Sundheds- og Forebyggelsesudvalget 2011-12
L 185
Offentligt
IS S N 1606- 1691
IS S N 0000- 0000
EMCDDA
MONOGRAPHSHarm reduction:evidence, impacts and challenges
EMCDDAMONOGRAPHSHarm reduction:evidence, impacts and challenges
EditorsTim Rhodes and Dagmar Hedrich
Legal noticeThis publication of the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA)is protected by copyright. The EMCDDA accepts no responsibility or liability for anyconsequences arising from the use of the data contained in this document. The contents ofthis publication do not necessarily reflect the official opinions of the EMCDDA’s partners,the EU Member States or any institution or agency of the European Union or EuropeanCommunities.A great deal of additional information on the European Union is available on the Internet. Itcan be accessed through the Europa server (http://europa.eu).
Europe Direct is a service to help you find answers to your questionsabout the European UnionFreephone number (*):00 800 6 7 8 9 10 11(*) Certain mobile telephone operators do not allow access to 00 800 numbers or these calls may be billed.
Cataloguing data can be found at the end of this publication.Luxembourg: Publications Office of the European Union, 2010ISBN 978-92-9168-419-9doi: 10.2810/29497� European Monitoring Centre for Drugs and Drug Addiction, 2010Reproduction is authorised provided the source is acknowledged.Printed in SpainPrinted on white chlorine-free PaPer
Cais do Sodré, 1249-289 Lisbon, PortugalTel. (351) 211 21 02 00 • Fax (351) 218 13 17 11[email protected] • www.emcdda.europa.eu
ContentsForewordAcknowledgementsPreface71113
IntroductionChapter 1:Harm reduction and the mainstreamTim Rhodes and Dagmar Hedrich19
Part I:Chapter 2:
BackgroundThe diffusion of harm reduction in Europe and beyondCatherine Cook, Jamie Bridge and Gerry V. Stimson37
Chapter 3:
The development of European drug policy and the place of harmreduction within thisSusanne MacGregor and Marcus Whiting59
Chapter 4:
Perspectives on harm reduction — what experts have to sayHarm reduction in an open and experimenting societyJürgen Rehm and Benedikt FischerHCV prevention—a challenge for evidence-based harm reductionMatthew HickmanBroadening the scope and impact of harm reduction for HIV prevention,treatment and care among injecting drug usersAndrew BallTranslating evidence into action — challenges to scaling upharm reduction in Europe and Central AsiaRifat Atun and Michel KazatchkinePeople who use drugs and their role in harm reductionMat SouthwellHarm reduction — an ‘ethical’ perspectiveCraig FryThe ambiguity of harm reduction — goal or means,and what constitutes harm?Robin Room
797985
89
94101104
108
Part II:Chapter 5:
Evidence and impactsHarm reduction among injecting drug users — evidenceof effectivenessJo Kimber, Norah Palmateer, Sharon Hutchinson,Matthew Hickman, David Goldberg and Tim Rhodes115
Chapter 6:
The effect of epidemiological setting on the impact of harm reductiontargeting injecting drug usersPeter Vickerman and Matthew Hickman165
Chapter 7:
The fast and furious — cocaine, amphetamines and harm reductionJean-Paul Grund, Philip Coffin, Marie Jauffret-Roustide,Minke Dijkstra, Dick de Bruin and Peter Blanken
191
Chapter 8:
Harm reduction policies for cannabisWayne Hall and Benedikt Fischer
235
Chapter 9:
Harm reduction policies for tobaccoCoral Gartner, Wayne Hall and Ann McNeill
255
Chapter 10:
Alcohol harm reduction in EuropeRachel Herring, Betsy Thom, Franca Beccaria,Torsten Kolind and Jacek Moskalewicz
275
Part III:Chapter 11:
Challenges and innovationsDrug consumption facilities in Europe and beyondDagmar Hedrich, Thomas Kerr and Fran§oise Dubois-Arber305
Chapter 12:
User involvement and user organising in harm reductionNeil Hunt, Eliot Albert and Virginia Montañés Sánchez
333
Chapter 13:
Young people, recreational drug use and harm reductionAdam Fletcher, Amador Calafat, Alessandro Pirona andDeborah Olszewski
357
Chapter 14:
Criminal justice approaches to harm reduction in EuropeAlex Stevens, Heino Stöver and Cinzia Brentari
379
Chapter 15:
Variations in problem drug use patterns and their implicationsfor harm reductionRichard Hartnoll, Anna Gyarmathy and Tomas Zabransky405
ConclusionsChapter 16:Current and future perspectives on harm reduction in theEuropean UnionMarina Davoli, Roland Simon and Paul Griffiths437
ContributorsAbbreviationsFurther reading
449455461
ForewordIt is with great pleasure that I introduce the EMCDDA´s latest Scientific monograph, whichprovides a state-of-the-art review of the role of harm reduction strategies andinterventions. Harm reduction has become an integral part of the European policy debateon drugs, but this was not always the case. Although harm reduction approaches have along history in the addictions field and in general medicine, our modern concept of harmreduction has its roots in the challenges posed by the rapid spread of HIV infectionamong drug injectors in the mid-1980s. Initially, there was considerable controversysurrounding the notion that preventing the spread of HIV was of paramount importanceand required immediate and effective action, even if this meant that abstinence as atherapeutic goal had to take second place.In Europe today, that controversy has to a large extent been replaced by consensus. Thisreflects not only a general agreement on the value of the approach but also recognition thatnational differences in interpretation and emphasis exist. Harm reduction as a concept is nowaccepted as part of abalanced approach,an integral element of a comprehensive strategythat includes prevention, treatment, social rehabilitation and supply reduction measures. This,I would argue, is a strong endorsement of the pragmatic and evidence-based approach thatEuropean drug policies have come to embrace.It would be wrong to overstate this position; the drug debate remains an ideological as wellas a scientific one. Nonetheless, the evidence that needle exchange and substitution treatmentcan be effective elements in a strategy to reduce HIV infection among injectors, andimportantly that these interventions do not lead to greater harms in the wider community, hashad a significant impact on European drug policies and actions. Although it would be wrongto minimise the continuing problem that we face, when comparing Europe to many otherparts of the world it is clear that overall our pragmatic approach has borne fruit. Argumentsmay still exist about the relative role played by different types of interventions, but mostinformed commentators would now agree that harm reduction approaches have beeninfluential in addressing the risks posed by drug injecting in Europe over the last 20 years.This is, then, an appropriate moment to take stock of existing scientific evidence on harmreduction and consider the issues that we will need to tackle in the future. The evidence forsome harm reduction interventions is relatively robust. For others, methodological difficultiesmake generating a solid evidence base difficult, and the current scientific bases for guidingpolicymaking need to be strengthened.The assertion that the concept of harm reduction is an accepted part of the European drugpolicy landscape does not mean that all interventions that fall under this heading are eitherwidely supported or endorsed. Many areas of controversy remain, and one purpose of thismonograph is to chart where the current fault lines now lie, with the hope that future studieswill provide a sounder basis for informed actions. Moreover, and perhaps more importantly,the drug problems and issues we face in Europe today are very different to those we7
Harm reduction: evidence, impacts and challenges
struggled with in the past. HIV remains an important issue, but it is no longer thepredominant one. From a quantitative public health point of view, drug overdose, HCVinfection, and other psychiatric and physical co-morbidities are becoming of equal or evengreater importance. In addition, drug injecting levels appear to be falling and patterns ofdrug taking are become more complex and are increasingly characterised by theconsumption of multiple substances, both licit and illicit.What role will harm reduction have within this new landscape? This monograph begins toexplore that question, as we consider how harm reduction strategies may be a usefulcomponent of our approach to the challenges that drug use in twenty-first century Europe willbring. I strongly believe that in taking drug policy forward we have a duty to learn from thepast, and that ideological positions should not stand in the way of a cool-headed analysis ofthe evidence. In the future this is likely to become imperative both to those who instinctivelysupport harm reduction approaches, and to those who instinctively oppose them. Thismonograph makes an important contribution to the debate by highlighting where we arenow, and considering how we have got here. It also draws our attention to some of thechallenges that lie ahead, if we are to understand the role and possible limits of harmreduction approaches to future European drug policies.Wolfgang GötzDirector, EMCDDA
8
AcknowledgementsThe EMCDDA would like to thank all authors, editors and reviewers who have worked on thispublication. In particular, the monograph benefited from overall editorial input by TimRhodes and Dagmar Hedrich. A special mention goes to the members of the internalcoordination group who accompanied the project from inception to publication — namely toAlessandro Pirona and Anna Gyarmathy; as well as to the planning group: Roland Simon,Rosemary de Sousa, Paul Griffiths, Julian Vicente and Lucas Wiessing. The EMCDDAgratefully acknowledges the contributions from many unknown external reviewers and fromthe reviewers drawn from the EMCDDA’s Scientific Committee. Furthermore, valuable reviewcomments and input were received from EMCDDA staff members Marica Ferri, BrendanHughes, André Noor, Cécile Martel, Luis Prieto and Frank Zobel. Vaughan Birbeck providedmuch appreciated help with bibliographic references, and Alison Elks of Magenta Publishingedited the final publication.
11
PrefaceHarm reduction is now positioned as part of the mainstream policy response to drug usein Europe. However, this has not always been the case, and in reflecting on this fact wefelt that the time was right to take stock of how we had arrived at this position, ask what itmeans for both policies and action, and begin to consider how harm reduction is likely todevelop in the future.This monograph builds on other titles in the EMCDDA’s Scientific monographs series,where we have taken an important and topical subject, assembled some of the bestexperts in the field, and allowed them to develop their ideas constrained only by theneed to demonstrate scientific rigour and sound argument. Our Scientific monographs areintended to be both technically challenging and thought provoking. Unlike our otherpublications we take more of an editorial ‘back seat’ and we do not seek consensus ornecessarily to produce a balanced view. Good science is best done when unconstrained,and best read with a critical eye.This volume includes a variety of perspectives on harm reduction approaches, togetherwith an analysis of the concept’s role within drug policies, both in Europe and beyond.Readers may not necessarily agree with all of the arguments made or the conclusiondrawn, but we hope it is perceived as a valuable contribution to the ongoing debate onhow to respond to contemporary drug problems in Europe.A number of contributors explore what harm reduction means and what policies it canencompass, as well as charting how the concept evolved. They reflect on the point wehave now reached in terms of both harm reduction practice and the evidence base for itseffectiveness. A major issue that many contributors touch on is the difficulty of assessinghow complex interventions occurring in real world settings can be evaluated, and whyconclusive evidence in such settings can be so elusive.With an eye to the future, we also asked our contributors to wrestle with the difficultissue of how harm reduction might be extended into new areas that are of particularrelevance to the evolving European drug situation. Here the empirical base forgrounding discussions is far less developed, and a more exploratory approach isnecessary.As a European agency, the EMCDDA has a somewhat unique perspective on thedevelopment of the drugs debate within the European Union. It is therefore appropriatefor us to make our own introductory remarks about the mainstreaming of the concept ofharm reduction at the European level, as opposed to the national one. Thisdevelopment, we would argue, is sometimes misunderstood, as there is a tendency bysome commentators to polarise the position and focus exclusively on either thedifferences, or alternatively the commonalities, that exist between Member States intheir drug policies. Europe is closer now than it once was in terms of how it responds to13
Harm reduction: evidence, impacts and challenges
and views drug use, but differences still exist, reflecting national policy perspectives,cultural differences and, to some extent, simply a different experience of the drugproblem.Despite these differences in opinion and experience, there is a general consensus thatabstinence-orientated drug policies need to be supplemented by measures that candemonstrably reduce the harms that drug users are exposed to. This consensus isstrongest in the area of reducing HIV infection among injectors — although even herethere is disagreement on the appropriateness of which interventions might fall under thisgeneral heading. It is also the case that the range and intensity of harm reductionservices available in EU Member States varies considerably. Therefore, the observationthat harm reduction has played an important part in achieving the relatively positiveposition that the EU has achieved with respect to HIV infection among injectors has to betempered with the comment that some countries have maintained low rates of infectionsamong injecting drug users where the availability of harm reduction services has beenlimited.In summary, considerable debate still exists at European level on the appropriateness ofdifferent approaches, and some interventions, such as drug consumption rooms, are stillhighly contentious. However, Europe’s policy debate in this area appears now to be amore pragmatic one in which harm reduction policies are not automatically considered toconflict with measures intended to deter drug use or promote abstinence. Rather, theconsensus is increasingly moving towards a comprehensive, balanced and evidence-based approach that seamlessly includes harm reduction alongside prevention, treatmentand supply reduction measures.This monograph is comprehensive in its scope. It covers interventions that are stillcontroversial and ones that have become so mainstream that many might now find it hardto believe that this has not always been the case. We have included voices from the usercommunity, as activism has historically been an important element in the development ofthis perspective. The monograph also addresses new challenges for a harm reductionapproach, such as alcohol and tobacco use and Europe’s growing appetite for stimulantdrugs.The EMCDDA is grateful that so many experts were prepared to assist us with this work,often tackling new and demanding topics. This task would have been infinitely moredifficult if we had not benefited from having a first-class editorial team working on thisproject. We are indebted to our editors, Tim Rhodes and Dagmar Hedrich, who bothplayed a major role in conceptualising, planning and implementing this project andwithout whose input this document would have been a far less comprehensive andimpressive achievement.It is important to note that the voices presented here are not those of the EMCDDA orthe European institutions. As with other Scientific monographs, the intention is toprovide a forum for stimulating debate and collecting high-quality scientific opinion andinformed comment on a topic of contemporary relevance. The monographs are14
Preface
intended to be of particular interest to a specialist audience and therefore some of thepapers in this collection are highly technical in nature. All papers presented here havebeen peer-reviewed to ensure an appropriate degree of scientific rigour, but the viewsexpressed by the authors remain their own.The EMCDDA’s role is as a central reference point on drug information within theEuropean Union. We are policy neutral; our task is to document and report, and never toadvocate or lobby. This neutrality is important when we address any drug use issue, asthis is an area where so many have passionate and deeply held views. However, it isparticularly important when we address a topic like harm reduction, where perspectivesare sometimes polarised and there are those on all sides of the drugs debate that see alinkage between this subject and broader issues about how societies control drugconsumption. The rationale for our work is that, over time, better policy comes fromdebate informed by a cool-headed and neutral assessment of the information available.Many of the contributors to this report are passionate and committed in their views; theyalso provide a wealth of data, analysis and argumentation. They do not speak with acommon voice, and we do not necessarily endorse all the conclusions drawn, but takencollectively we believe they make a valuable contribution to a better understanding of atopic that has become an important element in contemporary drug policies.Paul Griffiths and Roland SimonEMCDDA
15
Introduction
Chapter 1Harm reduction and the mainstreamTim Rhodes and Dagmar Hedrich
AbstractHarm reduction encompasses interventions, programmes and policies that seek to reducethe health, social and economic harms of drug use to individuals, communities and societies.We envisage harm reduction as a ‘combinationintervention’,made up of a package ofinterventions tailored to local setting and need, which give primary emphasis to reducingthe harms of drug use. We note the enhanced impact potential derived from deliveringmultiple harm reduction interventions in combination, and at sufficient scale, especiallyneedle and syringe distribution in combination with opioid substitution treatmentprogrammes. We note that harm reduction is a manifestation of mainstream public healthapproaches endorsed globally by the United Nations, and in the EU drugs strategy andaction plans, and features as an integral element of drug policy in most of the Europeanregion. However, we note evidence that links drug harms to policies that emphasise strictlaw enforcement against drug users; an unintended consequence of international drugcontrol conventions. The continuum of ‘combination interventions’ available to harmreduction thus extends from drug treatment through to policy or legal reform and theremoval of structural barriers to protecting the rights of all to health. We end by introducingthis monograph, which seeks to reflect upon two decades of scientific evidence concerningharm reduction approaches in Europe and beyond.
IntroductionHarm reduction encompasses interventions, programmes and policies that seek to reducethe health, social and economic harms of drug use to individuals, communities andsocieties. A core principle of harm reduction is the development of pragmatic responses todealing with drug use through a hierarchy of intervention goals that place primaryemphasis on reducing the health-related harms of continued drug use (Des Jarlais, 1995;Lenton and Single, 2004). Harm reduction approaches neither exclude nor presume atreatment goal of abstinence, and this means that abstinence-oriented interventions canalso fall within the hierarchy of harm reduction goals. We therefore envisage harmreduction as a ‘combinationintervention’,made up of a package of interventions tailoredto local setting and need that give primary emphasis to reducing the harms of drug use. Inrelation to reducing the harms of injecting drug use, for example, this combination ofinterventions may draw upon needle and syringe programmes (NSPs), opioid substitutiontreatment (OST), counselling services, the provision of drug consumption rooms (DCRs),peer education and outreach, and the promotion of public policies conducive to protectingthe health of populations at risk (WHO, 2009).19
Harm reduction: evidence, impacts and challenges
Harm reduction as mainstream public healthHarm reduction in the drugs field has a long history, variably traced back to the prescriptionof heroin and morphine to people dependent on opioids in the United Kingdom in the 1920s(Spear, 1994), the articulation of public health concerns of legal drugs, alcohol and tobacco,and the introduction of methadone maintenance in the United States in the 1960s (Bellis,1981; Erickson, 1999). By the 1970s, the World Health Organization (WHO) recommendedpolicies of harm reduction to ‘prevent or reduce the severity of problems associated with thenon-medical use of dependence-producing drugs’, noting that this goal is at once ‘broader,more specific’ as well as ‘more realistic’ than the prevention of non-medical use per se inmany countries (WHO, 1974; Ball, 2007).The concepts of risk and harm reduction are closely aligned to that of health promotion andpublic health more generally. Yet in relation to illicit drugs, debates about developing publichealth approaches to reducing drug-related harms are often clouded by harm reductionpositioned as a symbol of radical liberalisation or attack upon traditional drug control. Publichealth has at its core the idea of protecting individual and population health through thesurveillance, identification and management of risk to health (Ashton and Seymour, 1988;Peterson and Lupton, 1996). It is essentially a model of risk and harm reduction. The new publichealth movement of the mid-1980s coincided with the emergence of human immunodeficiencyvirus (HIV) epidemics in many countries. This new vision of public health was heralded as a shiftbeyond narrowly defined biomedical understandings towards one that envisaged health andharm as also products of the social and policy environment, and which gave greater emphasisto community-based and ‘low-threshold’ interventions (WHO, 1986). Contemporary publichealth thus characterises risk and health decision-making as a responsibility of health consciousindividuals whilst also emphasising the significance of the social environment in producing harmand in shaping the capacity of individuals and communities to avoid risk (Peterson and Lupton,1996; Rhodes, 2002). Consequently, mainstream public health approaches recognise the needto create ‘enabling environments’ for risk reduction and behaviour change, including throughthe strengthening of community actions and the creation of public policies supportive of health(WHO, 1986). Harm reduction is an exemplar of mainstream public health intervention.
Harm reduction as mainstream drug policy in EuropeEuropean intergovernmental collaboration and information exchange in the drugs field datesback to the early 1970s. While drug policy in the European Union (EU) remains primarily theresponsibility of the Member States, cooperation in matters of drug policy between EUcountries increased over the 1990s, resulting in the adoption of a joint EU drugs strategy aswell as the elaboration of detailed action plans (MacGregor and Whiting, 2010).The EU drugs strategy aims at making ‘a contribution to the attainment of a high level of healthprotection, well-being and social cohesion by complementing the Member States’ action inpreventing and reducing drug use, dependence and drug-related harm to health and society’and at ‘ensuring a high level of security for the general public’ (Council of the European Union,2004, p. 5). For over a decade, EU drug action plans have given priority to preventing the20
Chapter 1: Harm reduction and the mainstream
transmission of infectious disease and reducing drug-related deaths among drug usingpopulations. In a Recommendation adopted by the European Council of 18 June 2003 on the‘prevention and reduction of health-related harm associated with drug dependence’ (Council ofthe European Union, 2003), a framework for action is outlined to assist Member States todevelop strategies to reduce and prevent drug-related harm through the implementation ofharm reduction services for problem drug users. The Recommendation seeks to reduce thenumber of drug-related deaths and extent of health damage, including that related to HIV,hepatitis B (HBV), hepatitis C (HCV) and tuberculosis (TB). These aims are reiterated in thepriorities of the current EU drugs strategy 2005–12 related to demand reduction, aiming at the‘measurable reduction’ of drug use, dependence and drug-related health and social riskthrough a package of interventions combining harm reduction, treatment and rehabilitation,and which emphasise the need to enhance both the ‘quality’ and ‘effectiveness’ of services.Under the responsibility of the EU Commission, progress reviews of the implementation of theEU drugs action plans are carried out with the Member States and additional studies arecommissioned to assess broader policy aspects. Such studies suggest a growing emphasisplaced upon demand and harm reduction in national drug policies in the EU (van derGouwe et al., 2006; European Commission, 2002, 2006, 2008, 2009). The reduction ofdrug harms thus features as a public health objective of all EU Member States (van derGouwe et al., 2006; Cook et al., 2010; MacGregor and Whiting, 2010), with a trend inEurope towards the ‘growth and consolidation of harm reduction measures’ (EMCDDA,2009a, p. 31). The European Commission has noted ‘a process of convergence’ in the drugpolicy adopted by Member States and, as a consequence, increased evidence of ‘policyconsistency’ across the region (European Commission, 2008, p. 67). This convergencetowards harm reduction in drug policy in Europe has been described as the ‘commonposition’ (Hedrich et al., 2008, p. 513).The ‘mainstreaming’ of harm reduction is also evidenced by its transference acrosssubstances, including those causing the greatest burden of global health harm at apopulation level, such as alcohol and tobacco (Rehm et al., 2009; Mathers and Loncar,2006; Rehm and Fischer, 2010; Room, 2010). While the adoption of harm reductionmeasures in relation to tobacco is relatively developmental (Sweanor et al., 2007; Gartner etal., 2010), alcohol harm reduction has a long tradition and is a core feature of alcohol policyin many countries (Robson and Marlatt, 2006; Herring et al., 2010). Harm reduction mayalso feature as a stratagem of public health intervention in relation to cannabis, recreationaland stimulant drug use (Hall and Fischer, 2010; Fletcher et al., 2010; Grund et al., 2010).
