & ConsumersMinistry of Agriculture, Food and EnvironmentMinistry of Food Agriculture and LivestockRobert Koch-InstituteInfectology Center of LatviaHellenic Centre for Disease Control and PreventionCentre for Health Security and Communicable Disease Control,Directorate of HealthThe National Institute for Health and WelfareStatens Serum Institut
SurnameStruelensSørensenTast LahtiThorsteinsdottirTrkovUngerVanholmeVesmesVuopioWallmannWesterZemlickovaSurnameAngenBovilleChan FungGyssensHajlováHauksdottirJakabJuulKunoeMancarellaNanda
First nameMarcAliceElinaThorunnMarijaKilianLucIngridJaanaJürgenAstridHelenaFirst nameØysteinClaireFu ChunMargaretIngeborgAlenaVilborgZsuzsannaMaiAsjaGiovanniArun
TitleProf.Mrs/MsDr.Mrs/MsDr.MrDr.Mrs/MsProf.Dr.Mrs/MsDr.TitleMrMrs/MsDr.
Ministry/institutionEuropean Centre for Disease Prevention and Control (ECDC)Danish Veterinary and Food AdministrationNational Veterinary InstituteThe Directorate of HealthNational Institute of Public HealthDepartment of Agriculture, Food and the MarineFederal Agency for the Safety of the Food ChainMinistry of AgricultureNational Institute for Health and WelfareFederal Office of Consumer Protection and Food SafetyNorwegian Institute of Public HealthNational Institute of Public HealthMinistry/institutionNational Veterinary Institute, Technical University of DenmarkDepartment of HealthWorld Health Organization
CountryEU/EuropeDenmarkSwedenIcelandSloveniaIrelandBelgiumEstoniaFinlandGermanyNorwayCzech RepublicCountryDenmarkUnited KingdomWHONetherlandsSlovakiaDenmarkWHO/EuropeEU/EuropeDenmarkEU/EuropeWHO/Europe
WorkshopWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshop 3BWorkshopNot participatingNot participatingNot participatingNot participatingNot participatingNot participatingNot participatingNot participatingNot participatingNot participatingNot participating53
Prof.SWABMrs/Ms Public Health Authority, Department of EpidemiologyMrs/Ms Nordic Council of MinistersMrs/Ms World Health Organization Regional Office for EuropeMrs/MsMrs/MsMrMrEuropean-ParliamentNational Board of HealthEuropean Centre for Disease Prevention and Control (ECDC)World Health Organization, Regional Office for Europe
SurnameNordvigNørgaardPedersenRakaSeychellSmithSøndergaardSprengerWalshWalterWorningModeratorMeilstrup
First nameRuneNicolajCourtLulMartinElseDortheMarcTimothyAnneAnne Marie
TitleMrMrProf.Prof.MrDr.Mrs/MsDr.Prof.Mrs/MsDr.
Ministry/institutionNational Board of Health (Sundhedsstyrelsen)Pig Research CentreOdense University HospitalMinistry of Health, National Institute of Public Health of KosovaEuropean Commission, DG Health & ConsumersThe National Board of HealthMinistry of HealthEuropean Centre for Disease Prevention and Control (ECDC)Cardiff UniversityNorwegian Directorate of HealthWorld Health Organization
CountryDenmarkDenmarkDenmarkEU/EuropeEU/EuropeDenmarkDenmarkEU/EuropeUnited KingdomNorwayWHO
WorkshopNot participatingNot participatingNot participatingNot participatingNot participatingNot participatingNot participatingNot participatingNot participatingNot participatingNot participating
Per
Mr
Journalist and Climate Director, Monday Morning - a leadingindependent think tank
Denmark
Not participating
OrganisersAmelungGroth RasmussenHansenHoltonKnudsenKrohnLindgaardStrøbækSzpakowskaThoustrup
AndersLineLineChristinaCharlotteMariaGitteGrithEmiliaLisette
MrMrs/MsMrs/MsMrs/MsMrs/MsMrs/MsMrs/MsMrs/MsMrs/MsMrs/Ms
Ministry of Food, Agriculture and FisheriesMinistry of Food, Agriculture and FisheriesMinistry of HealthMinistry of HealthMinistry of Food, Agriculture and FisheriesMinistry of Food, Agriculture and FisheriesMinistry of HealthMinistry of HealthMinistry of HealthMinistry of Health
DenmarkDenmarkDenmarkDenmarkDenmarkDenmarkDenmarkDenmarkDenmarkDenmark
Workshop 3Workshop 3Not participatingNot participatingWorkshop 3Workshop 2Workshop 2Workshop 1Not participatingWorkshop 154
55