Global drug control and harm reductionA recent EU Commission study on global illicit drug markets found no evidence that the globaldrug problem had been reduced in the past decade, but judged that the enforcement of drugprohibition had caused substantial unintended harms (European Commission, 2009). Thislatter finding was shared by the United Nations Office on Drugs and Crime (UNODC) in anevaluation of a century of international drug control efforts 1909–2009 (UNODC, 2009). Thereport clarifies that public health was the driving concern behind drug control, the21
Harm reduction: evidence, impacts and challenges
fundamental objective of the international drug control conventions being to limit the licit tradein narcotic drugs to medical requirements. It states: ‘Public health, the first principle of drugcontrol, has receded from that position, over-shadowed by the concern with public security’,and that ‘looking back over the last century, one can see that the control system and itsapplications have had several unintended consequences’ (UNODC, 2009, pp. 92–3), amongthem the emergence or growth of illicit drug markets, and a ‘policy displacement’ to investingin law enforcement responses, with a corresponding lack of investment in tackling the publichealth harms of drug use. International drug control is framed by three major UN drugtreaties (of 1961, 1971 and 1988), which encourage UN Member States to develop nationalpolicies based on strict law enforcement (Bewley-Taylor, 2004; Wood et al., 2009). There is anincreased momentum, contextualised by a ‘preponderance of evidence’, in support ofrecognising that the current international drug control framework is associated with multiplehealth and social harms, and that these iatrogenic effects can include the exacerbation of HIVepidemics among injecting drug users (IDUs) (Wood et al., 2009, p. 990).Agencies within the UN system have recently re-focused their attention on the primacy ofpublic health, embracing harm reduction interventions as part of a balanced approach withcomplementarity to prevention and treatment interventions. In December 2005, the UnitedNations (UN) General Assembly adopted a resolution encouraging global actions towards‘scaling-up HIV prevention, treatment, care and support with the aim of coming as close aspossible to the goal of universal access to treatment by 2010 for all those who need it’(United Nations General Assembly, 2006). This led to the development of the WHO, UNODCand United Nations Joint Programme on HIV/AIDS (UNAIDS) joint technical guide forcountries on target setting for universal access to HIV prevention, treatment and care forinjecting drug users, and focused advocacy efforts on the need for greater coverage towards‘universal access’ (Donoghoe et al., 2008; WHO et al., 2009; ECOSOC, 2009). Scaling-upaccess to, and achieving adequate coverage of, a ‘comprehensive package’ of harmreduction for problem drug users is a major driver of current global drug policy initiatives(WHO, 2009; Ball, 2010; Atun and Kazatchkine, 2010).
Harm reduction as a ‘combination intervention’As a ‘combination intervention’, harm reduction comprises a package of interventionstailored to local setting and need, including access to drug treatment. In reducing the harmsof drug injecting, for example, a harm reduction package may combine OST, NSPs, DCRsand counselling services with peer interventions as well as actions to lobby for policy change.Envisaging harm reduction as a combination intervention is not merely pragmatic and borneout of need, but is also evidence-based. Evidence points towards the enhanced impact ofharm reduction services when they work in combination. Cohort and modelling studies haveshown that the impact of NSP and OST on reduced incidence of infectious disease amongIDUs can be minimal if delivered as ‘stand-alone’ interventions but are markedly moreeffective when delivered in combination, with sufficient engagement among participants toboth (Van Den Berg et al., 2007). This may be especially the case in reducing the incidenceof HCV among IDUs (Hickman, 2010). While epidemiological studies associate NSP and OST22
Chapter 1: Harm reduction and the mainstream
with reduced HIV risk and transmission (Gibson et al., 2001; Wodak and Cooney, 2005;Farrell et al., 2005; Institute of Medicine, 2007; Palmateer et al., 2010; Kimber et al., 2010),the evidence for these interventions impacting on HCV risk and transmission is more modest(Muga et al., 2006; Wright and Tompkins, 2006; Hallinan et al., 2004; Goldberg et al.,2001; Palmateer et al., 2010; Kimber et al., 2010). To date, there is only one European studyshowing that ‘full participation’ across combined harm reduction interventions (NSP andOST) can reduce HIV incidence (by 57 %)andHCV incidence (by 64 %) (van den Berg et al.,2007). A recent cohort study in the United Kingdom also links OST with statistically significantreductions in the incidence of HCV (Craine et al., 2009). Findings noting the enhanced effectof OST in combination with NSP on reduced HIV and HCV incidence among IDUs haveparticular relevance for countries experiencing explosive outbreaks of infectious disease.Just as the effectiveness of NSP and OST services may be enhanced when combined, there isan ‘enhanced impact’ relationship between participation in OST and adherence to HIVtreatment and care among IDUs (Malta et al., 2008; Palepu et al., 2006; Lert andKazatchkine, 2007). There is a potential HIV prevention effect derived from maximisingaccess to HIV treatment (Ball, 2010; Montaner et al., 2006). Similarly, low-threshold access toHIV testing is an important combinative component of harm reduction. In the EU, there is aconsiderable level of homogeneity in policy priorities regarding measures to limit the spreadof infectious diseases among drug users, with NSP being offered either in combination withvoluntary testing and counselling for infectious disease, or in combination with thedissemination of information, education and communication materials (EMCDDA, 2009a, p.83; EMCDDA, 2009c). Evidence also suggests an enhanced impact relationship betweenhepatitis C treatment and access to drug treatment and social support services (Grebely etal., 2007; Birkhead et al., 2007). Additionally, the integration of HIV treatment services withTB treatment and prevention services is a critical feature in determining health outcomes inpeople living with HIV (Sylla et al., 2007), especially in transitional Europe, which is‘especially severely affected’ by TB drug resistance among drug using populations (WHO etal., 2008). Moreover, in HIV prevention there may be combined intervention effects resultingfrom sexual risk reduction being delivered alongside harm reduction (Lindenburg et al.,2006; Copenhaver et al., 2006). Harm reduction integrates with treatment and care in acombined intervention approach (Ball, 2010).
Harm reduction and ‘enabling environments’ for healthA fundamental tenet of public health intervention is to create environments conducive toindividual and community risk avoidance, including through the creation and maintenance ofpublic policies supportive of health (WHO, 1986). The continuum of ‘combinationinterventions’ available to harm reduction extends from drug prevention and treatmentthrough to policy reform and the removal of structural barriers to protecting the rights of allto health. WHO makes specific recommendation for ‘laws that do not compromise access toHIV services for drug users through criminalisation and marginalisation’ (Ball, 2007). If publicpolicies or laws generate harm then these too fall within the scope of the combination ofinterventions that make up harm reduction. Structural interventions for public health seek toremove contextual or environmental barriers to risk and harm reduction while enabling social23
Harm reduction: evidence, impacts and challenges
and environmental conditions that protect against risk and vulnerability (Blankenship et al.,2006). The delineation of the ‘risk environment’ surrounding the production of drug harms indifferent settings has led to the identification of structural interventions with the potential forencouraging community-level change (Rhodes, 2002, 2009).Of critical concern — as evidenced by multiple studies in multiple settings — is how the legalenvironment can constrain risk avoidance and promote harm among problem drug users,especially among people who inject drugs (Small et al., 2006; Rhodes, 2009; Kerr et al.,2005). In some settings, intense street-level police surveillance and contact can be associatedwith reluctance among IDUs to carry sterile needles and syringes for fear of arrest, caution, fineor detention (Rhodes et al., 2003; Cooper et al., 2005; Miller et al., 2008). Evidence associateselevated odds of syringe sharing with increased police contact (Rhodes et al., 2004),confiscation of injecting equipment (Werb et al., 2008), and rates of arrest (Pollini et al., 2008),yet rates of arrest can show no deterrent effect on levels of injecting (Friedman et al., 2010).High-visibility policing, and police ‘crackdowns’, have been linked to the interruption of saferinjecting routines, leading to safety ‘short-cuts’ or hasty injections, exacerbating the risk of viraland bacterial infections as well as overdose (Blakenship and Koester, 2002; Bluthenthal et al.,1999; Small et al., 2006). Such policing practices may displace drug users geographically,disrupt social networks of support, contribute to the stigmatisation of drug use, and limit thefeasibility, coverage and impact of public health responses (Burris et al., 2004; Davis et al.,2005; Friedman et al., 2006; Broadhead et al., 1999). In turn, prison and incarceration arelinked to elevated odds of HIV transmission among people who use drugs (Dolan et al., 2007;Jürgens et al., 2009; Stevens et al., 2010).Harm reduction may therefore include interventions that seek to reduce the harms generatedby drug and other public policies, including through policy reform and legal change. Forinstance, as Room (2010, p. 110) notes: ‘If the harm arises from heavy use per se, reducingor eliminating use or changing the mode of use are the logical first choices for reducing theharm. But if the harm results from the criminalisation per se, decriminalising is a logical wayof reducing the harm.’ WHO also notes that ‘the alignment of drug control measures withpublic health goals [is] a priority’ (Ball, 2007, p. 687). It is therefore important to note thepotential public health gains of engaging policing and criminal justice agencies as part oflocal public health partnerships, including in the delivery of harm reduction interventions incommunity and closed settings (see Stevens et al., 2010).
Coverage and scale-up2010 is the year for achieving the UN General Assembly target of ‘near universal access’ toHIV prevention, treatment and care for populations affected by HIV. In Europe, considerableprogress has been made towards achieving greater coverage of harm reduction services forIDUs (see Cook et al., 2010). Every EU Member State has one or more needle and syringeprogrammes (EMCDDA, 2009a). Pharmacy-based NSPs operate in at least 12 MemberStates. All Member States provide opioid substitution treatment for those with opioiddependence (EMCDDA, 2009a). An estimated 650,000 people were receiving OST inEurope in 2007, though large national variations in coverage exist (EMCDDA, 2009a).24
Chapter 1: Harm reduction and the mainstream
Evidence suggests coverage is an important determinant of drug-related risk and harm. In arecent comparison of the incidence of diagnosed HIV among IDUs and the coverage of OSTand NSP in the EU and five other middle- and high-income countries, those countries withgreatest provision of both OST and NSP in 2000 to 2004 had lower HIV incidence in 2005and 2006 (Wiessing et al., 2009). In this study, the availability and coverage of harmreduction measures was considerably lower in Russia and Ukraine where the incidence ofHIV was considerably higher when compared to Western European countries. Whereas HIVtransmission rates are stabilising or decreasing in most of Western and Central Europe, theyare increasing in the Eastern part of the continent, outside the EU, where harm reductionservices are ‘insufficient and need to be reinforced’ (Wiessing et al., 2008).Coverage of harm reduction interventions is variable within the EU. While recent estimates ofthe total number of OST clients represent around 40 % of the estimated total number ofproblem opiate users in the EU, the level of provision is far from uniform across the region.Estimates of coverage from 10 countries where such data are available range from below5 % to over 50 % of opioid users covered by OST (EMCDDA, 2009e).European trends in the provision of NSP between 2003 and 2007 show a 33 % increase inthe number of syringes distributed through specialised programmes, with steady increasesin most countries, except several countries in northern and central Europe (EMCDDA,2009d). Although country-specific coverage estimates of NSP are scarce, the number ofsyringes distributed by specialist NSPs per estimated IDU per year seems to vary widelybetween countries (EMCDDA, 2010). European-level estimates suggest that on averagesome 50 syringes are distributed per estimated IDU per year across the EU (Wiessing et al.,2009). Overall availability of sterile syringes is also dependent upon pharmacy provision, inturn influenced by legislation, regulations, and pricing, as well as by the attitudes ofpharmacists.In its evaluation of the EU drug action plan, the European Commission emphasised that the‘availability and accessibility of [harm reduction] programmes are still variable among theMember States’ and that ‘further improvements are still needed in [the] accessibility,availability and coverage’ of services (European Commission, 2008, p. 66). In the Europeanregion more generally, scaling up comprehensive service provision is a priority, withstrengthening health systems, engaging civil society, and securing political commitment forharm reduction considered key determinants to effective scale-up (Atun and Kazatchkine,2010). There is then considerable variability in how harm reduction is enacted in policy andeven more so in practice, as well as resistance to the mainstreaming of harm reduction insome settings. Understanding the failure to implement evidence-based programmes andpolicies has been identified as a major topic for future research (Des Jarlais and Semaan,2009). In countries where heroin epidemics are recent and rates of HIV infection among drugusers low, implementation of harm reduction measures such as NSP or OST may beperceived by some as difficult to justify. This may be especially so in the context of finite andretracting economic resources in the health sector. Evidence, however, indicates the cost-effectiveness of the introduction and scale-up of harm reduction (Zaric et al., 2000; NationalCentre in HIV Epidemiology and Clinical Research UNSW, 2009).25
Harm reduction: evidence, impacts and challenges
Voices of resistance to the mainstreaming of harm reduction in drug policy can be foundwithin the EU (see MacGregor and Whiting, 2010), but are most vociferous within thebroader European region, and especially Russia, which today has one of the largestepidemics of HIV associated with drug injecting in the world, has a policy that places strongemphasis on law enforcement, prohibits the introduction of OST and limits the developmentof NSP and other harm reduction interventions to adequate scale (Sarang et al., 2007;Human Rights Watch, 2007; Elovich and Drucker, 2008).
Evidence, impacts and challengesAn effective harm reduction policy, programme or intervention is one that ‘can bedemonstrated, to a reasonable and informed audience, by direct measurement or otherwise,that on balance of probabilities has, or is likely to result in, a net reduction in drug-relatedharm’ (Lenton and Single, 2004, p. 217). This monograph aims to reflect upon over twodecades of harm reduction research, evidence and impact in Europe and beyond.There are now multiple systematic and other reviews of the scientific evidence in support ofdifferent harm reduction interventions, especially in the context of HIV, hepatitis C andinjecting drug use (Wodak and Cooney, 2005; Farrell et al., 2005; Institute of Medicine,2007; Palmateer et al., 2010). Chapters in this monograph take stock of such evidence inEuropean perspective, including regarding the effectiveness of interventions to prevent HIVand HCV among injecting drug users (Chapter 5 — Kimber et al., 2010), the role of DCRs(Chapter 11 — Hedrich et al., 2010), the effect of epidemiological setting on interventionimpact (Chapter 6 — Vickerman and Hickman, 2010) and the implications that variations indrug use patterns have on harm reduction interventions (Chapter 15 — Hartnoll et al., 2010).While diffusing throughout Europe primarily in response to health harms linked to injectingdrug use (Chapter 2 — Cook et al., 2010; Chapter 3 — MacGregor and Whiting, 2010),harm reduction approaches have mainstream applicability. Chapters consider the specificchallenges of harm reduction interventions and policies regarding alcohol (Chapter 10 —Herring et al., 2010), tobacco (Chapter 9 — Gartner et al., 2010), cannabis (Chapter 8 —Hall and Fischer, 2010), recreational drug use among young people (Chapter 13 — Fletcheret al., 2010), and stimulants (Chapter 7 — Grund et al., 2010). The potential role — oftenunrealised — of drug user engagement and criminal justice interventions are also discussed(Chapter 12 — Hunt et al., 2010; Chapter 14 — Stevens et al., 2010). Taken together, thismonograph seeks to synthesise, as well as critically appraise, evidence of the impacts andchallenges of harm reduction interventions and policies in Europe and beyond.Harm reduction, like any public policy, is inevitably linked to political debate, and it is naiveto assume otherwise, but it is precisely because of this that it is imperative that interventionsare also developed upon evidence-based argument and critique. Europe is experiencingsignificant political change, which in 2004 enabled the most extensive wave of EuropeanUnion enlargement ever seen. Following the ratification of the Lisbon Treaty by all 27Member States in 2009, the importance of the Union as a major political player in the regionwill grow. Among the new challenges to be faced is maintaining a strong public healthposition in controlling and preventing HIV and HCV epidemics linked to drug use. This may26
Chapter 1: Harm reduction and the mainstream
be in a context of harsher economic conditions as well as increased migration, includingfrom countries with large HIV epidemics driven by drug injecting and where evidence-basedharm reduction measures are not always met with political commitment. The relative successof harm reduction strategies adopted in many European countries over the past two decades,and the evidence gathered in their support, provides a framework for the development,expansion and evaluation of harm reduction across multiple forms of substance use.
ReferencesNote: publications with three or more authors are listed chronologically, to facilitate the location of ‘et al.’references.Ashton, J. and Seymour, H. (1988),The new public health,Open University Press, Milton Keynes.Atun, R. and Kazathckine, M. (2010), ‘Translating evidence into action: challenges to scaling up harm reductionin Europe and Central Asia’, in Chapter 4, ‘Perspectives on harm reduction: what experts have to say’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Ball, A. (2007), ‘HIV, injecting drug use and harm reduction: a public health response’,Addiction102, pp. 684–90.Ball, A. (2010), ‘Broadening the scope and impact of harm reduction for HIV prevention, treatment and careamong injecting drug users’, in Chapter 4, ‘Perspectives on harm reduction: what experts have to say’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Bellis, D. J. (1981),Heroin and politicians: the failure of public policy to control addiction in America,GreenwoodPress, Westport, CT.Bewley-Taylor, D. (2004), ‘Harm reduction and the global drug control regime: contemporary problems andfuture prospects’,Drug and Alcohol Review23, pp. 483–9.Birkhead, G. S., Klein, S. J., Candelas, A. R., et al. (2007), ‘Integrating multiple programme and policyapproaches to hepatitis C prevention and care for injection drug users: a comprehensive approach’,InternationalJournal of Drug Policy18, pp. 417–25.Blankenship, K. M. and Koester, S. (2002), ‘Criminal law, policing policy, and HIV risk in female street sexworkers and injection drug users’,Journal of Law and Medical Ethics30, pp. 548–59.Blankenship, K. M., Friedman, S. R., Dworkin, S. and Mantell, J. E. (2006), ‘Structural interventions: concepts,challenges and opportunities for research’,Journal of Urban Health83, pp. 59–72.Bluthenthal, R. N., Lorvick J., Kral A. H., Erringer, E. A. and Kahn, J. G. (1999), ‘Collateral damage in the war ondrugs: HIV risk behaviors among injection drug users’,International Journal of Drug Policy10, pp. 25–38.Broadhead, R. S., Van Hulst, Y. and Heckathorn, D. D. (1999), ‘Termination of an established syringe-exchange:a study of claims and their impact’,Social Problems46, pp. 48–66.Burris, S., Donoghoe, M., Blankenship, K., et al. (2004), ‘Addressing the “risk environment” for injection drugusers: the mysterious case of the missing cop’,Milbank Quarterly82, pp. 125–56.Cooper, H., Moore, L., Gruskin, S. and Krieger, N. (2005), ‘The impact of a police drug crackdown on druginjectors’ ability to practice harm reduction’,Social Science and Medicine61, pp. 673–84.
27
Harm reduction: evidence, impacts and challenges
Cook, C., Bridge, J. and Stimson, G. V. (2010), ‘The diffusion of harm reduction in Europe and beyond’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Copenhaver, M., Johnson, B., Lee, I-C., et al. (2006), ‘Behavioral HIV risk reduction among people who injectdrugs: meta-analytic evidence of efficacy’,Journal of Substance Abuse Treatment31, pp. 163–71.Council of the European Union (2003), ‘Council Recommendation of 18 June 2003 on the prevention andreduction of health-related harm associated with drug dependence (2003/488/EC)’. Available at http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CELEX:32003H0488:EN:HTML.Council of the European Union (2004),EU drugs strategy (2005–2012),CORDROGUE 77, 22 November 2004.Available at http://ec.europa.eu/justice_home/doc_centre/drugs/strategy/doc_drugs_strategy_en.htm.Craine, N., Hickman, M., Parry, J. V., et al. (2009), ‘Incidence of hepatitis C in drug injectors: the role ofhomelessness, opiate substitution treatment, equipment sharing, and community size’,Epidemiology and Infection137, pp. 1255–65.Davis, C., Burris, S., Metzger, D., Becjer, J. and Lunch, K. (2005), ‘Effects of an intensive street-level policeintervention on syringe exchange program utilization’,American Journal of Public Health95, pp. 223–36.Des Jarlais, D. C. (1995), ‘Harm reduction: a framework for incorporating science into drug policy’,AmericanJournal of Public Health85, pp. 10–12.Des Jarlais, D. C. and Semaan, S. (2009), ‘HIV prevention and psychoactive drug use: a research agenda’,Journal of Epidemiology and Community Health63, pp. 191–6.Des Jarlais, D. C., Perlis, T., Arasteh, K., et al. (2005), ‘Reductions in hepatitis C virus and HIV infections amonginjecting drug users in New York City’,AIDS19 (Supplement 3), pp. S20–5.Dolan, K., Kite, B., Aceijas, C., and Stimson, G. V. (2007), ‘HIV in prison in low income and middle incomecountries’,Lancet Infectious Diseases7, pp. 32–43.Donoghoe, M., Verster, A., Pervilhac, C. and Williams, P. (2008), ‘Setting targets for universal access to HIVprevention, treatment and care for injecting drug users (IDUs): towards consensus and improved guidance’,International Journal of Drug Policy19 (Supplement 1), pp. S5–14.ECOSOC (UN Economic and Social Council) (2009), ‘Economic and Social Council resolution E/2009/L.23adopted by the Council on 24 July 2009: Joint United Nations Programme on Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome (UNAIDS)’. Available at http://www.un.org/Docs/journal/asp/ws.asp?m=E/2009/L.23.Elovich, R. and Drucker, E. (2008), ‘On drug treatment and social control: Russian narcology’s great leapbackwards’,Harm Reduction Journal5, p. 23. DOI: 10.1186/1477-7517-5-23.EMCDDA (2009a),Annual report 2009: the state of the drugs problem in Europe,European Monitoring Centre forDrugs and Drug Addiction, Lisbon.EMCDDA (2009b),Drug offences: sentencing and other outcomes,European Monitoring Centre for Drugs andDrug Addiction, Lisbon.EMCDDA (2009c), Statistical bulletin, Table HSR-6, European Monitoring Centre for Drugs and Drug Addiction,Lisbon. Available at http://www.emcdda.europa.eu/stats09/hsrtab6.EMCDDA (2009d), Statistical bulletin, Table HSR-5, European Monitoring Centre for Drugs and Drug Addiction,Lisbon. Available at http://www.emcdda.europa.eu/stats09/hsrtab5.
28
Chapter 1: Harm reduction and the mainstream
EMCDDA (2009e), Statistical bulletin, Figure HSR-1, European Monitoring Centre for Drugs and Drug Addiction,Lisbon. Available at http://www.emcdda.europa.eu/stats09/hsrfig1.EMCDDA (2010),Injecting drug use in Europe,European Monitoring Centre for Drugs and Drug Addiction, Lisbon.Erickson, P. (1999), ‘Introduction: the three phases of harm reduction. An examination of emerging concepts,methodologies, and critiques’,Substance Use and Misuse34 (1), pp. 1–7.European Commission (2002),Implementation of EU-action plan on drugs 2000–2004: progress review for theMember States.Available at http://ec.europa.eu/justice_home/doc_centre/drugs/studies/doc/review_actplan_02_04_en.pdf.European Commission (2006),2006 progress review on the implementation of the EU drugs action plan (2005–2008),Commission Staff Working Document SEC (2006) 1803. Available at http://ec.europa.eu/justice_home/doc_centre/drugs/strategy/doc/sec_2006_1803_en.pdf.European Commission (2008),The report of the final evaluation of the EU drugs action plan 2005–2008,CommissionStaff Working Document (accompanying document to the Communication from the Commission to the Council andthe European Parliament on an EU drugs action plan 2009–2012) COM (2008) 567, SEC(2008) 2456. Availableat http://ec.europa.eu/health/ph_determinants/life_style/drug/documents/COM2008_0567_a1_en.pdf.European Commission (2009),Report on global illicit drug markets, 2009.Available at http://ec.europa.eu/justice_home/doc_centre/drugs/studies/doc_drugs_studies_en.htm.Farrell, M., Gowing, L., Marsden, J., Ling, W. and Ali, R. (2005), ‘Effectiveness of drug dependence treatment inHIV prevention’,International Journal of Drug Policy16 (Supplement 1), pp. S67–75.Fletcher, A., Calafat, A., Pirona, A. and Olszewski, D. (2010), ‘Young people, recreational drug use and harmreduction’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence,impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, PublicationsOffice of the European Union, Luxembourg.Friedman, S. R., Cooper, H. L. F., Tempalski, B., et al. (2006), ‘Relationships between deterrence and lawenforcement and drug-related harm among drug injectors in U.S. metropolitan cities’,AIDS20, pp. 93–9.Friedman, S. R., Pouget, E. R., Chatterjee, S., et al. (2010), ‘Do drug arrests deter injection drug use?’ (in press).Gartner, C., Hall, W. and NcNeill, A. (2010), ‘Harm reduction policies for tobacco’, in European MonitoringCentre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts and challenges,Rhodes, T.and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of the European Union,Luxembourg.Gibson, D. R., Flynn, N. and Perales, D. (2001), ‘Effectiveness of syringe exchange programs in reducing HIV riskbehavior and HIV seroconversion among injecting drug users’,AIDS15, pp. 1329–41.Goldberg, D., Burns, S., Taylor, A., et al. (2001), ‘Trends in HCV prevalence among injecting drug users inGlasgow and Edinburgh during the era of needle/syringe exchange’,Scandinavian Journal of Infectious Diseases33, pp. 457–61.Grebely, J., Genoway, K., Khara, M., et al. (2007), ‘Treatment uptake and outcomes among current and formerinjection drug users receiving directly observed therapy within a multidisciplinary group model for the treatmentof hepatitis C virus infection’,International Journal of Drug Policy18: 437–43.Grund, J-P., Coffin, P., Jauffret-Roustide, M., et al. (2010), ‘The fast and furious: cocaine, amphetamines and harmreduction’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence,impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, PublicationsOffice of the European Union, Luxembourg.
29
Harm reduction: evidence, impacts and challenges
Hall, W. and Fischer, B. (2010), ‘Harm reduction policies for cannabis’, in European Monitoring Centre for Drugsand Drug Addiction (EMCDDA),Harm reduction: evidence, impacts and challenges,Rhodes, T. and Hedrich, D.(eds), Scientific Monograph Series No. 10, Publications Office of the European Union, Luxembourg.Hallinan, R., Byrne, A., Amin, J. and Dore, G. J. (2004), ‘Hepatitis C virus incidence among injecting drug userson opioid replacement therapy’,Australian and New Zealand Journal of Public Health28, pp. 576–8.Hartnoll, R., Gyarmarthy, A. and Zabransky, T. (2010), ‘Variations in problem drug use patterns and theirimplications for harm reduction’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harmreduction: evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No.10, Publications Office of the European Union, Luxembourg.Hedrich, D., Pirona, A. and Wiessing, L. (2008), ‘From margins to mainstream: the evolution of harm reductionresponses to problem drug use in Europe’,Drugs: education, prevention and policy15, pp. 503–17.Hedrich, D., Kerr, T. and Dubois-Arber, F. (2010), ‘Drug consumption facilities in Europe and beyond’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Herring, R., Thom, B., Beccaria, F., Kolind, T. and Moskalewicz, J. (2010), ‘Alcohol harm reduction in Europe’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Hickman, M. (2010), ‘HCV prevention: a challenge for evidence-based harm reduction’, in Chapter 4,‘Perspectives on harm reduction: what experts have to say’, in European Monitoring Centre for Drugs and DrugAddiction (EMCDDA),Harm reduction: evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds),Scientific Monograph Series No. 10, Publications Office of the European Union, Luxembourg.Human Rights Watch (2007),Rehabilitation required: Russia’s human rights obligation to provide evidence-baseddrug dependence treatment,Human Rights Watch, New York.Hunt, N., Albert, E. and Montañés Sánchez, V. (2010), ‘User involvement and user organising in harm reduction’,in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Institute of Medicine (2007),Preventing HIV infection among injecting drug users in high-risk countries: an assessmentof the evidence,National Academy of Sciences, Washington, DC.International Drug Policy Consortium (2009),The 2009 Commission on Narcotic Drugs and its high level segment:report of proceedings,Briefing Paper, IDPC, London.Jürgens, R., Ball, A. and Verster, A. (2009), ‘Interventions to reduce HIV transmission related to injecting drug usein prison’,Lancet Infectious Diseases9, pp. 57–66.Kerr, T., Small, W. and Wood, E. (2005), ‘The public health and social impacts of drug market enforcement: areview of the evidence’,International Journal of Drug Policy16, pp. 210–20.Kimber, J., Palmateer, N., Hutchinson, S., et al. (2010), ‘Harm reduction among injecting drug users: evidence ofeffectiveness’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction:evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10,Publications Office of the European Union, Luxembourg.Lancet(2009), ‘The future of harm reduction programmes in Russia’,Lancet374, p. 1213.
30
Chapter 1: Harm reduction and the mainstream
Lenton, S. and Single, E. (2004), ‘The definition of harm reduction’,Drug and Alcohol Review17, pp. 213–20.Lert, F. And Kazatchkine, M. (2007), ‘Antiretroviral HIV treatment and care for injecting drug users: an evidence-based overview’,International Journal of Drug Policy18, 255–61.Lindenburg, C. E. A., Krol, A., Smit, C., et al. (2006), ‘Decline in HIV incidence and injecting, but not in sexualrisk behaviour, seen in drug users in Amsterdam’,AIDS20, pp. 1771–5.MacGregor, S. and Whiting, M. (2010), ‘The development of European drug policy and the place of harmreduction within this’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction:evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10,Publications Office of the European Union, Luxembourg.Malta, M., Strathdee, S., Magnanini, M., et al. (2008), ‘Adherence to antiretroviral therapy for HIV among drugusers: a systematic review’,Addiction103, pp. 1242–57.Mathers, C. D. and Loncar, D. (2006), ‘Projections of global mortality and burden of disease from 2002 to2030’,PLoS Medicine3, pp. 2011–30.Miller, C., Firestone, M., Ramos, R., et al. (2008), ‘Injecting drug users’ experiences of policing practices in twoMexican–U.S. border cities’,International Journal of Drug Policy19, pp. 324–31.Montaner, J. S., Hogg, R., Wood, E., et al. (2006), ‘The case for expanding access to highly active antiretroviraltherapy to curb the growth of the HIV epidemic’,Lancet368, 531–6.Muga, R., Sanvisens, A., Bolao, F., et al. (2006), ‘Significant reductions of HIV prevalence but not of hepatitis Cvirus infections in injection drug users from metropolitan Barcelona: 1987–2001’,Drug and Alcohol Dependence82, Supplement 1, pp. S29–33.National Centre in HIV Epidemiology and Clinical Research UNSW (2009),Return on investment 2: evaluating thecost-effectiveness of needle and syringe programs in Australia 2009,Australian Government Department for Healthand Ageing. Available at http://www.health.gov.au/internet/main/publishing.nsf/Content/needle-return-2.Palepu, A., Tyndall, M. W., Joy, R., et al. (2006), ‘Antiretroviral adherence and HIV treatment outcomes amongHIV/HCV co-infected injection drug users: the role of methadone maintenance therapy’,Drug and AlcoholDependence84, pp. 188–94.Palmateer, N., Kimber, J., Hickman, M., et al. (2010), ‘Preventing hepatitis C and HIV transmission amonginjecting drug users: a review of reviews’,Addiction,in press.Peterson, A. and Lupton, D. (1996),The new public health: health and self in the age of risk,Sage Publications,Newbury Park, CA.Pollini, R. A., Brouwer, K. C., Lozada, R. M., et al. (2008), ‘Syringe possession arrests are associated withreceptive syringe sharing in two Mexico–U.S. border cities’,Addiction103, pp. 101–08.Rehm, J., Mathers, C., Popova, S., et al. (2009), ‘Global burden of disease and injury and economic costattributable to alcohol and alcohol-use disorders’,Lancet373, pp. 2223–32.Rehm, J., Fischer, B., Hickman, M., et al. (2010), ‘Perspectives on harm reduction: what experts have to say’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Rhodes, T. (2002), ‘The “risk environment”: a framework for understanding and reducing drug-related harm’,International Journal of Drug Policy13, pp. 85–94.
31
Harm reduction: evidence, impacts and challenges
Rhodes, T. (2009), ‘Risk environments and drug harms: a social science for harm reduction approach’,International Journal of Drug Policy20, pp. 193–201.Rhodes, T., Mikhailova, L., Sarang, A., et al. (2003), ‘Situational factors influencing drug injecting, risk reductionand syringe exchange in Togliatti City, Russian Federation: a qualitative study of micro risk environment’,SocialScience and Medicine57, pp. 39–54.Rhodes, T., Judd, A., Mikhailova, L., et al. (2004), ‘Injecting equipment sharing among injecting drug users inTogliatti City, Russian Federation: maximising the protective effects of syringe distribution’,Journal of AcquiredImmune Deficiency Syndromes35, pp. 293–300.Robson, G. and Marlatt, G. (2006), ‘Harm reduction and alcohol policy’,International Journal of Drug Policy17,pp. 255–7.Room, R. (2010), ‘The ambiguity of harm reduction: goal or means, and what constitutes harm?’, in Chapter 4,‘Perspectives on harm reduction: what experts have to say’, in European Monitoring Centre for Drugs and DrugAddiction (EMCDDA),Harm reduction: evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds),Scientific Monograph Series No. 10, Publications Office of the European Union, Luxembourg.Sarang, A., Rhodes, T., Platt, L., et al. (2006), ‘Drug injecting and syringe use in the HIV risk environment ofRussian penitentiary institutions’,Addiction101, pp. 1787–96.Sarang, A., Stuikyte, R. and Bykov, R. (2007), ‘Implementation of harm reduction in Central and Eastern Europeand Central Asia’,International Journal of Drug Policy18, pp. 129–35.Sarang, A., Rhodes, T. and Platt, L. (2008), ‘Access to syringes in three Russian cities: implications for syringedistribution and coverage’,International Journal of Drug Policy19, pp. S25–S36.Small, W., Kerr, T., Charette, J., Schechter, M. T. and Spittal, P. M. (2006), ‘Impacts of intensified police activityon injection drug users: evidence from an ethnographic investigation’,International Journal of Drug Policy17, pp.85–95.Spear, B. (1994), ‘The early years of the “British System” in practice’, in Strang, J. and Gossop, M. (eds)Heroinaddiction and drug policy,Oxford University Press, Oxford, pp. 3–28.Stevens, A., Stöver, H. and Brentari, C. (2010), ‘Criminal justice approaches to harm reduction in Europe’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Sweanor, D., Alcabes, P. and Drucker, E. (2007), ‘Tobacco harm reduction: how rational public policy couldtransform a pandemic’,International Journal of Drug Policy,18, pp. 70–4.Sylla, L., Douglas Bruce, R., Kamarulzaman, A. and Altice, F. L. (2007), ‘Integration and co-location of HIV/AIDS,tuberculosis and drug treatment services’,International Journal of Drug Policy18, pp. 306–12.United Nations Development Program (2008),Living with HIV in Eastern Europe and the CIS,UNDP, Bratislava.United Nations General Assembly Sixtieth Special Session (2006),Political declaration on HIV/AIDS.Resolution60/262 adopted by the United Nations General Assembly, United Nations, New York.UNODC (United Nations Office on Drugs and Crime) (2009),A century of international drug control,UNODC,Vienna. Available at http://www.unodc.org/documents/data-and-analysis/Studies/100_Years_of_Drug_Control.pdf.van den Berg, C., Smit, C., Van Brussel, G., Coutinho, R. A. and Prins, M. (2007), ‘Full participation in harmreduction programmes is associated with decreased risk for human immunodeficiency virus and hepatitis C virus:evidence from the Amsterdam cohort studies among drug users’,Addiction102, pp. 1454–62.
32
Chapter 1: Harm reduction and the mainstream
van der Gouwe, D., Gallà, M., Van Gageldonk, A., Croes, E., Engelhardt, J., Van Laar, M. and Buster, M.(2006),Prevention and reduction of health-related harm associated with drug dependence: an inventory of policies,evidence and practices in the EU relevant to the implementation of the Council Recommendation of 18 June 2003.Synthesis report. Contract nr. SI2.397049,Trimbos Instituut, Utrecht. Available at http://ec.europa.eu/health/ph_determinants/life_style/drug/documents/drug_report_en.pdf.Vickerman, P. and Hickman, M. (2010), ‘The effect of epidemiological setting on the impact of harm reductiontargeting injecting drug users’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harmreduction: evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No.10, Publications Office of the European Union, Luxembourg.Werb, D., Wood, E., Small, W., et al. (2008), ‘Effects of police confiscation of illicit drugs and syringes amonginjection drug users in Vancouver’,International Journal of Drug Policy19, pp. 332–8.WHO (World Health Organization) (1974),Expert committee on drug dependence: twentieth report,TechnicalReport Series 551, WHO, Geneva.WHO (1986),Ottawa Charter for Health Promotion,WHO, Geneva, WHO/HPR/HEP/95.1.WHO (2009),HIV/AIDS: comprehensive harm reduction package,WHO, Geneva. Available at http://www.who.int/hiv/topics/idu/harm_reduction/en/index.html.WHO, UNODC and UNAIDS (Joint United Nations Programme on HIV/AIDS) (2008),Policy guidelines forcollaborative HIV and TB services for injecting and other drug users,WHO, Geneva. Available at http://www.who.int/tb/publications/2008/en/index.html.WHO, UNODC and UNAIDS (2009), ‘Technical guide for countries to set targets for universal access to HIVprevention, treatment and care for injecting drug users. Available at http://www.who.int/hiv/pub/idu/targetsetting/en/index.html.Wiessing, L., Van de Laar, M.J., Donoghoe, M.C., et al. (2008), ‘HIV among injecting drug users in Europe:increasing trends in the East’,Eurosurveillance3 (50). Available at http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19067.Wiessing, L., Likataviˇ ius, G., Klempová, D., et al. (2009), ‘Associations between availability and coverage ofcHIV-prevention measures and subsequent incidence of diagnosed HIV infection among injection drug users’,American Journal of Public Health99 (6), pp. 1049–52.Wodak, A. and Cooney, A. (2005), ‘Effectiveness of sterile needle and syringe programmes’,InternationalJournal of Drug Policy16, Supplement 1, pp. S31–44.Wolfe, D. and Malinowska-Sempruch, K. (2004),Illicit drug policies and the global HIV epidemic,Open SocietyInstitute, New York.Wood, E., Spittal, P. M., Li, K., et al. (2004), ‘Inability to access addiction treatment and risk of HIV-infectionamong injection drug users’,Journal of Acquired Immune Deficiency Syndromes36, pp. 750–4.Wood, E., Werb, D., Marshall, B., Montaner, J. S. G. and Kerr, T. (2009), ‘The war on drugs: a devastatingpublic-policy disaster’,Lancet373, pp. 989–90.Wright, N. M. and Tompkins, C. N. (2006), ‘A review of the evidence for the effectiveness of primary preventioninterventions for hepatitis C among injecting drug users’,Harm Reduction Journal6 (3), p. 27.Zaric, G. S., Barnett, P. G. and Brandeau, M. L. (2000), ‘HIV transmission and the cost-effectiveness ofmethadone maintenance’,American Journal of Public Health90 (7), pp.1100–11.
33
Background
PARTI
Chapter 2The diffusion of harm reduction in Europe and beyondCatherine Cook, Jamie Bridge and Gerry V. Stimson
AbstractThis chapter traces the diffusion of harm reduction in Europe and around the world. The term‘harm reduction’ became prominent in the mid-1980s as a response to newly discovered HIVepidemics amongst people who inject drugs in some cities. At this time, many European citiesplayed a key role in the development of innovative interventions such as needle and syringeprogrammes. The harm reduction approach increased in global coverage and acceptancethroughout the 1990s and became an integral part of drug policy guidance from theEuropean Union at the turn of the century. By 2009, some 31 European countries supportedharm reduction in policy or practice — all of which provided needle and syringeprogrammes and opioid substitution therapy. Six countries also provided prison needle andsyringe programmes, 23 provided opioid substitution therapy in prisons, and all but two ofthe drug consumption rooms in the world were in Europe. However, models and coveragevary across the European region. Harm reduction is now an official policy of the UnitedNations, and Europe has played a key role in this development and continues to be a strongvoice for harm reduction at the international level.Keywords:history, harm reduction, global diffusion, international policy, Europe.
IntroductionThe term ‘harm reduction’ refers to ‘policies, programmes and practices that aim to reducethe adverse health, social and economic consequences of the use of legal and illegalpsychoactive drugs’, and are ‘based on a strong commitment to public health and humanrights’ (IHRA, 2009a, p. 1). The term came to prominence after the emergence of HIV inEurope and elsewhere in the mid-1980s (Stimson, 2007). However, the underlyingprinciples of this approach can be traced back much further (see box on p. 38). Thischapter seeks to explore the emergence and diffusion of harm reduction from a localised,community-based response to international best practice. Since space restricts anexhaustive history transcending all aspects of harm reduction, we will focus primarily onthe development and acceptance of approaches to prevent HIV transmission amongstpeople who inject drugs. It is these interventions that have come to epitomise the essence ofharm reduction. For the purposes of this chapter, Europe is defined as comprising 33countries — the 27 Member States of the European Union (EU), the candidate countries(Croatia, the Former Yugoslav Republic of Macedonia and Turkey), and Norway,Switzerland and Iceland.37
Harm reduction: evidence, impacts and challenges
Early examples of ‘harm reduction’ principles and practice1912 to 19231926Narcotic maintenance clinics in the United States.Report of the United Kingdom Departmental Committee on Morphine andHeroin Addiction (the Rolleston Committee) concluded in support of opiateprescription to help maintain normality for heroin-dependent patients.Emergence of ‘controlled drinking’ as an alternative to abstinence-basedtreatments for some alcohol users.Grass-roots work on reducing harms connected to the use of LSD, cannabis,amphetamines, and to glue sniffing.
1960s1960s on
The diffusion of harm reduction in EuropeIn 1985 HIV antibody tests were introduced, leading to the discovery of high rates ofinfection in numerous European cities among people who inject drugs — includingEdinburgh (51 %) (Robertson et al., 1986), Milan (60 %), Bari (76 %), Bilbao (50 %), Paris(64 %), Toulouse (64 %), Geneva (52 %) and Innsbruck (44 %) (Stimson, 1995). These localisedepidemics occurred in a short space of time, with 40 % or more prevalence of infectionreached within two years of the introduction of the virus into drug-injecting communities(Stimson, 1994). Analysis of stored blood samples indicated that HIV was first present inAmsterdam in 1981, and in Edinburgh one or two years later (Stimson, 1991). Heroin useand drug injecting in European countries had been on the increase since the 1960s (Hartnollet al., 1989) and research indicated that the sharing of needles and syringes was commonamongst people who injected drugs (Stimson, 1991).It soon became evident that parts of Europe faced a public health emergency (see boxbelow). Across Europe, the response was driven at a city level by local health authorities andcivil society (sometimes in spite of interference from government) (O’Hare, 2007a). In 1984(one year before the introduction of HIV testing), drug user organisations in the Netherlandsstarted to distribute sterile injecting equipment to their peers to counter hepatitis Btransmission (Buning et al., 1990; Stimson, 2007). This is widely acknowledged as the firstformal needle and syringe programme (NSP), although informal or ad hoc NSPs existedaround the world before 1984. Soon after, the Netherlands integrated NSPs within low-threshold centres nationwide (Buning et al., 1990).The transformation brought by HIV and harm reductionHIV and AIDS provide the greatest challenges yet to drug policies and services. Policy-makersand practitioners … have been forced to reassess their ways of dealing with drug problems;this includes clarifying their aims, identifying their objectives and priorities for their work, theirstyles of working and relationships with clients, and the location of the work. Within the spaceof about three years, mainly between 1986 and 1988, there have been major debates aboutHIV, AIDS and injecting drug use. In years to come, it is likely that the late 1980s will beidentified as a key period of crisis and transformation in the history of drugs policy.(Stimson, 1990b)
38
Chapter 2: The diffusion of harm reduction in Europe and beyond
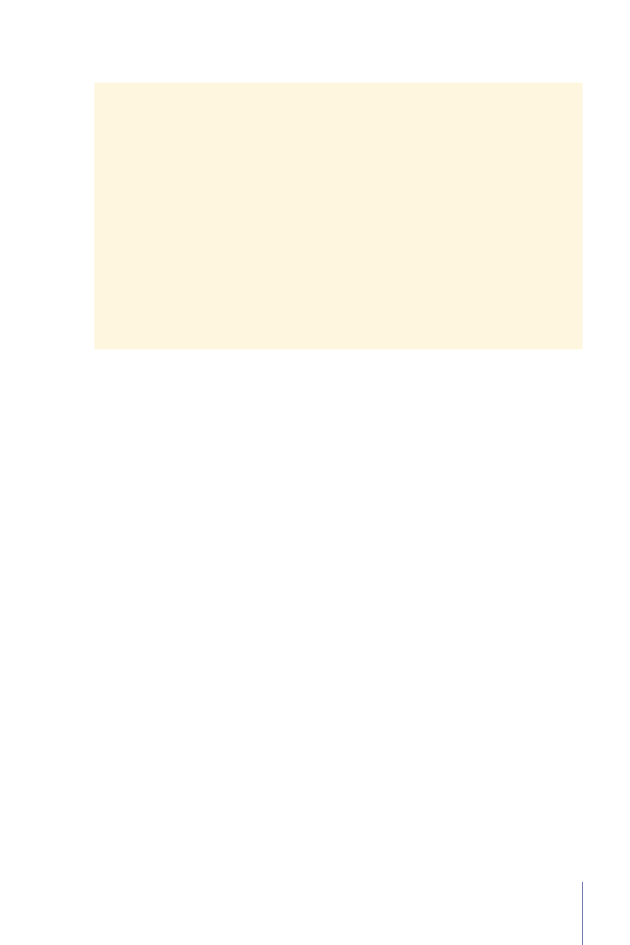
In 1986, parts of the United Kingdom introduced NSPs (Stimson, 1995; O’Hare, 2007b). By1987, similar programmes had also been adopted in Denmark, Malta, Spain and Sweden(Hedrich et al., 2008). By 1990, NSPs operated in 14 European countries, and were publiclyfunded in 12. This had increased to 28 countries by the turn of the century, with public fundssupporting programmes in all but one of these (EMCDDA, 2009a, Table HSR-4). Somecountries were also experimenting with alternative models of distribution, including syringevending machines and pharmacy-based schemes (Stimson, 1989). By the early 1990s, therewas growing evidence of the feasibility of NSPs and in support of the interventions’ ability toattract into services otherwise-hidden populations of people who inject drugs, and reducelevels of syringe sharing (Stimson, 1991).Figure 2.1:Year of introduction of opioid substitution treatment (OST) and official introduction ofneedle and syringe programmes (NSPs) in EU countries
3025201510501965OSTNSP
1970
1975
1980
1985
1990
1995
2000
2005
Note: The data represent the official introduction of OST, and the availability of publicly funded NSPs.Source:Reitox national focal points.
The spread of NSPs in Europe in the late 1980s and throughout the 1990s was the result ofbroader policy shifts away from the treatment of dependence and towards the management ofthe health of people who used drugs (Stimson and Lart, 1990). A focus on health and its riskmanagement increased the emphasis on low-threshold access to services and community-basedinterventions. Outreach, and especially peer-driven outreach, epitomised these shifts (Rhodesand Hartnoll, 1991; Rhodes, 1993). No longer were services solely reliant upon drug usersseeking help for treatment, but instead they reached out to those most hidden and vulnerable asa means of reducing population-wide drug-related risk. In many instances, harm reduction wascoordinated at the community or city level (Huber, 1995; Hartnoll and Hedrich, 1996).These shifts enabled the reshaping of prescribing and drug treatment services towards amore ‘user friendly’ and collaborative model. The practice of prescribing opiates to peopledependent on them had been widely adopted as early as the 1920s in the United Kingdom(Department Committee on Morphine and Heroin Addiction, 1926; Stimson and39
Harm reduction: evidence, impacts and challenges
Oppenheimer, 1982). Methadone maintenance treatment (MMT) was introduced in Europe inthe 1960s; first in Sweden, then in the Netherlands, the United Kingdom, and Denmark(Hedrich et al., 2008), albeit with limited provision and often in the context of abstinence-orientated programmes. The emergence of HIV in the mid-1980s served to reinvigorate thisintervention, combining it with outreach-based models, such as the‘methadone by bus’project in Amsterdam (Buning et al., 1990).The number of European countries with MMTrapidly increased throughout the 1990s (see Figure 2.1).By the 1990s, harm reduction was becoming endorsed as part of national drug policies inmany European countries, although some were slower to follow suit (including Germany,Greece and France, which maintained abstinence-based policies) (Michels et al., 2007;Stimson, 1995; Bergeron and Kopp, 2002). It took over a decade, however, for the EU toagree, for the first time, a ‘Drugs strategy’ (European Union, 2000a) with an associated‘Action plan’ (European Union, 2000b), for the period 2000–04, containing a number ofconcrete targets. National drug policies across Europe have always been the individualresponsibility of Member States, and as such the EU’s role is a ‘co-ordinating, complementaryand supporting one’ (Hedrich et al., 2008), creating frameworks rather than legally bindinginstruments. This first EU drugs strategy presented six recommended targets, one of whichwas ‘to reduce substantially over five years the incidence of drug-related health damage(including HIV and hepatitis) and the number of drug-related deaths’ (European Union,2000a). Although the document did not explicitly use the term harm reduction, this targetrepresents an important milestone in European drug policy.The next milestone came in 2003, when the Council of the European Union adopted arecommendation on the prevention and reduction of health-related harm associated withdrug dependence. This stated that Member States should set the reduction of drug-relatedrisks as a public health objective and listed some of the key harm reduction measures to‘reduce substantially the incidence of drug-related health damage’ (see box below). In 2004a new eight-year EU drugs strategy (2005–12) was adopted, which explicitly aimed for a‘Measurable reduction of ... drug-related health and social risks’ through a comprehensivesystem ‘including prevention, early intervention, treatment, harm reduction, rehabilitation andsocial reintegration measures within the EU Member States’ (European Union, 2004).Council Recommendation of 18 June 2003 on the prevention and reduction of health-relatedharm associated with drug dependence (COM 2003/488/EC)Member States should, in order to reduce substantially the incidence of drug-related healthdamage (such as HIV, hepatitis B and C and tuberculosis) and the number of drug-relateddeaths, make available, as an integral part of their overall drug prevention and treatmentpolicies, a range of different services and facilities, particularly aiming at risk reduction; tothis end, bearing in mind the general objective, in the first place, to prevent drug abuse,Member States should:1. provide information and counselling to drug users to promote risk reduction and to facilitatetheir access to appropriate services;
40
Chapter 2: The diffusion of harm reduction in Europe and beyond
2. inform communities and families and enable them to be involved in the prevention andreduction of health risks associated with drug dependence;3. include outreach work methodologies within the national health and social drug policies,and support appropriate outreach work training and the development of working standardsand methods; outreach work is defined as a community-oriented activity undertaken inorder to contact individuals or groups from particular target populations, who are noteffectively contacted or reached by existing services or through traditional health educationchannels;4. encourage, when appropriate, the involvement of, and promote training for, peers andvolunteers in outreach work, including measures to reduce drug-related deaths, first aidand early involvement of the emergency services;5. promote networking and cooperation between agencies involved in outreach work, topermit continuity of services and better users’ accessibility;6. provide, in accordance with the individual needs of the drug abuser, drug-free treatmentas well as appropriate substitution treatment supported by adequate psychosocial careand rehabilitation, taking into account the fact that a wide variety of different treatmentoptions should be provided for the drug-abuser;7. establish measures to prevent diversion of substitution substances while ensuring appropriateaccess to treatment;8. consider making available to drug abusers in prison access to services similar to thoseprovided to drug abusers not in prison, in a way that does not compromise the continuousand overall efforts of keeping drugs out of prison;9. promote adequate hepatitis B vaccination coverage and prophylactic measures againstHIV, hepatitis B and C, tuberculosis and sexually transmitted diseases, as well as screeningfor all the aforementioned diseases among injection drug users and their immediate socialnetworks, and take the appropriate medical actions;10. provide where appropriate, access to distribution of condoms and injection materials,and also to programmes and points for their exchange;11. ensure that emergency services are trained and equipped to deal with overdoses;12. promote appropriate integration between health, including mental health, and socialcare, and specialised approaches in risk reduction;13. support training leading to a recognised qualification for professionals responsible forthe prevention and reduction of health-related risks associated with drug dependence.(Council of the European Union, 2003)
41
Harm reduction: evidence, impacts and challenges
During this time, the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA)established itself as a core instrument for the monitoring of evidence related to patterns of druguse and policy in the EU. Founded in 1993, and building upon work by the Pompidou Group ofthe Council of Europe, the EMCDDA generated the first EU-wide overviews of harm reductionactivity at the turn of the century (for example, EMCDDA, 2000). As the EU grew, newerMember States began to develop national drug monitoring systems to feed into this process. Inaddition, it has been argued that ‘there is clear evidence that “EU drugs guidance” was a modelfor national policies’ for newer Member States (Commission of the European Communities,2007; Hedrich et al., 2008, p. 513). By 2009, there was explicit support for harm reduction innational policy documents in all 27 EU Member States, as well as in Croatia, the FormerYugoslav Republic of Macedonia, Norway and Switzerland (Cook, 2009). This convergencetowards a ‘common position’ (Hedrich et al., 2008, p. 513) has allowed the EU to be a strongadvocate for harm reduction at international fora (see also MacGregor and Whiting, 2010).
The diffusion of harm reduction beyond EuropeIn Australia, medical experts learned of NSPs in the Netherlands through a letter in themedical journalThe Lancet,and in 1985 ‘harm minimisation’ was universally adopted as anational policy (Wellbourne-Wood, 1999). In 1987, the Canadian Government adopted harmreduction as the framework for the National Drug Strategy (Canadian AIDS Society, 2000),and in the United States the first NSPs appeared before 1988 despite long-standing federalopposition to policies of harm reduction (Sherman and Purchase, 2001; Lane, 1993; Watters,1996). In many US states, in the absence of legally endorsed needle and syringe distribution,some activist groups also began distributing bleach for cleaning syringes (Watters, 1996;Moss, 1990). The first harm reduction project in Latin America started in Brazil in 1989(Bueno, 2007). Three years later, the HIV/AIDS Prevention Program for Drug Users wasestablished in Buenes Aires. Touze et al. (1999) attributes ‘the increasing amount ofinformation on international harm reduction experiences in the mass media’ as one of fivecontributory factors to the adoption of harm reduction in Argentina.Much international attention was focused on selected European cities, especially Amsterdam(where a city official was hired to manage the demand for visits), and Liverpool, whichhosted the first ‘International Conference on the Reduction of Drug Related Harm’ in 1990(O’Hare, 2007b). In the same year, Frankfurt also hosted the first ‘Conference of EuropeanCities in the Centre of the Drug Trade’. New networks and alliances of cities and experts wereemerging within and beyond Europe (including, in 1996, the International Harm ReductionAssociation). Bilateral funding and support from European governments also began to focuson harm reduction in the developing world (for example, the Asian Harm Reduction Networkwas founded in 1996 with support from the Dutch Government).At a global level, the World Health Organization (WHO) was one of the first multilateralbodies to endorse the underlying principles of harm reduction in a meeting in Stockholm in1986 (WHO, 1986). As early as 1974, the WHO Expert Committee on Drug Dependencehad made reference to ‘concern for preventing and reducing problems rather than just druguse’ (Wodak, 2004). Other agencies of the United Nations system — including UNAIDS (theJoint United Nations Programme on HIV/AIDS, established in 1996) — showed greater42
Chapter 2: The diffusion of harm reduction in Europe and beyond
reticence or ambiguity. Since the turn of the century, however, harm reduction appears firmlyentrenched in the international policy dialogue (United Nations General Assembly, 2001;International Harm Reduction Association, 2009b).In 2001, a meeting of the United Nations (UN)General Assembly (the chief policy-makingbody of the United Nations) adopted a ‘Declaration of Commitment’, which explicitly statedthat ‘harm reduction efforts related to drug use’ should be implemented by Member States(United Nations General Assembly, 2001). Two years later, the WHO commissioned a reviewof scientific evidence on the effectiveness of harm reduction interventions targeting peoplewho inject drugs, which was published in 2005 (WHO, 2005a; Wodak and Cooney, 2005;Farrell et al., 2005; Needle et al., 2005). That same year, methadone and buprenorphinewere added to the WHO list of ‘essential medicines’ (WHO, 2005b), and UNAIDS releaseda position paper entitled ‘Intensifying HIV Prevention’ that listed a core package of harmreduction interventions (UNAIDS, 2005a) — later expanded to become the ‘comprehensiveharm reduction package’ (WHO, 2009).In December 2005, the UN General Assembly adopted a resolution requesting that UNAIDSassist in ‘scaling-up HIV prevention, treatment, care and support with the aim of coming asclose as possible to the goal of universal access to treatment by 2010 for all those who needit’ (United Nations General Assembly, 2006). This led to the development of WHO, UNAIDSand UNODC guidelines on national target setting and programming on HIV prevention,treatment and care for injecting drug users, and focused advocacy efforts on the need forgreater coverage towards ‘universal access’ (Donoghoe et al., 2008).In contrast to the United Nations’ HIV/AIDS response, there has been notably less support forharm reduction from the various UN drug control agencies. Within the UNAIDS programme,UNODC is the lead agency on the ‘Prevention of transmission of HIV among injecting drugusers and in prisons’ (UNAIDS, 2005b) but this role remains overshadowed by its parallel remitto control the production and supply of illicit drugs. In addition, UNODC’s governing body —the Commission on Narcotic Drugs (CND) — has seen ongoing resistance to harm reductionfrom some countries (including Japan, Russia and the United States), creating incoherence on aglobal policy position for harm reduction across the UN system (Hunt, 2008). The InternationalNarcotics Control Board (the expert advisory body monitoring compliance with the UN DrugConventions) has also regularly questioned the legality of some harm reduction interventions(Csete and Wolfe, 2007). Most recently, in 2009, CND adopted a draft ten-year ‘PoliticalDeclaration’ on drug control that (after months of negotiation and despite advocacy effortsfrom civil society, the UNAIDS Executive Director, and two UN Special Rapporteurs) resistedrequests to include the term harm reduction (United Nations Commission on Narcotic Drugs,2009; see also MacGregor and Whiting, 2010). Despite this, however, there were 84 countriesaround the world supporting harm reduction in either policy or practice by 2009, spanningevery continent and including 31 European countries (Cook, 2009).
Current harm reduction practice in EuropeEurope remains one of the regions most supportive of harm reduction policy and practice,including through bilateral support from European governments to programmes in low- and43
Harm reduction: evidence, impacts and challenges
middle-income countries. Yet there is still considerable variation within Europe in the extentand nature of harm reduction, and the coverage these interventions achieve among targetedpopulations (see Table 2.1, Figure 2.2 and Figure 2.3). We synthesise here current harmreduction practices in Europe, focusing on access to sterile injecting equipment, opioidsubstitution treatment and drug consumption rooms (DCRs) (see also Donoghoe et al., 2008;Aceijas et al., 2007; Kimber et al., 2010; Hedrich et al., 2010).Access to sterile injecting equipment in EuropeBy 2009, there were 77 countries and territories worldwide with at least one operationalNSP, and 31 of these countries were European (Cook, 2009). With the exception of Icelandand Turkey, every European country where injecting drug use had been reported had one ormore NSP (see Table 2.1). The most recent EU Member to begin providing sterile injectingequipment to people who inject drugs was Cyprus in 2007. Across the region, sterile injectingequipment is delivered through community-based specialist drugs services, pharmacies andoutreach (including peer outreach), although not all service delivery models are employed inall countries. For example, access to free injecting equipment is only available throughpharmacies in Northern Ireland, and two hospital-based outlets in Sweden (EMCDDA,2009a, Table HSR-4). Syringe sales are legal in all countries, except in Sweden.In 2007, subsidised pharmacy-based syringe distribution was available in 12 countries:Austria, Belgium, Croatia, Czech Republic, Denmark, France, Greece, the Netherlands,Portugal, Slovenia, Spain and the United Kingdom. Seven countries also used syringevending machines (Austria, Denmark, France, Germany, Hungary, Italy and Luxembourg)and several had mobile service provision (EMCDDA, 2009a, Table HSR-4).
Table 2.1:Harm reduction practice in EuropeCountryPrison opioidPrisonDrugNeedle and Opioidsubstitution consumption needle and substitutionsyringetherapysyringeroomsprogrammes therapyprogrammes
AustriaBelgiumBulgariaCroatiaCyprusCzech RepublicDenmarkEstoniaFinlandFrance
44
Chapter 2: The diffusion of harm reduction in Europe and beyond
Table 2.1(continued)CountryPrison opioidPrisonDrugNeedle and Opioidsubstitution consumption needle and substitutionsyringetherapysyringeroomsprogrammes therapyprogrammes
GermanyGreeceHungaryIcelandIrelandItalyLatviaLithuaniaLuxembourgFormer YugoslavRepublic ofMacedoniaMaltaNetherlandsNorwayPolandPortugalRomaniaSlovakiaSloveniaSpainSwedenSwitzerlandTurkeyUnited Kingdom
Source:Adapted from Cook, 2009.
Cross-country comparisons of coverage require robust reporting systems and harmonisedindicators. While more robust than the data estimates available in other regions of the world,information remains unavailable for some European countries and patchy in others(EMCDDA, 2009a, Table HSR-5). In addition, estimating intervention ‘coverage’ — theproportion of target populations reached by harm reduction interventions, ideally withsufficient intensity to have probable impact — requires estimates of target populationprevalence and intervention dose that are often unavailable or of dubious reliability (Heimer,2008; Aceijas et al., 2007; Sharma et al., 2008). While most European countries have45
Harm reduction: evidence, impacts and challenges
estimates of the prevalence of problem drug use, far fewer have specific estimates of theprevalence of drug injecting (EMCDDA, 2009a, Table PDU-1).Available data indicates substantial variation in NSP coverage across the region (Figure 2.2).Even when comparing the number of NSP sites nationwide, an indicator that does not takeinto account the size of injecting populations, or factors impeding service access, they varyfrom several thousand (France), several hundred (United Kingdom, Portugal, Spain) to fewerthan five (Cyprus, Greece, Romania and Sweden) (Cook and Kanaef, 2008). A number ofEuropean countries are providing over 150 syringes per injector per year through specialistNSPs (for example, the Czech Republic, Portugal, Norway and Luxembourg) (EMCDDA,2010) — levels of coverage that may contribute to the aversion or reduction of HIV epidemics(Vickerman et al., 2006). However, this is by no means consistent throughout Europe, andcoverage is almost negligible in some countries (Figure 2.2). In Sweden (one of the firstcountries to establish NSPs in Europe), there are only two NSP sites, and the interventionreaches approximately 1 200 people; just 5 % of the estimated total number of people whoinject drugs in the country (Svenska Brukarföreningen et al., 2007; Olsson et al., 2001).In addition, national NSP coverage estimates often hide dramatic geographical coveragevariations, with provision in many cities, towns and rural areas woefully inadequate. InFrance, for example, there are no specialist drugs facilities with NSPs in some cities with apopulation over 100 000 and with known injecting drug use (ASUD, 2008).Figure 2.2:Syringes distributed through specialised programmes, per estimated IDU per year(2002–07)400350300Number of syringes250200B150100500BCyprusBGreeceBCroatiaBLatviaBSlovakiaBHungaryBCzech RepublicLuxembourgPortugalNorwayMaltaBBBB
Source:EMCDDA, 2010.
46
Estonia
Chapter 2: The diffusion of harm reduction in Europe and beyond
Figure 2.2 illustrates that many people injecting drugs in Europe have inadequate access tosubsidised or free syringes from NSPs. In several countries, current coverage levels are nothigh enough to avert or reverse an HIV epidemic in the IDU population (Vickerman et al.,2006; Heimer et al., 2008). It should be noted, however, that pharmacy sales of injectingequipment are not captured in Figure 2.2 and may be a common source of syringes for somepeople using drugs in the region.Several countries have larger numbers of non-specialist pharmacy-based NSPs than specialistagencies (EMCDDA, 2006, Table NSP-1), and some (for example, Northern Ireland andSweden) rely only on one type of outlet. Specialist NSPs, however, may provide more thanneedles and syringes alone, including a greater intensity of harm reduction advice andeducation, referrals into drug and HIV treatment, and a wider range of injecting equipment(including ‘spoons’ or ‘cookers’, water, filters, alcohol pads, tourniquets, condoms, acidicpowders for dissolving drugs, and aluminium foil or inhalation pipes to assist ‘route transitions’from injecting to smoking). Among the common developments in Europe is a diversification ofoutlets for needle and syringe exchange, which also provides a basis for scaling up syringeprovision. In most countries several types of legal syringe sources, including NSPs, pharmaciesand mobile units, are available to meet the needs of people who inject drugs.Access to sterile injecting equipment in European prisonsDespite evidence-based reviews of effectiveness and recommendations for implementation(WHO, 2005a; Kimber et al., 2010), only 10 countries worldwide have introduced needleand syringe programmes (NSPs) in prisons. Six of these countries are European: Germany,Luxembourg, Portugal, Romania, Spain and Switzerland. The first prison NSP was introducedin Switzerland in 1992, followed four years later by Germany, and then Spain in 1997.Service models vary between prisons and include ‘one-to-one’ exchanges implemented bymedical staff, exchanges operated by external NGOs or by peer workers, and the use ofautomated syringe vending machines.The number of prisoners with access to this intervention varies across the region, but only inSpain have syringe programmes been made available across a national prison system. Inrecent years, Spain has scaled-up the availability, while in Germany a change in governmentled to the closure of six prison-based syringe programmes, leaving only one (WHO, 2005c).In 2009, Belgium and Scotland were in the process of developing pilot programmes.Researchers on this issue have concluded that the poor availability of this intervention inEurope ‘cannot be based on logic’ (Stöver et al., 2008a, p. 94).Drug consumption rooms in EuropeWith the exception of one Canadian and one Australian facility, all DCRs are operating inEuropean countries (see Hedrich et al., 2010). Germany, Luxembourg, the Netherlands, Norway,Spain and Switzerland have an estimated 90 DCRs collectively, spanning 59 European cities(with the majority in the Netherlands and Germany). These facilities, which are usuallyintegrated into low-threshold drugs agencies, allow the smoking and/or injecting of drugs under47
Harm reduction: evidence, impacts and challenges
supervision by trained staff and without fear of arrest. In 2007 there were an estimated 13 727,supervised consumptions in Luxembourg’s sole DCR and 11 600 in Norway’s single facility. InGermany, large numbers of supervised consumptions occurred in Frankfurt (171 235 in 2007),Berlin (12 000 in 2006) and Hannover (29 332 in 2006). Despite positive evaluations, thesefacilities remain controversial both within Europe and elsewhere (Hedrich et al., 2010).Access to opioid substitution treatment in EuropeBy 2009, there were 65 countries and territories worldwide that provided opioid substitutiontreatment (OST) for drug dependence, almost half of which were in Europe (Cook, 2009). AllEuropean countries where injecting drug use is reported, with the exception of Iceland and Turkey,prescribe methadone and/or buprenorphine as treatment for opioid dependence (see Table 2.1).In 2007, more than 650 000 opioid users were estimated to have received OST in Europe,with huge national variations in coverage (EMCDDA, 2009b). England and Wales, Italy andFrance were each prescribing the treatment to more than 100 000 people. Methadone is themost commonly prescribed OST medicine across the region, with the exceptions of Croatia,the Czech Republic, Cyprus, France, Finland, Latvia and Sweden, where high-dosagebuprenorphine is used and Austria, where slow-release morphine is used more often(EMCDDA, 2009a, Table HSR-3). In general, the volume of OST prescribing increasedbetween 2003 and 2007, with the most dramatic increases in Bulgaria, the Czech Republic,Estonia, Finland, Latvia and Norway. Decreases have been reported in Spain and astabilisation of the demand for OST seemed also to take place in France, Luxembourg andthe Netherlands (see EMCDDA, 2009a, HSR Tables).Figure 2.3:Opioid maintenance treatment clients as a percentage of the estimated number ofproblem opioid users, 2007 or most recent year available90Opioid maintenance treatment clients (%)80706050403020100CyprusSlovakiaPolandGreeceFinlandMaltaAustriaCzechRepublicGermanyItaly
Source:EMCDDA, 2009b.
48
Chapter 2: The diffusion of harm reduction in Europe and beyond
The coverage of OST provision varies greatly across the region. While countries such as Spainand the United Kingdom have large numbers of OST sites (2 229 and 1 030 respectively;EMCDDA, 2009c; United Kingdom National Treatment Agency, 2007), at least 10 Europeancountries have fewer than 20 sites providing OST (EMCDDA, 2009c). Where estimates of theprevalence of problem drug use and data on clients in substitution treatment are available, thecoverage of OST can be calculated (see Figure 2.3). While these estimates must be interpretedwith caution due to uncertainties in both values, the results indicate significant variations incoverage across the EU — from 5 % in Cyprus and Slovakia to around 50 % in the CzechRepublic, Germany and Italy. In a recent UN target-setting guide, reaching 40 % or more ofpeople using opioids problematically with OST is cited as ‘good coverage’ (WHO et al., 2009).Even where OST is available, several factors influence the effective utilisation of services.Long waiting lists, limited treatment slots, strict adherence policies, and an unwillingness ofgeneral practitioners to prescribe OST are all reported to impact upon accessibility inEuropean countries. The costs attached to OST, the lack of ‘take-home’ doses and, in somecases, the need for medical insurance also act as barriers (Cook and Kanaef, 2008).A number of European countries have remained at the forefront of innovation with regards toOST and drug dependence therapies. For those who cannot or do not wish to stop injecting,a small number of European countries prescribe injectable OST medicines (including theNetherlands, Switzerland and the United Kingdom) (Cook and Kanaef, 2008). Theprescription of pharmaceutical heroin (diacetylmorphine) remains limited to a few Europeancountries (Fischer et al., 2007; EMCDDA, 2009a, Table HSR-1). Despite positive findings fromrandomised controlled trials in several countries (indicating that diacetylmorphine is effective,safe, and cost-effective, and can reduce drug-related crime and improve patient health), onlyDenmark, Germany, the Netherlands, Switzerland and the United Kingdom include thisintervention as part of the national response to drugs. Pilot programmes are currentlyunderway in Belgium and Luxembourg (EMCDDA, 2009a, Table HSR-1).Access to opioid substitution treatment in European prisonsEuropean countries make up a large proportion of those worldwide that offer OST to prisoners;23 countries in Europe out of 33 globally (Table 2.1). However, there are ‘heterogeneous andinconsistent regulations and treatment modalities throughout Europe’, and practice varies withincountries and from prison to prison (Stöver et al., 2006). OST is available in the majority ofprisons in Austria, Belgium, Croatia, Denmark, Luxembourg, Malta, Portugal, Slovenia andSpain (EMCDDA, 2009a, Figure HSR-2). It remains limited to specific geographical areas or asmall proportion of prisons elsewhere in the region. In France, buprenorphine is more widelyavailable in prisons than methadone (as is the case in the community), but this is still restrictedto certain prisons (van der Gouwe et al., 2006). Latest estimates show that the national prisonsystem of Spain provided OST to 19 010 prisoners, the highest number reported in Europe. Farfewer prisoners were receiving OST in other countries, including Ireland (1 295), Portugal (707),Belgium (300), Luxembourg (191), Finland (40), Serbia (10) and Montenegro (5) (Cook andKanaef, 2008). Switzerland is the only country globally providing heroin (diacetylmorphine)maintenance to prisoners, although this is limited to two facilities (Stöver et al., 2008b).49
Harm reduction: evidence, impacts and challenges
The availability and provision of OST in European prisons has increased in recent years, but theregulations and practices surrounding prison OST vary greatly, leading to gaps betweentreatment need and provision. For example, prison OST is often subject to overly strict inclusioncriteria, resulting in relatively few prisoners being able to access it (BISDRO and WIAD, 2008).Medical risks associated with disruption of long-term maintenance treatment when servingprison sentences remain an issue where OST is not available to prisoners (BISDRO and WIAD,2008). The difference compared to the availability of OST in the community is particularlystriking (EMCDDA, 2009a, Figure HSR-2). Four decades after the introduction of communityOST in Europe and following the considerable scale-up in the past two decades, the gapbetween treatment provision inside and outside prison walls has further increased.
ConclusionKey messages• arm reduction became widely established as a response to HIV/AIDS in the 1980s.H• arly policy and practice was pioneered by a number of European cities.E• y 2009, some 31 countries in Europe had needle and syringe programmes, and 31 had Bopioid substitution treatment.• f the European countries reporting injecting drug use, only Iceland and Turkey have not Oimplemented harm reduction measures.• urope had a significant impact on the diffusion of harm reduction globally, and in 2009 Ethere were 84 countries around the world that endorsed harm reduction in policy orpractice.• he European Union has played a crucial role in promoting and supporting harm reduction Tat the United Nations.
Since the mid-1980s, harm reduction has transformed from a peer-driven, grass-rootsapproach to an official policy of the United Nations, with Europe playing a leading role.European countries were among the ‘earlier adopters’ of harm reduction, facilitating itsdiffusion throughout Europe and beyond. Countries in Europe remain among the forerunnersof innovations in harm reduction practice and technology — for example, developing newNSP products (such as coloured syringes to reduce sharing; Exchange Supplies, n.d.) andinterventions to encourage transitions away from injecting (Pizzey and Hunt, 2008), deliveringNSP and OST in prisons, and establishing DCRs. At the same time, definitions of harmreduction are expanding to embrace the need to protect the rights to health and access toservices of people who use drugs, and to protect them from harmful drug policies, and Europeremains central to this dialogue and advocacy. There are now two decades of research andevaluation exploring the feasibility and impact of harm reduction interventions, especiallyamong people who inject drugs (Kimber et al., 2010; Palmateer et al., 2010; Wiessing et al.,2009; Wodak and Cooney, 2005; Farrell et al., 2005; Institute of Medicine, 2007).Yet harm reduction practice and policy varies across Europe (see also MacGregor andWhiting, 2010). Where national harm reduction responses are well established, these may50
Chapter 2: The diffusion of harm reduction in Europe and beyond
be threatened by governmental changes. The global politics of drug use continue to bepolarised. One recent instance of this was the non-inclusion of the term ‘harm reduction’ inthe ‘Political Declaration’ of the 2009 Commission on Narcotic Drugs, prompting a coalitionof twenty-five UN Member States (the majority being EU countries) to announce that theywould interpret sections of the Declaration to nonetheless mean harm reduction (InternationalDrug Policy Consortium, 2009). The need for networking, exchange and coordination withinEurope remains if policies of harm reduction in Europe and beyond are to be defended,strengthened and properly evaluated.
AcknowledgementsThe authors would like to thank Dagmar Hedrich and Lucas Wiessing from EMCDDA fortheir feedback and comments. In addition, we would also like to thank Cinzia Bentari,Esther Croes, Pat O’Hare, Tuukka Tammi, Daan van der Gouwe, Annette Verster and AlexWodak.
ReferencesAceijas, C., Stimson, G. V., Hickman, M. and Rhodes, T., United Nations Reference Group on HIV/AIDSPrevention and Care among IDU in Developing and Transitional Countries (2004), ‘Global overview of injectingdrug use and HIV infection among injecting drug users’,AIDS18 (17), Nov. 19, pp. 2295–303.Aceijas, C., Hickman, M., Donoghoe, M. C., Burrows, D. and Stuikyte, R. (2007), ‘Access and coverage ofneedle and syringe programmes (NSP) in Central and Eastern Europe and Central Asia’,Addiction102 (8), pp.1244–50.ASUD (French National Association for the Safety of Drug Users) (2008), ‘Global state of harm reductionqualitative data response’, in Cook, C. and Kanaef, N.,Global state of harm reduction: mapping the response todrug-related HIV and hepatitis C epidemics,International Harm Reduction Association, London.Bergeron, H., and Kopp, P. (2002), ‘Policy paradigms, ideas, and interests: the case of the French publichealth policy toward drug abuse’,The Annals of the American Academy of Political and Social Science582 (1),pp. 37–48.Bueno, R. (2007), ‘The Latin American harm reduction network (RELARD): successes and challenges’,InternationalJournal of Drug Policy18, pp. 145–7.Buning, E. C., Van Brussel, G. H. and Van Santen, G. (1990), ‘The “methadone by bus” project in Amsterdam’,British Journal of Addiction85, pp. 1247–50.Canadian AIDS Society (2000),Position statement: harm reduction and substance use.Available at www.cdnaids.ca/web/setup.nsf/(ActiveFiles)/PS_Harm_Reduction_and_Substance_Use/$file/Harm_Reduction_and_Substance_Use_En_Red.pdf.Cook, C. (2009),Harm reduction policies and practices worldwide: an overview of national support for harmreduction in policy and practice,International Harm Reduction Association, London.Cook, C. and Kanaef, N. (2008),Global state of harm reduction: mapping the response to drug-related HIV andhepatitis C epidemics,International Harm Reduction Association, London.
51
Harm reduction: evidence, impacts and challenges
Council of the European Union (2003), ‘Council Recommendation of 18 June 2003 on the prevention andreduction of health-related harm associated with drug dependence’,Official Journal of the European Union3 Jul,L165 (46). Available at http://eur-lex.europa.eu/JOHtml.do?uri=OJ:L:2003:165:SOM:EN:HTML.Csete, J. and Wolfe, D. (2007),Closed to reason: the International Narcotics Control Board and HIV/AIDS,Canadian HIV/AIDS Legal Network and the International Harm Reduction Development Program of the OpenSociety Institute, Toronto/New York, p. 3.Department Committee on Morphine and Heroin Addiction (1926)Report.Available at www.drugtext.org/index.php/en/reports/220.Donoghoe, M., Verster, A., Pervilhac, C. and Williams, P. (2008), ‘Setting targets for universal access to HIVprevention, treatment and care for injecting drug users (IDUs): towards consensus and improved guidance’,International Journal of Drug Policy19 (Supplement 1), pp. S5–S14.EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2000),Reviewing current practice insubstitution treatment,Office for Official Publications of the European Communities, Luxembourg.EMCDDA (2006), Table NSP-1: Number of syringe provision outlets and number of syringes (in thousands)exchanged, distributed or sold 2003, Statistical bulletin 2006. Available at http://stats06.emcdda.europa.eu/en/elements/nsptab02-en.html.EMCDDA (2008),National drug related research in Europe,Selected issue, EMCDDA, Lisbon.EMCDDA (2009a), Statistical bulletin 2009, Available at http://www.emcdda.europa.eu/stats09. Tables HSR‘Health and social responses’. Available at http://www.emcdda.europa.eu/stats09/hsr. Tables PDU ‘Problematicdrug use population’. Available at http://www.emcdda.europa.eu/stats09/pdu.EMCDDA (2009b),Annual report 2009: the state of the drugs problem in Europe,EMCDDA, Lisbon.EMCDDA (2009c), Drug treatment overviews. Available at www.emcdda.europa.eu/responses/treatment-overviews.EMCDDA (2010),Trends in injecting drug use in Europe,Selected issue, European Monitoring Centre for Drugsand Drug Addiction, Lisbon.European Commission (2007), ‘Report from the Commission to the European Parliament and the Council on theimplementation of the Council Recommendation of 18 June 2003 on the prevention and reduction of health-related harm associated with drug dependence’, COM (2007) 199 final (eur-lex.europa.eu/LexUriServ/site/en/com/2007/com2007_0199en01.pdf).European Union (2000a),European Union Drug Strategy 2000–2004.Available at http://www.emcdda.europa.eu/html.cfm/index2005EN.html.European Union (2000b),The European Union Action Plan on Drugs 2000–2004.Available at http://www.emcdda.europa.eu/html.cfm/index1338EN.html.European Union (2004),European Union Drugs Strategy 2005–2012.Available at http://www.emcdda.europa.eu/html.cfm/index6790EN.html.Exchange Supplies (n.d.),Nevershare syringe.Available at http://www.exchangesupplies.org/needle_exchange_supplies/never_share_syringe/never_share_syringe_intro.html.Farrell, M., Gowing, L., Marsden, J., Ling, W. and Ali, R. (2005), ‘Effectiveness of drug dependence treatment inHIV prevention’,International Journal of Drug Policy16 (Supplement 1), pp. S67–S75.
52
Chapter 2: The diffusion of harm reduction in Europe and beyond
Fischer, B., Oviedo-Joekes, E., Blanken, P., et al.. (2007), ‘Heroin-assisted treatment (HAT) a decade later: a briefupdate on science and politics’,Journal of Urban Health84, 552–62.Greenwald, G. (2009),Drug decriminalization in Portugal: lessons for creating fair and successful drug policies,Cato Institute, USA.Hartnoll, R. and Hedrich, D. (1996), ‘AIDS prevention and drug policy: dilemmas in the local environment’, inRhodes, T. and Hartnoll, R. (eds)AIDS, drugs and prevention: perspectives on individual and community action,Routledge, London, pp. 42–65.Hartnoll, R., Avico, U., Ingold, F. R., et al. (1989), ‘A multi-city study of drug misuse in Europe’,Bulletin onNarcotics41, pp. 3–27.Hedrich, D., Pirona, A. and Wiessing, L. (2008), ‘From margins to mainstream: the evolution of harm reductionresponses to problem drug use in Europe’,Drugs: education, prevention and policy15, pp. 503–17.Hedrich, D., Kerr, T. and Dubois-Arber, F. (2010), ‘Drug consumption facilities in Europe and beyond’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Heimer, R. (2008), ‘Community coverage and HIV prevention: assessing metrics for estimating HIV incidencethrough syringe exchange’,International Journal of Drug Policy19 (Supplement 1), pp. S65–S73.Huber, C. (1995), ‘Needle park: what can we learn from the Zürich experience?’Addiction90, pp. 291–2.Hunt, P. (2008),Human rights, health and harm reduction: states’ amnesia and parallel universes: an address byProfessor Paul Hunt, UN Special Rapporteur on the right to the highest attainable standard of health,Harm Reduction2008: IHRA’s 19th International Conference, Barcelona — 11 May 2008, International Harm ReductionAssociation, London.IHRA (International Harm Reduction Association) (2009a),What is harm reduction? A position statement from theInternational Harm Reduction Association,International Harm Reduction Association, London.IHRA (2009b),Building consensus: a reference guide to human rights and drug policy,International Harm ReductionAssociation, London.IHRA (2009c),German parliament votes in favour of heroin assisted treatment.Available at www.ihra.net/June2009#GermanParliamentVotesinFavourofHeroinAssistedTreatment.IHRA and Human Rights Watch (2009),Building consensus: a reference guide to human rights and drug policy,International Harm Reduction Association, London, pp. 18–19.Institute of Medicine (2007),Preventing HIV infection among injecting drug users in high risk countries: an assessmentof the evidence,Committee on the Prevention of HIV Infection Among Injecting Drug Users in High-Risk Countries,National Academies Press, Washington.International Drug Policy Consortium (2009), ‘The 2009 Commission on Narcotic Drugs and its high levelsegment: report of proceedings’,IDPC Briefing Paper,April.Kazatchkine, M. and McClure, C. (2009),From evidence to action: reflections on the global politics of harmreduction and HIV,International Harm Reduction Association, London.Kimber, J., Palmateer, N., Hutchinson, S., et al. (2010), ‘Harm reduction among injecting drug users: evidence ofeffectiveness’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction:
53
Harm reduction: evidence, impacts and challenges
evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10,Publications Office of the European Union, Luxembourg.Lane, S. D. (1993),Needle exchange: a brief history.Available at www.aegis.com/law/journals/1993/HKFNE009.html.MacGregor, S. and Whiting, M. (2010), ‘The development of European drug policy and the place of harmreduction within this’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction:evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10,Publications Office of the European Union, Luxembourg.Michels, I. I., Stöver, H. and Gerlach, R. (2007), ‘Substitution treatment for opiate addicts in Germany’,HarmReduction Journal4 (5). Available at http://www.harmreductionjournal.com/content/4/1/5.Moss, A. (1990), ‘Control of HIV infection in injecting drug users in San Francisco’, in Strang, J. and Stimson, G.V.,AIDS and drug misuse: the challenge for policy and practice in the 1990s,Routledge, London.Needle, R. H., Burrows, D., Friedman, S. R., et al. (2005), ‘Effectiveness of community-based outreach inpreventing HIV/AIDS among injecting drug users’,International Journal of Drug Policy16 (Supplement 1), pp.45–57.O’Hare, P. (2007a), ‘Harm reduction in the Mersey region’,International Journal of Drug Policy18, p. 152.O’Hare, P. (2007b), ‘Merseyside: the first harm reduction conferences and the early history of harm reduction’,International Journal of Drug Policy18, pp. 141–4.Olsson, B., Adamsson Wahren, C. and Byqvist, S. (2001),Det tunga narkotikamissbrukets omfattning I Sverige1998,CAN, Stockholm.Palmateer, N., Kimber, J., Hickman, M., et al. (2010), ‘Preventing hepatitis C and HIV transmission amonginjecting drug users: a review of reviews’,Addiction,in press.Pizzey, R. and Hunt, N. (2008), ‘Distributing foil from needle and syringe programmes (NSPs) to promotetransitions from heroin injecting to chasing: an evaluation’,Harm Reduction Journal5, p. 24.Rhodes, T. (1993), ‘Time for community change: what has outreach to offer?’,Addiction88, pp. 1317–20.Rhodes, T. and Hartnoll, R. (1991), ‘Reaching the hard to reach: models of HIV outreach health education’, inAggleton, P., Davies, P. and Hart, G. (eds),AIDS: responses, interventions and care,Falmer Press, London.Robertson, J. R., Bucknall, A. B. V., Welsby, P. D., et al. (1986), ‘Epidemic of AIDS-related virus (HTLV-III/LAV)infection among intravenous drug abusers’,British Medical Journal292, p. 527.Sharma, M., Burrows, D. and Bluthenthal, R. (2008), ‘Improving coverage and scale-up of HIV prevention,treatment and care for injecting drug users: moving the agenda forward’,International Journal of Drug Policy19(Supplement 1), pp. 1–4.Sherman, S. G. and Purchase, D. (2001) ‘Point defiance: a case study of the United States’ first public needleexchange in Tacoma, Washington’,International Journal of Drug Policy12, pp. 45–57.Stimson, G. V. (1989), ‘Syringe exchange programmes for injecting drug users’,AIDS3, pp. 253–60.Stimson, G. V. (1990a), ‘AIDS and HIV: the challenge for British drug services’,British Journal of Addiction85 (3),pp. 329–39.Stimson, G. V. (1990b), ‘Revising policy and practice: new ideas about the drugs problem’, in Strang, J. andStimson, G.,AIDS and drug misuse: the challenge for policy and practice in the 1990s,London, Routledge.
54
Chapter 2: The diffusion of harm reduction in Europe and beyond
Stimson, G. V. (1991), ‘Risk reduction by drug users with regard to HIV infection’,International Review of Psychiatry3, pp. 401–15.Stimson, G. V. (1994), ‘Reconstruction of sub-regional diffusion of HIV infection among injecting drug users inSouth East Asia: implications for early intervention’,AIDS8, pp. 1630–2.Stimson, G. V. (1995), ‘AIDS and injecting drug use in the United Kingdom, 1987–1993: the policy response andthe prevention of the epidemic’,Social Science and Medicine41 (5), pp. 699–716.Stimson, G. V. (2007), ‘Harm reduction — coming of age: a local movement with global impact’,InternationalJournal of Drug Policy18, pp. 67–9.Stimson, G. V. and Lart, R. (1990), ‘HIV, drugs and public health in England: new words, old tunes’,InternationalJournal of the Addictions26, pp. 1263–77.Stimson, G. V. and Oppenheimer, E. (1982),Heroin addiction: treatment and control in Britain,Tavistock, London.Stöver, H., Casselman, J. and Hennebel, L. (2006), ‘Substitution treatment in European prisons: a study of policiesand practices in 18 European countries’,International Journal of Prisoner HealthMarch, 2 (1), pp. 3–12.Stöver, H., Weilandt, C., Zurhold, H., Hartwig, C. and Thane, K. (2008a),Final report on prevention, treatment,and harm reduction services in prison, on reintegration services on release from prison and methods to monitor/analyse drug use among prisoners,European Commission Directorate — General for Health and Consumers, DrugPolicy and Harm Reduction, SANCO/2006/C4/02.Stöver, H., Weilandt, C., Huisman, A., et al. (2008b),Reduction of drug-related crime in prison: the impact ofopioid substitution treatment on the manageability of opioid dependent prisoners,BISDRO, University of Bremen,Bremen.Svenska Brukarföreningen/Swedish Drug Users Union and International Harm Reduction Association (2007),Briefing to the Committee on Economic, Social and Cultural Rights on the fifth report of Sweden on the implementationof the International Covenant on Economic, Social and Cultural Rights,International Harm Reduction Association,London.Touze, G., Rossi, D., Goltzman, P., et al. (1999), ‘Harm reduction in Argentina: a challenge to non-governmentalorganisations’,International Journal of Drug Policy10, pp. 47–51.van der Gouwe, D., Gallà, M., van Gageldonk, A., et al. (2006),Prevention and reduction of health-related harmassociated with drug dependence: an inventory of policies, evidence and practices in the EU relevant to theimplementation of the Council Recommendation of 18 June 2003,Trimbos Instituut, Utrecht.UNAIDS (Joint United Nations Programme on HIV/AIDS) (2005a),Intensifying HIV prevention: UNAIDS PolicyPosition Paper,UNAIDS, Geneva. Available at http://data.unaids.org/publications/irc-pub06/jc1165-intensif_hiv-newstyle_en.pdf.UNAIDS (2005b),UNAIDS Technical Support Division of Labour: summary & rationale,UNAIDS, Geneva.Available at data.unaids.org/una-docs/JC1146-Division_of_labour.pdfUnited Kingdom National Treatment Agency (2007),Global state — data collection response.Cited in Cook, C.and Kanaef, N. (2008),Global state of harm reduction 2008: mapping the response to drug-related HIV andhepatitis C epidemics,International Harm Reduction Association, London.United Nations Commission on Narcotic Drugs (2009),Report on the fifty-second session (14 March 2008 and11–20 March 2009) Economic and Social Council Official Records, 2009: supplement no. 8 — political declarationand plan of action on international cooperation towards an integrated and balanced strategy to counter the worlddrug problem,United Nations Commission on Narcotic Drugs,Vienna.
55
Harm reduction: evidence, impacts and challenges
United Nations General Assembly Sixtieth Special Session (2006), ‘Agenda item 45: resolution adopted by theGeneral Assembly. 60/262’,Political declaration on HIV/AIDS,New York.United Nations General Assembly Twenty-Sixth Special Session (2001), ‘Agenda item 8: resolution adopted bythe General Assembly. S-26/2’,Declaration of Commitment on HIV/AIDS,New York.Vickerman, P., Hickman, M., Rhodes, T. and Watts, C. (2006), ‘Model projections on the required coverage ofsyringe distribution to prevent HIV epidemics among injecting drug users’,Journal of Acquired Immune DeficiencySyndromes42, pp. 355–61.Watters, J. (1996), ‘Americans and syringe exchange: roots of resistance’, in Rhodes, T. and Hartnoll, R. (eds),AIDS, drugs and prevention: perspectives on individual and community action,Routledge, London, pp. 22–41.Wellbourne-Wood, D. (1999), ‘Harm reduction in Australia: some problems putting policy into practice’,International Journal of Drug Policy10, pp. 403–13.Wiessing, L., van de Laar, M. J., Donoghoe, M. C., et al. (2008), ‘HIV among injecting drug users in Europe:increasing trends in the east’,Eurosurveillance13 (50). Available at http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19067.Wiessing, L., Likatavičius, G., Klempová, D., et al. (2009), ‘Associations between availability and coverage ofHIV-prevention measures and subsequent incidence of diagnosed HIV infection among injection drug users’,American Journal of Public Health99 (6), pp.1049–52.Wodak, A. (2004), ‘Letter from Dr Alex Wodak to Dr Zerhouni at the US National Institute of Health NIH’.Available at www.drugpolicy.org/library/05_07_04wodaknih.cfm.Wodak, A. and Cooney, A. (2005), ‘Effectiveness of sterile needle and syringe programmes’,InternationalJournal of Drug Policy16, S1, pp. S31–S44.WHO (World Health Organization) (1986),Consultation on AIDS among drug abusers,7–9 October 1986,Stockholm, ICP/ADA535(S).WHO (2005a),Evidence for action series.Available at www.who.int/hiv/pub/idu/idupolicybriefs/en/index.htmland http://whqlibdoc.who.int/publications/2007/9789241595780_eng.pdf.WHO (2005b),Essential medicines: WHO model list(14th edition). Available at http://whqlibdoc.who.int/hq/2005/a87017_eng.pdf.WHO (2005c),Status paper on prisons, drugs and harm reduction,World Health Organization, Copenhagen.Available at http://www.euro.who.int/document/e85877.pdf.WHO (2009),HIV/AIDS: comprehensive harm reduction package.Available at http://www.who.int/hiv/topics/idu/harm_reduction/en/index.html.WHO, UNODC (United Nations Office on Drugs and Crime) and UNAIDS (2009),Technical guide for countries toset targets for universal access to HIV prevention, treatment and care for injecting drug users,WHO, UNODC/UNAIDS.
56
Chapter 3The development of European drug policy and the place ofharm reduction within thisSusanne MacGregor and Marcus Whiting
AbstractThis chapter gives a necessarily brief overview of the development of drug policy at theEuropean Union level in recent decades. These developments are set within the wider contextof moves towards European integration. The chapter considers how far a process ofconvergence has occurred, within which harm reduction may have a central place; and howfar this gives a distinctive character to European policy internationally. It draws mainly ondocumentary evidence and scholarly accounts of policy development. Key processesidentified include: the achievement of agreed policy statements at intergovernmental level; theinfluence of guidance, action plans and target setting; the role of the European MonitoringCentre for Drugs and Drug Addiction (EMCDDA); the spread of information; networking,training and collaborative activities among researchers and practitioners; the size and shapeof the drug problem; and the impact of HIV/AIDS. While common agreements have beenforged at the supra-national level, differences remain between and within different MemberStates, reflecting their social and political institutions, differing public attitudes, religious andcultural values, and varying financial and human resources.Keywords:European drug policy, harm reduction, convergence, cultural and institutionaldifferences, political influences.
IntroductionA steady, progressive evolution of drugs policy, towards a more rational, evidence-basedapproach, has been the ambition of medical humanists and technocrats involved in policy andpractice networks in the EU. Advocates like the International Harm Reduction Association andthe Open Society Institute also hope to see harm reduction principles entrenched within policy. Inthe light of this, the aim of this chapter is to explore how policies have developed over time andwhat forces have been influential, considering in particular what has been achieved in terms ofpolicy convergence and the introduction of harm reduction. To do this, we draw largely upon ananalysis of the content of EU policy documents and key published books and articles.We define ‘Europe’ here as primarily referring to the European Union, and ‘drug policy’ asstatements in EU policy documents. However, we recognise that Europe is a largergeographical and cultural entity than the European Union itself, and that the national policiesof European countries also form part of ‘European drug policy’. In addition, we are awarethat policies cannot be judged solely on the basis of statements in documents or the rhetoricof politicians and other players on the policy field. ‘Policy’ more broadly defined refers to the59
Harm reduction: evidence, impacts and challenges
way a society meets needs, maintains control and manages risks. To describe and assess thiswould require analysis of what actually happens and with what impacts. Policy judged byfunctions or effects may result from forces other than the overt goals in formal policystatements. In a short chapter such as this, it is not possible to analyse or account for all theseforces. We have chosen instead to look mainly at the formal development of EU drug policy,but attempt to set this within its context and to indicate that the process of development hasnot been inevitable and has at times been contentious.
MethodsThis paper draws on research towards a social history of the development of the drugsproblem and responses to it over a 30-year period. Here the focus is on European drugpolicy and specifically its links to public health and discussions of the role of harm reductionapproaches. Methods used have included reviews of secondary literature in books andjournals and of documentary evidence, especially that available through Europeaninstitutions like the European Commission and the EMCDDA. Observation of discussions atconferences and networking meetings has also played a part, along with interviews withsome of the key players in the development of policy over this period. A detailed narrativehistory is not possible in a short chapter so the approach adopted here is to present aninterpretative account of developments.
The context for policy developmentDevelopment of the European UnionThe European Union (EU) is a political and economic union in which sovereign countries agreeto share or give up some attributions and powers. A simple description of the process of policydevelopment would note that in any given field it starts with open intergovernmental discussionsthen moves into areas where the union’s institutions obtain some power of proposition, action ordecision. The EU is thus a policy actor in itself and one that is progressively trying to createconvergence, while limited in its influence on actions at national level.The EU has expanded rapidly to its current 27 Member States in a period of economicliberalisation involving free movement of both labour and capital and a reduction in bordercontrols. The size and shape of the drugs problem and responses to it within Europe have beeninfluenced by these larger trends and the series of treaties that marked this trajectory: the SingleEuropean Act 1986; Maastricht Treaty 1993; Amsterdam Treaty 1997; and the most recentLisbon Treaty. These Acts were important contextual features and, together with the collapse ofthe Soviet Union and reductions in border controls, influenced the supply of illicit drugs and theresponses of criminal justice agencies. A number of key principles are important features of theEuropean Project, especially human rights, electoral democracy and free trade.Throughout this period there have been two different visions of the European Union —characterised as the ‘widening’ or ‘deepening’ scenarios — with enlargement paralleling thedominance of the widening, free market approach. This approach emphasises economic60
Chapter 3: The development of European drug policy and the place of harm reduction within this
cooperation alongside the retention of national sovereignty and national differences withregard to social and political institutions. The deepening agenda would hope to seeagreement on social policies.While drug policy does not fit neatly into conventional models of social policy, attitudes to drugsand social responses to problems do reflect the historical development of institutions (constrainingand shaping options for policy change) and cultural norms relating to rights and responsibilities.Moves towards a shared EU approach to drugs have been in this sense part of the EuropeanProject. The development of a drug policy could indicate some success for moves to deepenintegration, with the development of shared practices related to social and criminal justicepolicies. The widening agenda — with enlargement increasing the number of EU Member States— clearly presents problems for integrationist ambitions as it increases the range of difference tobe potentially coordinated in any shared strategy — differences of culture, language, pathdependency in the development of institutions, human and financial resources: these and moreinfluence the potential for acceptance and implementation of policy proposals.National policiesWe begin with a brief overview of the current state of play, considering what has beenachieved in terms of policy coordination and recognition of a role for harm reduction. In2008, there were 14 national strategies, 15 action plans, six programmes, two policy notes/documents, one white paper, one governmental plan, one implementation decree, andnumerous provincial, regional, local or devolved administration documents relating to drugpolicy within the countries of the EU. A general trend can be discerned towards theproduction of explicit strategies and related action plans, increasingly linked to an overall EUdrugs strategy. Within these statements, the term ‘harm reduction’ is often present and insome countries is specifically identified as a major policy goal (see Table 3.1).
Table 3.1:Overview of national drug strategies and references to harm reductionwithin themCountryBelgium
PolicyDrug policy note 2001; covers bothlicit and illicit drugsNational anti-drug strategy2003–08 plus action planNational Drug Policy Strategy2005–09 plus action plan
References to harm reductionHarm reduction (plus assistance andreintegration) one of three pillars ofpolicyProgramme for the development ofmethadone maintenance adopted2006Harm reduction one of seven policyfields in action plan
Bulgaria
Czech RepublicDenmark
Action plan ‘The fight against drugs’ Harm reduction as a goal2003‘paradoxical’ but should be anintegrated element — some of theseinitiatives may be ‘pragmatic andreasonable’
61
Harm reduction: evidence, impacts and challenges
Table 3.1(continued)CountryGermany
PolicyAction plan on drugs and drugaddiction 2003 — focus on allpsychotropic substancesNational strategy on the preventionof drug dependency 2005 plustriennial action plansNational drug strategy 2001
References to harm reductionHarm reduction (with survival aid)one of four pillars of policyHarm reduction one of six pillars ofpolicyNeed for continued efforts toenhance harm reduction measures,such as needle and syringeprogrammes (NSPs)
Estonia
Ireland
GreeceSpain
National strategy on drugs 2006— focus on illicit drugs and alcoholNational drug strategy 1999 plusaction plan 2005Harm reduction a specific section inthe strategy, with objective to ensureaccess to harm reductionprogrammes for drug dependentpeople with targets, especially NSPsand vaccinationsHarm reduction (with socialreintegration) one of five axes of theplanHarm reduction objectives listed,including NSPs and opioidsubstitution treatment (OST)
France
Governmental plan to fight drugsand drug addiction 2008; coversboth alcohol and illicit drugsNew action plan 2008National drug strategy 2004 plustwo action plans — focus on licitand illicit substancesState programme for the reductionof addiction to narcotic andpsychotropic substances 2005–08National strategy on drug addictionprevention and control, and relatednational programme forimplementationNational strategy and action planon drugs and drug addiction2005–09
ItalyCyprus
Latvia
Lithuania
Luxembourg
Treatment is preferred to harmreduction, but integrated andcomplementary approach required;reduction of risks, harms andnuisance one of four axes of policySpecific section on harm reduction,with reference to outreach, OSTand NSPs as priority goals incontext of development oftreatment services
Hungary
National strategy on drugs2000–09, plus action plan 2007
Malta
Drugs policy document adopted2008
62
Chapter 3: The development of European drug policy and the place of harm reduction within this
Table 3.1(continued)CountryNetherlands
PolicyWhite Paper 1995 Drugs Policy:continuity and change —distinguishes soft and hard drugsNo federal strategy or action plan— objectives devolved by the nineprovincesNational programme forcounteracting drug addiction 2006
References to harm reductionTo reduce harm to users, one of fourmajor objectives of policy
Austria
Poland
Harm reduction (with treatment,rehabilitation and socialreintegration) one of five pillars ofpolicySpecific sections on risk and harmreduction. Aim to constantlyimprove risk and harm reductioninterventions. The boundariesbetween prevention, treatment, riskand harm reduction, reintegrationand dissuasion are ‘artificial’Specific section on harm reductionin action planSpecific discussion of harmreduction programmes but in thecontext of noting that there are toofew — aim to set up network ofharm reduction programmes andincrease access
Portugal
National strategy for the fightagainst drugs 1999, plus strategicplan for implementation
RomaniaSlovenia
Anti-drug strategy 2005 plus actionplanResolution on the nationalprogramme on drugs 2004
Slovakia
National programme for the fightagainst drugs 2005 plus actionplans1997 national drug strategy and2007 resolutionSeparate plans for alcohol anddrugs but adopted together:national alcohol and drug actionplans 2006Drugs: protecting families andcommunities 2008 — ten-yearstrategy plus three-year action planReference to harm minimisationthrough NSE and relevant treatmentsHarm reduction (together withtreatment) one of seven policyareas
Finland
Sweden
United Kingdom
Note: The full text versions of the national drug strategies are available at http://www.emcdda.europa.eu/policy-and-law/national/strategies.
At the present time, EMCDDA states, ‘the prevention and reduction of drug-related harm isa public health objective in all Member States and in the EU drug strategy and actionplan ... The general European trend is one of growth and consolidation of harm reduction63
Harm reduction: evidence, impacts and challenges
measures’ (EMCDDA, 2009, p. 31). But a closer look at the current situation gives a morequalified picture. EU Member States do employ a combination of some of the main harmreduction measures, which ‘are reported to be available in all countries except Turkey [but]considerable differences exist in the range and levels of service provision’ (EMCDDA,2009, p. 31).Thus, harm reduction occupies a clear place within European policies but its influence shouldnot be overstated. However, while differences between countries remain, these are not asgreat as in earlier times. The move to a shared position has involved compromises and a shiftto the centre. Shared features of policy are also evident in the stress on research andinformation exchange and use of managerialist approaches, involving action plans,logframes, strategies, targets and benchmarks.How, then, do we explain continuing differences at national level? Do drug policies follow theshape of the drug problem in a country, and is this in itself a reflection of attitudes to druguse? Or can the policy environment influence attitudes and thus the size and nature of drugtaking and associated problems?Since 1998, the year of the UNGASS Twentieth Session Declarations (United Nations, 1998),‘most European countries have moved towards an approach that distinguishes between thedrug trafficker, who is viewed as a criminal, and the drug user, who is seen more as a sickperson in need of treatment’ (EMCDDA, 2008, p. 22). Differences remain, however, forexample on whether or not to set threshold quantities for personal possession. There aredifferences also regarding maximum or probable sentences and whether or not these arebecoming more punitive or lenient. Encouragement into treatment (increasingly as analternative to a criminal charge or sentence) is developing across countries, but differencesremain with regard to the stage when referral to treatment occurs. In the majority of MemberStates, substitution treatment combined with psychosocial care is the predominant option foropioid users. Shared concerns about public nuisance are visible, as are concerns arounddriving under the influence or use in the workplace.In general, public attitudes to drug taking appear to remain primarily restrictive. Forexample, a Eurobarometer survey in 2006 conducted in 29 countries found only 26 %supporting legalisation of the possession of cannabis for personal use (ranging from 8 % inFinland to 49 % in the Netherlands) (Eurobarometer, 2006, pp. 36, 49–50). A review ofattitudes to drug policy in three countries with relatively restrictive policies (Bulgaria, Polandand Sweden) and three countries with relatively liberal ones (Czech Republic, theNetherlands and Denmark) found that for most people the most important factor influencingthem not to use illicit drugs was concern about health consequences (ranging from 73 % inBulgaria to 27 % in Holland). Fewer were primarily influenced by the fact of illegality(ranging from 3 % in Denmark to 19 % in Poland). Most saw prevention and education as themost important policy area (ranging from 17 % in Poland to 57 % in Sweden). Needle andsyringe programmes (NSPs) were supported by some respondents (ranging between 22 % inSweden and 54 % in Denmark) but opposed by others (ranging from 7 % in Denmark to29 % in Bulgaria).64
Chapter 3: The development of European drug policy and the place of harm reduction within this
This survey found a correlation between public attitudes on drug use and a country’s drugpolicies (Hungarian Civil Liberties Union, 2009). Countries were deeply divided in their viewson the decriminalisation of cannabis. The majority considered drug use to be a public healthissue and there was wide acceptance of NSPs as a response to HIV. However, the majoritybelieved that prescribing heroin for addicts would do more harm than good. It is worthnoting that some of the countries described above as relatively liberal have seen legislativeand administrative moves to more repressive responses in recent years. So there is movementin a number of directions, away from harm reduction and public health principles in somecases, while in others there is a move towards agreement around a core of the moremoderate and less contentious issues.
European Union drug policyEU Member States are the main actors in the drug field, and drug legislation is a matter ofnational competence. However, the Treaties explicitly acknowledge the need to deal withdrug issues at EU level, in particular in the fields of justice and home affairs, and publichealth. The tension between ideas of law enforcement and ideas of public health is built intothis policy area. Drug trafficking has been a key area for developing cooperation betweenpolice and judiciaries. A multidisciplinary group has been working on organised crime andincreased cooperation has developed between police, customs and Europol groups. Themain technical and policy forum to facilitate joint efforts of Member States and theCommission is the EU Council’s Horizontal Drugs Group (HDG). This meets about once amonth, bringing together representatives of Member States and the Commission. The HDG isplaying a key role in the drafting of European drug policy documents. One of them is thecurrent EU drugs strategy (2005–12) endorsed by the Council of the European Union inDecember 2004, which sets out two general aims:1. The EU aims at a contribution to the attainment of a high level of health protection, wellbeing and social cohesion by complementing Member States’ action in preventing andreducing drug use, dependence and drug related harms to health and society; and2. the EU and its Member States aim to ensure a high level of security for the general publicby taking action against drug production, cross border trafficking in drugs and diversionof precursors and by intensifying preventive action against drug related crime througheffective cooperation embedded in a joint approach.(European Commission, 2008, p. 7)Overall, responsibility for drugs continues to be diffused across all pillars (1), leading to someconfusion, and a constant struggle to improve coordination, which has developed in some(1)Between 1993 and 2009, the European Union (EU) legally comprised three pillars: economic, social andenvironmental policies; foreign policy and military matters; and one concerning cooperation in the fight againstcrime. This structure was introduced with the Treaty of Maastricht in 1993, and was eventually abandoned on 1December 2009 with the entry into force of the Treaty of Lisbon, when the EU obtained a consolidated legalpersonality.
65
Harm reduction: evidence, impacts and challenges
areas more than others. The strategy also stresses the value of consultation with a broadgroup of partners, principally scientific centres, drug professionals, representative non-government organisations (NGOs), civil society and local communities. The current EU drugsaction plan focuses on five priorities: improving coordination, cooperation and raising publicawareness; reducing the demand for drugs; reducing the supply of drugs; improvinginternational cooperation; and improving understanding of the problem.Moves toward harm reductionUnder the heading of demand reduction, objective 10 of the current 2009–12 EU drugsaction plan refers specifically to harm reduction. The objective here is to ‘ensure access toharm reduction services in order to reduce the spread of HIV/AIDS, hepatitis C and otherdrug-related blood borne infectious diseases and to reduce the number of drug-relateddeaths in the EU’ (OJ C 326, 20.12.2008, p. 14).Before that, on 18 June 2003, the Council of the EU had already adopted a recommendationon the prevention and reduction of health-related harm associated with drug dependence.This referred to the following aims:Member States should, in order to provide for a high level of health protection, set as a publichealth objective the prevention of drug dependence and the reduction of related risks, anddevelop and implement comprehensive strategies accordingly … Member States should, in orderto reduce substantially the incidence of drug-related health damage (such as HIV, hepatitis B andC and tuberculosis) and the number of drug related deaths, make available, as an integral partof their overall drug prevention and treatment policies, a range of different services and facilities,particularly aiming at risk reduction.(Council of the European Union, 2003/488/EC)
This recommendation called upon Member States to provide a number of harm reductioninterventions, including: information and counselling; outreach; drug-free and substitutiontreatment; hepatitis B vaccination; prevention interventions for HIV, hepatitis B and C,tuberculosis and sexually transmitted diseases; the distribution of condoms; and thedistribution and exchange of injecting equipment (see also Cook et al., 2010).Drawing upon numerous EU policy documents, Figure 3.1 summarises some key events in thedevelopment of EU drug policy, noting the place of harm reduction within this. It suggests thatuntil the mid-1980s, the idea of a European drug policy had not even been debated. Sincethis time, attention to drug issues has increased, and policy has developed in scope anddetail. In the 1992 Maastricht Treaty, drug dependence was included in the field of publichealth. This was the first example of an EU treaty that specifically mentioned drugs andopened the possibility for setting up EU action and funding programmes in this field,although under the principle of ‘subsidiarity’. Subsidiarity means that in policy areas that donot come within the exclusive competence of the Community, action would be taken at EUlevel only if the objectives of the proposed action could not be sufficiently achieved byMember States acting alone and could be better achieved by the Community.66
Chapter 3: The development of European drug policy and the place of harm reduction within this
Table 3.2Some key events in the development of European drug policyEventCo-operation Group to combat drugabuse and illicit trafficking in drugs(Pompidou Group) set up at Council ofEurope, StrasbourgTrevi working groups to counter terrorismand to coordinate policingSchengen Agreement
Date1971
NotesFirst multidisciplinary cooperation groupin drugs field in Europe
1976
Agreed by EC Interior Ministers
1985
Removed border controls betweenBelgium, the Netherlands, Luxembourg,Germany and FranceTo focus on international drug trafficking
EC countries redefine task of Trevi 3working groupSingle European ActStewart-Clark Inquiry into the DrugsProblem in the Member States of theCommunityUN Convention against the Illicit Traffic inNarcotic Drugs and PsychotropicSubstancesCELAD established (European Committeeto Combat Drugs)First European action plan to combatdrugsFrankfurt Resolution established ECDP(European Cities on Drug Policy)Revision of European plan to combatdrugsFirst European Drug Prevention Week,LondonCooney Inquiry on Drug Trafficking andOrganised CrimeMaastricht TreatyEuropol Drugs Unit agreedEMCDDA agreedECAD (European Cities Against Drugs) setup via Stockholm resolutionEMCDDA established in LisbonEuropean Union action plan to combatdrugs (1996–2000)1993199219881986
Signed by EC Member StatesCommissioned by European Parliament
Adopted at United Nations Conference
19891990
Members are coordinators of nationaldrug policy — existed until 1993Adopted by European Council in Rome(December 1990)At First Conference: European Cities atthe Centre of Illegal Trade in Drugs,FrankfurtAdopted by European Council inEdinburgh (December)Funded by the European CommissionCommissioned by the EuropeanParliamentCELAD became K4 Committee — existeduntil 1997At First Major Conference, in Stockholm
19941995
Adopted at Cannes European Council,June
67
Harm reduction: evidence, impacts and challenges
Table 3.2(continued)EventCommunity Programme for the preventionof drug dependence(1996–2000)Dublin European CouncilEuropol Drugs Unit established in TheHagueAmsterdam TreatyHorizontal Drugs Group set upEC Drug Unit placed under Task Force forJustice and Home AffairsAgreement between EU and Andescountries on money laundering andprecursorsEuropol Drug Unit is replaced by EuropolEU drugs strategy (2000–04)EU action plan on drugs (2000–04)Council of Ministers passesRecommendation on the prevention andreduction of health-related harmassociated with drug dependencePompidou Group platforms forPrevention, Treatment and ResearchestablishedCouncil Framework Decision on drugtraffickingEU drugs strategy (2005–12)EU drugs action plan (2005–08)HIV/AIDS protocols on treatment andcare for the European regionGreen Paper ‘The role of civil society indrugs policy in the European Union’2006200519992000200319981999Later agreements also with Chile andMexico and with West and South Africaand CaribbeanFocus on serious international organisedcrimeEndorsed by European Council in HelsinkiEndorsed at European Council in Sta.Maria da FeiraSeen as major step towards a progressivepublic health approach1997Agreement on draft reached (entered intoforce in 1999)To report back to Coreper — replacedK4 committee
Date1996
NotesFunding programme decided byEuropean Parliament and Council,implemented by European CommissionAgreed need for strategy againstorganised crime
2004
Also stress on dealing with new syntheticdrugs and chemical precursors andmoney launderingEndorsed by European CouncilPublished by WHO/EuropePresented by the European Commission
68
Chapter 3: The development of European drug policy and the place of harm reduction within this
Table 3.2(continued)EventDrug Prevention and InformationProgramme (2007–13)EU drugs action plan (2009–12)
Date2007
NotesFunding programme decided byEuropean Parliament and Council,implemented by European CommissionEndorsed by European Council
2008
The 1997 Treaty of Amsterdam put even more stress on public health and made explicitreference to drugs. It was agreed that ‘the Community shall complement the Member States’actions in reducing drugs-related health damage, including information and prevention’.Specific interventions are now detailed in two action plans (2005–08 and 2009–12) whichinter aliaaim to significantly reduce the prevalence of drug use among the population andthe social harm and health damage caused by the use of and trade in illicit drugs. Actions atEU level must be targeted and offer clear added value, and results must be realistic andmeasurable. Actions must also be cost-effective and contribute directly to the achievement ofat least one of the goals or priorities set out in the EU drug strategy. Evaluation of the impactof the first action plan (2005–08) in the area of demand reduction concluded that: ‘Thereremains a lack of reliable and consistent information to describe the existence of or evaluatethe impact of prevention programmes; that further improvements are still needed inaccessibility, availability and coverage of treatment programmes; and that the majority ofMember States offer drug-free treatment, psychosocial treatment and substitution treatment’(European Commission, 2008, p. 66).The European Commission concluded that:In the field of harm reduction, major progress has been achieved in recent years. In all EUMember States the prevention and reduction of drug related harm is a defined public healthobjective at national level. Among the most prevalent interventions are needle and syringeexchange programmes, outreach workers and opioid substitution treatment combined withpsychosocial assistance. However availability and accessibility of these programmes are variableamong the Member States and in some countries with low coverage, there are signs of higherlevels of risk taking among new, younger generations of — in particular — heroin injectors whohave not been reached by prevention and harm reduction messages.(European Commission, 2008, p. 66 [6.1.2.3: 4])
The continuing lack of provision of services in relation to drug users in prison and releasedprisoners was also noted, while ‘treatment and harm reduction programmes are often nottailored to address the specific needs and problems of different groups of problem ordependent drug users, for example, women, under-aged young people, migrants, specificethnic groups and vulnerable groups’ (European Commission, 2008, p. 66 [6.1.2.3:7]). TheCommission also noted that ‘the evaluation shows that the action plan supports a process ofconvergence between Member States’ drug policies and helps to achieve policy consistencybetween countries’ (European Commission, 2008, p. 67 [6.1.3:2]).69
Harm reduction: evidence, impacts and challenges
Factors influencing the development of EU drugs policyOn the occasion of the launch of the EMCDDA’s Annual report on the state of the drugproblem in Europe in 2008, the Director, Mr Götz, said, ‘there is a stronger agreement onthe direction to follow and a clearer understanding of the challenges ahead’, indicating hisopinion that within Europe a convergence of views on policy is developing. If this is so, it is aremarkable change in just over 20 years.A number of factors appear to have been influential in shaping developments in Europeandrug policy:• he evolution within the European Union of competencies in the field of drugs;t• he rising political priority of drugs across the areas of public health, public security (justice tand home affairs) and external relations;• clear demand from various European institutions as well as Member States for ainformation and evidence for policymaking and decisions;• he creation of institutions such as the Pompidou Group and then EMCDDA and its tnational counterparts to meet those information needs;• he existence alongside the institutional developments of longstanding and interlinked thuman networks of drug researchers and the possibilities to channel that scientificknowledge into the institutional process;• he wider influence of international connections and the exchange of knowledge and texperience.(Hartnoll, 2003, p. 67)Additional factors are: the growing similarities between countries in the nature and extent oftheir drug problems; the influence of evidence-based reason winning over ideology; and theeffects of involvement in the practice of data collection and analysis, and a relateddevelopment of norms, values and institutions (Bergeron and Griffiths, 2006, p. 123). Ingeneral terms, trends in drug use have affected many EU countries in roughly the same wayand at roughly the same time (Bergeron and Griffiths, 2006). These have led to fairly radicalchanges in many countries, especially in the light of HIV/AIDS (see also Cook et al., 2010). Inmost EU countries, HIV and AIDS became a problem in the 1980s, levelling off after the1990s, but with high levels of hepatitis C (EMCDDA, 2008). In addition, ‘since the 1985Schengen agreement, and its facilitation of free movement around Europe, the prevention ofinternational drug trafficking and organised crime has become a priority for all memberstates’ (Chatwin, 2007, p. 496) andnational governments are eager to reap the benefits of unity in the area of controlling organisedcrime and the illegal trafficking of drugs. However, spillover of this level of European control toareas other than drug trafficking and organised crime prevention has not been as extensive.Trends towards the implementation of harm reduction initiatives and the decriminalisation of thedrug user can be observed across Europe, with notable exceptions, but unity of policy in this areadoes not enjoy the same degree of official encouragement(Chatwin, 2007, p. 497)
70
Chapter 3: The development of European drug policy and the place of harm reduction within this
However, Chatwin has concluded that with regard to ‘the fight against organised crime anddrug trafficking, some progress towards a European drug policy is being made’ (Chatwin,2003, pp. 40–1). Finally, the ‘context of a particular country, its size, geographical positionand relation to its neighbours, the state of the drug problem and public opinion … politicalcontext [and] political ideology’ all influence national strategies (Muscat, 2008, p. 9).
Harm reduction in international policy debatesIn 1992, the Cooney Report to the European Parliament had advocated the use of needleexchange and methadone treatment programmes (Cooney, 1992). This was evidence of agrowing pragmatic approach in Europe based on harm reduction principles, reflecting asignificant shift of opinion between 1985 and the early 1990s, very much influenced byawareness of HIV/AIDS and its links to injecting drug use (Stimson, 1995). The EuropeanParliament at the time did not, however, adopt these recommendations.As illustrated in Table 3.2, there were a number of developments over the 1990s (see alsoEstievenart, 1995; Kaplan and Leuw, 1996), and in 2004 a former Interpol Chief writing inLeMondefelt able to declare the ‘war on drugs’ lost. Raymond Kendall said that it was time foran alternative approach — ‘harm reduction’ — and called for Europe to take the lead in aninternational movement to reform policy when the UN drug conventions came up for renewalin 2008. He said:Policies based solely on criminal sanctions have failed to demonstrate effectiveness. Economiccorruption increases, organised crime prospers and developing economies are hard hit bymilitary and environmental (crop eradication) interventions that have no apparent positive effect.At the same time, the marginalisation of drug users is compounded. There is therefore an urgentneed for a multi-dimensional and integrated approach, which aims at reducing both supply anddemand, and which also integrates harm reduction strategies designed to protect the health ofthe individual drug user as well as the well-being of society as a whole(Le Monde, 26 October 2004)
Is Europe now leading the policy case for harm reduction? Judged in terms of where thingswere a few decades ago, Europe does appear to have a recognisably shared approach andcountries have coordinated their policies. Importantly, Europe tends increasingly to speakwith one voice on the international stage.EU drugs policy respects the International Drugs Conventions and implements the fiveprinciples of international drug policy adopted at the UN General Assembly Special Session(UNGASS) on Drugs of June 1998 (United Nations, 1998). These principles are:sharedresponsibility— de-emphasising the distinction between producing and consuming countries;an emphasis onmultilateralism— recognising that unilateral action to single out particularcountries is ineffective; abalanced approach— controlling demand as well as controllingsupply;development mainstreaming— the drugs problem is complex and attention tosustainable development is critical; andrespect for human rights.71
Harm reduction: evidence, impacts and challenges
The EU is also playing an active role in developing UN drug policy, notably promoting theemphasis on demand reduction. For example, the Action Plan on Demand Reduction thatfollowed the 1998 UNGASS resolution rested on a set of guiding principles on demandreduction, based to an extent on ideas of harm reduction, though the term itself was notallowed — ‘adverse consequences of drug use’ was preferred. In this way, European ideascan be seen to be penetrating to the international level. More recently the EU also supportedthe UNGASS reviews, for example by preparing resolutions for the Commission on NarcoticDrugs (CND) meetings. A thematic paper drafted by the EMCDDA on the role of syringeprovision in the reduction of infectious disease incidence and prevalence was presented tothe HDG before the 2005 CND session and formed the basis of a mutually agreed positionfrom EU Member States (EMCDDA, 2004).The EU’s influence is partly levered by financial contributions: for example, between 1971 and1998 the total contribution to UN drugs-related activities through UNODC from EU countriesamounted to $535 million. Currently, EU countries contribute at least half of the UNODCbudget. Additionally, in international cooperation activities with countries that want to signassociation agreements with the EU, like Iran and Afghanistan, drug-related issues are raised,with human rights being discussed routinely. Particular attention is also given to assisting thirdcountries, especially those applying for future membership of the EU, and countries that aremain transit points for drugs reaching the EU. The EU thus reaches out to Latin America and theCaribbean, to central and south-east Asia and to West and South Africa.According to one drug policy researcher:The European Union is now mainly a single voice at international meetings with a strong andexplicit harm reduction tone even though there are signs of modest retreat from some of theboundaries of harm reduction(Reuter, 2009, p. 512)
In its evaluation of the EU drugs action plan 2005–08, the European Commission alsoconcluded that the EU is increasingly speaking with one voice in international fora, notably inthe UN CND (European Commission, 2008). It noted that the EU maintained a unifiedposition in the UNGASS review process and that during the CND Working Sessions in2006–08, the successive EU Presidencies delivered joint EU statements on the follow-up toUNGASS, drug demand reduction, illicit drug trafficking and supply, the InternationalNarcotics Control Board (INCB) and policy directives to strengthen the UNODC DrugProgramme, and the role of the CND as its governing body. The Commission, on behalf ofthe European Community, delivered its traditional statement on precursors at each CNDsession. However, the Commission warned that a harmonised approach among EU actorsduring the plenary meetings had to be maintained to ensure the EU speaks with one voice(European Commission, 2008). The EU positioned a paper in 2009 to CND noting theimportance of harm reduction, but the inclusion of the words ‘harm reduction’ in the final UNstatement were resisted, as they were a decade earlier in 1998 (International Drug PolicyConsortium, 2009). Yet, while Europe may be seen to speak with one voice at the highestelite level, it is important to note that differences remain between and within countries, andgroups organise to put pressure on these elites (see box on p. 73).72
Chapter 3: The development of European drug policy and the place of harm reduction within this
Voices against harm reductionDrug abuse is a global problem ... Even though the world is against drug abuse, someorganizations and local governments actively advocate the legalisation of drugs and promotepolicies such as ‘harm reduction’ that accept drug use and do not help drug users to becomefree from drug abuse. This undermines the international efforts to limit the supply of anddemand for drugs. ‘Harm reduction’ is too often another word for drug legalisation or otherinappropriate relaxation efforts, a policy approach that violates the UN Conventions. Therecan be no other goal than a drug-free world. Such a goal is neither utopian nor impossible.(Declaration of World Forum Against Drugs, Stockholm, Sweden, 2008)
Step-by-step developmentIt appears therefore that in drug policy as in other policy areas, incremental change hasbeen the explicit strategy of those aiming at ‘closer European Union’ (that is, achieving anincreasing proportion of common positions in policy statements), and has been activelypursued by the key actors within the dominant institutions of the EU (Hantrais, 1998; Clarke,2001, p. 34).While enlargement might have been expected to lead to greater diversity within Europe ondrug issues, oddly, convergence or harmonisation have in many ways followed theexpansion of the EU. EU accession instruments had an impact on drug policy convergenceand the adoption of harm reduction in new Member States. This is partly because theaccession countries were keen to drop all vestiges of the former Soviet system and were opento demonstrating their adherence to European values and policies. The deliberate policy ofinstitution building within the EU encouraged this process, including the coordination ofactivities aimed atsynchronisationin the conduct of reviews, publishing of strategies andaction plans and attention to the value of information and evaluation. Drugs as an issue canserve these purposes very well since drug misuse is at face value something all agree to be abad thing: through the process of deliberating on drug policy, networks develop, institutionsare formed and the wider aspects of a European approach are learnt, such as transparency,justification by reference to evidence, dialogue, and involvement of civil society.For instance, the European Union PHARE (2) programmes exercised influence over candidatecountries aiming to meet the requirements for accession. The European Commission funded amulti-beneficiary drug programme within PHARE, and the EU included national drug policyas an area of focus in its accession talks with candidate countries, which all signed the UNConventions. Many candidate countries made the prevention of trafficking of illicit drugs anarea of special attention and focus.(2)Acronym deriving from the original title of the EU assistance programme, Pologne Hongrie Assistance pour laRéstructuration Economique.
73
Harm reduction: evidence, impacts and challenges
There have thus been a number of steps in the path towards convergence: the sharedexperience of practitioners, especially those involved in tackling the heroin, HIV/AIDSand hepatitis C epidemics and treating injecting drug users (IDUs); an increasinglyshared perception of the problem, partly encouraged by dialogue around thedevelopment of information resources; the development of a common language tosupport the discourse; and the adoption of a set of common methods and reportingstandards.Forums and networks have also played a role in developing shared understandings andapproaches to the European drug problem. With the Frankfurt Resolution of November1990, representatives from the cities of Amsterdam, Frankfurt, Hamburg and Zurich resolvedthat attempts at eliminating drugs and drug consumption were a failure and that a newmodel was needed to cope with drug use in European cities (http://www.realitaeten-bureau.de/en_news_04.htm). This led to the setting up of European Cities on Drug Policy (ECDP),which helped open up the debate for a Europe-wide harm reduction drug policy approach.The direct involvement of user groups as well as epidemiologists and medical and criminaljustice and other practitioners has been another important factor. ENCOD (EuropeanCoalition for Just and Effective Drug Policies) is a European network of about 156organisations and individual citizens affected by and concerned about current drug policies.Another important network is the International Drug Policy Consortium — ‘promotingobjective and open debate of drug policies’; this brings together NGOs and professionalswho specialise in issues related to illegal drugs, while the International Harm ReductionAssociation (IHRA) has influence through its efforts to promote a harm reduction approach toall psychoactive substances on a global basis.On the other hand, there have continued below the surface to be strong opposing currents ofopinion on drug policy (see box on p. 73). In April 1994, the Stockholm resolution aimed topromote a drug-free Europe and established European Cities Against Drugs (now with 264signatory municipalities in 30 countries). In this process, Sweden played a leading role(http://www.ecad.net/resolution).
ConclusionSome have noted ‘a clear trend across Europe towards the recognition of harm reduction asan important component of mainstream public health and social policies towards problemdrug use’, representing something of a ‘sea change in European drug policies’ (Hedrich et al.,2008, p. 512). This convergence appears to have been strongly influenced by the productionof EU drugs strategies from 1999 onwards, and the development of concrete, measurabletargets, action plans and evaluation strategies. Hedrich et al. note:By including harm reduction as a key objective of drug policy, EU action plans not only reflectwhat was already happening in some Member States in response to serious public healthchallenges but [also] that European instruments further consolidated harm reduction as one of thecentral pillars of drug policy.(Hedrich et al., 2008, p. 514)
74
Chapter 3: The development of European drug policy and the place of harm reduction within this
Convergence towards ‘policy consensus’ was thus ‘mediated by EU guidance while notoriginating from it’ (Hedrich et al., 2008, p. 507).The evidence reviewed in this chapter supports a conclusion of a progressive although limitedconvergence in European drug policies and that harm reduction is both an element and anindicator of this convergence. Opioid substitution treatment and needle and syringeprogrammes have become part of the common response in Europe for reducing problemsrelated to drug injecting. This is characterised as a ‘new public health’ response to injectingdrugs and HIV/AIDS (see also Rhodes and Hedrich, 2010).EU drugs policy mixes traditional law enforcement approaches with an increasing focus onpublic health. A public health approach could be seen as relatively humane, sympatheticto those affected by drug use — both users, and families and communities — and asfollowing ethical principles (see also Fry, 2010). The public health model still, however, restson a ‘disease’ conception of drug use, framing it as an infectious and communicabledisease that can be regulated from above, using a package of measures includingsurveillance and monitoring and aiming at containment. The starting point is recognisingthat the disease is present, even if measures should try to prevent or eliminate it. The mainconcern is to reduce the risk of transmission and its development into an epidemic. Thisconception has grown in power with the arrival of HIV/AIDS, exacerbated more recentlyby hepatitis C. It is a feature of this model also to assume that some members ofpopulations are more vulnerable than others and that, although the underlying causes mayneed to be understood and tackled, in the short term the focus should be on targetingthese groups. The priority is to focus on containing and managing the disease. Thisapproach, based on scientific evidence and filtered through a range of regulatory andadvisory bodies, produces directives, recommendations and guidance documents to whichnational governments are expected to respond. These increasingly influence nationalpolicies, partly because national governments want to ‘show willing’, be part of and signedup to the European Project, and also in some cases because governments do not actuallyconsider drugs to be as important an issue as others on their busy agendas, so they do notbother to contest the matter.In reality, implementation, a crucial element in the policy process, is influenced by the degreeof acceptance by those involved of the measures suggested. Treatment professionals, serviceproviders and budget holders influence the shape of service responses, and the wider society— of non-governmental pressure groups, drug users themselves and families andcommunities — may agree or disagree about the basic values on which theserecommendations are based.Overall, however, within Europe, a coordinated and increasingly coherent ‘middle ground’policy on drugs appears to be emerging, within which harm reduction has an acceptedplace. But there is continuing tension between opposing views. A compromise may hold for awhile, but with changing circumstances and conditions further policy adaptations are likely toappear on the agenda.75
Harm reduction: evidence, impacts and challenges
AcknowledgementsThe research on which this chapter is based was supported by an Emeritus Fellowshipawarded to Susanne MacGregor by The Leverhulme Trust, for which we are very grateful.We would like to thank reviewers of drafts of this chapter for their valuable comments, whichwe have endeavoured to take into account. Any errors or faults of interpretation remain ourresponsibility.
ReferencesBergeron, H. and Griffiths, P. (2006), ‘Drifting towards a more common approach to a more common problem:epidemiology and the evolution of a European drug policy’, in Hughes, R., Lart, R. and Higate, P. (eds),Drugs:policy and politics,Open University Press, Milton Keynes, pp. 113–24.Chatwin, C. (2003),On the possibility of policy harmonisation for some illicit drugs in selected member states of theEuropean Union,Sheffield University, PhD thesis.Chatwin, C. (2007), ‘Multi-level governance: the way forward for European illicit drug policy?’,InternationalJournal of Drug Policy18, pp. 494–502.Clarke, J. (2001), ‘Globalisation and welfare states: some unsettling thoughts’, in Sykes, R., Palier, B. and Prior, P.M. (eds), Globalisationand European welfare states,Palgrave, Houndsmill, pp. 19–37.Cook, C., Bridge, J. and Stimson, G. V. (2010), ‘The diffusion of harm reduction in Europe and beyond’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Cooney, P. (1992),Report of the Committee of Inquiry on the spread of organised crime linked to drug trafficking inthe Member States of the Community,23 April, European Parliament, meeting documents, A3-0358/91.EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2004),A European perspective onresponding to blood borne infections among injecting drug users: a short briefing paper,European MonitoringCentre for Drugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/html.cfm/index5777EN.html.EMCDDA (2008),The state of the drugs problem in Europe,European Monitoring Centre for Drugs and DrugAddiction, Lisbon.EMCDDA (2009),The state of the drugs problem in Europe,European Monitoring Centre for Drugs and DrugAddiction, Lisbon.Estievenart, G. (ed.) (1995),Policies and strategies to combat drugs in Europe,European University Institute,Martinus Nijhoff Publishers, Florence.Eurobarometer (2006), ‘TNS Opinion and Social’,Public opinion in the European Union,Standard Eurobarometer,66, Autumn, European Commission. Available from http://ec.europa.eu/public_opinion/archives/eb/eb66/eb66_en.htm.European Commission (2008),Commission staff working document. Accompanying the communication from theCommission to the Council and the European Parliament on an EU drugs action plan (2009–2012) — report of thefinal evaluation of the EU drugs action plan (2005–2008),{COM(2008) 567} {SEC(2008) 2455} {SEC(2008)2454}, European Community, Brussels. Available at http://eur-lex.europa.eu/SECMonth.do?year=2008&month=09.
76
Chapter 3: The development of European drug policy and the place of harm reduction within this
Fry, C. (2010), ‘Harm reduction: an “ethical” perspective’, in Chapter 4, ‘Perspectives on harm reduction: whatexperts have to say’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction:evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10,Publications Office of the European Union, Luxembourg.Hantrais, L. (1998), ‘European and supranational dimensions’, in Alcock, P., Erskine, A. and May, M. (eds),Thestudent’s companion to social policy,Blackwell, Oxford, pp. 199–204.Hartnoll, R. L. (2003), ‘Drug epidemiology in the European institutions: historical background and key indicators’,Bulletin on NarcoticsLV (1 and 2), pp. 53–71.Hedrich, D., Pirona, A. and Wiessing, L. (2008), ‘From margin to mainstream: the evolution of harm reductionresponses to problem drug use in Europe’,Drugs: education, prevention and policy15, pp. 503–17.Hungarian Civil Liberties Union (2009),Public poll survey on drug policy attitudes in 6 EU Member States,HCLU.Available at http://eudrugpolicy.org/files/eudrugpolicy/PollReportEDPI.pdf.International Drug Policy Consortium (2009),The 2009 Commission on Narcotic Drugs and its high level segment:report of proceedings,IDPC Briefing Paper, April 2009.Kaplan, C. D. and Leuw, E. (1996), ‘A tale of two cities: drug policy instruments and city networks in theEuropean Union’,European Journal of Criminal Policy and Research4, pp. 74–89.Kendall, R. (2004), ‘Drugs: war lost, new battles’ [Drogues: guerre perdue, nouveaux combats],Le Monde26October — opinion editorial.Muscat, R. and members of the Pompidou research platform (2008),From a policy on illegal drugs to a policy onpsychoactive substances,Council of Europe Publishing, Strasbourg.Official Journal of the European Union (2008) Official Journal of the European Union C 326, 20.12.2008, PartIV: Notices from European Union Institutions and Bodies: Council,EU Drugs Action Plan for 2009–2012.Availableat: http://eur-lex.europa.eu/JOIndex.do?year=2008&serie=C&textfield2=326&Submit=Search&_submit=Search&ihmlang=en.Reuter, P. (2009), ‘Ten years after the United Nations General Assembly Special Session (UNGASS): assessingdrug problems, policies and reform proposals’,Addiction104, pp. 510–17.Rhodes, T. and Hedrich, D. (2010), ‘Harm reduction and the mainstream’, in European Monitoring Centre forDrugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts and challenges,Rhodes, T. and Hedrich,D. (eds), Scientific Monograph Series No. 10, Publications Office of the European Union, Luxembourg.Stimson, G. V. (1995), ‘AIDS and injecting drug use in the United Kingdom, 1987–1993: the policy response andthe prevention of the epidemic’,Social Science and Medicine41, pp. 699–716.United Nations (1998), ‘UN General Assembly Twentieth Special Session World Drug Problem 8–10 June’.United Nations, New York. Available at http://www.un.org/documents.United Nations (2008), ‘Economic, Social and Economic Council, Commission on Narcotic Drugs, fifty-firstsession’,The world drug problem: fifth report of the Executive Director,United Nations, Vienna, 10–14 March (E/CN.7/2008). Available at http://www.unodc.org.
77
Chapter 4Perspectives on harm reduction — what experts have to sayJürgen Rehm, Benedikt Fischer, Matthew Hickman, Andrew Ball, Rifat Atun, MichelKazatchkine, Mat Southwell, Craig Fry, Robin RoomHarm reduction is usually used as an umbrella term to define interventions, programmes andpolicies that seek to reduce the health, social and economic harms of substance use toindividuals, communities and societies. But definitions of harm reduction are also contested.At the same time, a variety of challenges face the development and implementation of harmreduction policies in Europe and elsewhere. We invited nine international experts to reflectupon harm reduction. Between them, they reflect expertise in international public healthpolicy and development (including representatives of the World Health Organization andGlobal Fund), the health and social sciences, medical ethics and user involvement. Theirtopics focus on challenges regarding:• trengthening the concept and evidence-base (Rehm and Fischer);s• reventing hepatitis C (Hickman);p• roadening the scope of interventions (Ball);b• caling up coverage (Atun and Kazatchkine);s• enerating genuine user involvement (Southwell);g• he ethics of policy decision-making (Fry); andt• ow best to think about and define what we mean by harm (Room).h
Harm reduction in an open and experimenting societyJürgen Rehm and Benedikt FischerOver the past 25 years ‘harm reduction’ has played an increasingly prominent and explicitrole in substance use policy and interventions, especially in Western Europe and Australia,but also in North America to some extent. Although people have struggled with theconcept in terms of its clarity, and there has been ideological opposition to it since itsinception, its fundamental significance is that it departs from the traditionally dominantapproach by which the severity of substance use problems is principally defined by theextent, quantity or frequency of substance use by an individual or within a population. Theimplied logic of this conventional approach to substance use suggested that abstinence,and thus reducing the prevalence of use ought to be main goals of substance use,interventions or policy.Although the principles of harm reduction stretch back several decades, harm reductionpractice was symbolically re-invented during the early phase of the HIV/AIDS epidemicamong injecting drug users (IDUs) in the 1980s. This was a time when health workers startedproviding clean syringes to IDUs — rather than seeking to achieve their abstinence from druguse — in order to halt the spread of HIV. Since then, harm reduction initiatives and79
Harm reduction: evidence, impacts and challenges
frameworks have been established for all areas of substance use, albeit not withoutsubstantial difficulty or opposition.Critics of harm reduction have claimed that the concept of ‘harm’ is not objectively defined,and therefore does not provide a strong empirical basis for the implementation andevaluation of harm reduction measures (Rehm and Fischer, 1997; Leshner, 2008; Hall, 2007).Further, it has been suggested that harm reduction approaches appear to sanction or evenenable substance use, and therefore may facilitate the ‘legalisation’ of illicit substances, andthus may send out ‘the wrong message’ (DuPont, 1996). Finally, an often-cited argument isthat harm reduction measures for illicit drugs contravene international drug control treaties,although such criticisms have been rejected both in theory and in practice (Room, 2003). Foreach of the main substantive substance use arenas (alcohol, tobacco, illicit drugs), there aredistinct harm reduction debates and initiatives. We summarise some of these below, beforesketching out an evidence- and experimental-based approach to implementing interventionsbased on harm reduction principles.
Harm reduction in different fields of substance use: commonalities anddifferencesThe term harm reduction has somewhat distinct connotations in different fields of substanceuse.AlcoholIn the alcohol field there has been recognition for some time now that abstinence may not bethe ideal or most feasible outcome of policy or therapeutic interventions, as consistent light tomoderate alcohol use without heavy drinking occasions has been shown to confer healthbenefits (Pearl, 1926; Rehm et al., 2004b; Rehm et al., 2003). Even though abstinence foreverybody is not the main goal of alcohol policy in Western societies anymore, approachesto reduce consumption in a given country or region are still presented as harm reduction(Room, 2004). However, the current use of the term has evolved, and in the debates at theWorld Health Assembly towards establishing a global strategy to reduce alcohol-attributableharm, harm reduction has been framed in different ways by many players.Despite differences of emphasis, there is an emerging consensus among alcohol experts:• hat abstinence may not necessarily be the only goal of a public health approach for the tpopulation and not even necessarily the goal of treatment for individuals who enter thetreatment system (see ‘controlled drinking’ approaches as one kind of therapy, or so-called‘wet hostels’ as one form of intervention, Podymov et al., 2006);• hat patterns and practices of drinking predominantly influence the alcohol-related harm texperienced (Rehm et al., 2003);• nd that this harm from drinking is to a substantial extent also influenced by the aenvironment and the context of drinking (Rehm et al., 2004a).80
Chapter 4: Perspectives on harm reduction — what experts have to say
Following this perspective, the risk behaviour of so-called ‘binge drinking’ (Gmel et al.,2003) has become the focus of many preventive and therapeutic interventions. Here, theadvice might be to replace the consumption of two bottles of wine in one setting on aFriday with drinking one glass of wine daily in conjunction with a meal. This change ofdrinking patterns results in about the same amount of alcohol being consumed, buttypically leads to much less health and social harm.However, closer examination shows that despite changes of language and examples, theinterventions proposed are often still the same as 40 years ago within a supposedly differentparadigm. As some of the accepted truths of the field (that is, that higher availability ofalcohol leads to more harm under all circumstances) have been empirically challenged(example: Sweden has experienced much higher availability of alcohol in the past years, butnot necessarily higher consumption or alcohol-attributable harm), the global strategy willneed a much closer examination of what interventions produce which effects under whatcircumstances, and less debate on how we label the successful interventions.TobaccoMany have argued that harm reduction cannot be applied to tobacco smoking, sincesmoking even small quantities of tobacco is associated with significant health risks (Instituteof Medicine, 2001). However, changing realities have led to a new focus on harmreduction and smoking, at least in high-income countries (Shiffman et al., 2002; Hatsukamiet al., 2004; Hughes, 1995). In many Western countries, smoking is now increasinglyconcentrated in a population of ‘hard-core’ smokers who often have symptoms ofdepression (Fergusson et al., 2003) and/or are economically disadvantaged (Barbeau etal., 2004). Such people may not be able to quit their tobacco consumption entirely, butmay be good candidates for harm reduction measures — for example, practices ofcontrolled smoking supported by alternative nicotine delivery mechanisms — that lower therisks associated with their smoking. In addition, harm reduction may offer alternativeinterventions for smokers that are less punitive or stigmatising in an increasingly harsh‘anti-smoking’ climate (Poland, 2000).Some attention has been given in this context to alternative or ‘safer’ nicotine deliverymodels that eliminate the highly carcinogenic effects of smoked tobacco inhalation bymeans of ‘cleaner’ forms of nicotine intake (Ferrence et al., 2000). These range fromvarious culture-specific forms of chewed tobacco products (e.g. ‘snus’) to nicotine gum orpatches. Some have pointed out that ‘controlled’ or ‘reduced’ smoking for certain userswould at least reduce exposure to harmful tobacco smoke and its consequences(Drinkmann, 2002; Hughes, 2000), if it is not compensated by more harmful ways ofinhaling. Studies have yet to demonstrate whether such approaches are really showing anoverall benefit for the target groups. Again, an extensive ideological debate will not reduceany of the harms associated with smoking. Rather, well-designed and executed scientificexperiments testing the benefits of different types of ‘harm reduction’ interventions forsmokers resistant to quitting may inform the best mix of interventions for different targetgroups (Rehm and Strack, 1994).81
Harm reduction: evidence, impacts and challenges
Illicit drugsUntil recently, the harm reduction approach has been equally controversial in the field of illicitdrugs (that is, drugs whose consumption is prohibited by law). Although depending on thetype of illegal drug, an accumulation of evidence over the past couple of decades points tothe substantial risks of death and disease associated with illicit drug use and specificallyunderlines the crucial role that behavioural, social and environmental factors play inaggravating or mitigating those risks (EMCDDA, 2003). Various harm reduction measureshave been used to pragmatically reduce drug-related risks especially in the area of IDU,including needle exchange programmes that are known to reduce transmission riskbehaviours for both HIV and hepatitis B and C among IDUs (Vlahov et al., 2001; Kimber etal., 2010). Supervised injection facilities — including many such operations in Europe andAustralia, and one facility in North America (‘Insite’ in Vancouver) — have become a mainintervention for IDUs and aim to reduce overdose, infectious disease and public orderproblems among IDUs by offering a protected and medically supervised drug injectingenvironment. Overall, the empirical evidence shows some success (Kimber et al., 2003;Hedrich, 2004; Hedrich et al., 2010), but the interpretation is limited by the weak designsapplied in many evaluations, often represented by the lack of adequate control groups. Thisleaves the door open for alternative interpretations of data produced and subsequentideological debate.
Towards a more evidence-based and experimental approachAlthough the term ‘harm reduction’ has different meanings within and across different fieldsof substance use, there are some clear conceptual underpinnings. First, the primary emphasiswithin this paradigm is on the outcomes of substance use rather than on use itself. Second,the major objective of intervention measures is to reduce negative outcomes, regardless ofwhether or not use is reduced.As such, harm reduction can be construed as an alternative — welcome or not — to theconventional paradigm underlying substance use interventions or policy, which has beenconcerned principally with useper se.Clearly, all fields of substance use are starkly shapedby an abundance of ideology. Harm reduction is and will remain controversial in this climate,as it challenges or deviates from conventional approaches and norms to substance use, someof which signal that any form of substance use is bad or should not be accepted or ‘aided’.Thus, simply renaming the approach may incur some short-lived gains on the rhetorical level,but may not resolve these substantive conceptual dilemmas in the long run. Rather, the use of‘harm reduction’ terminology should be avoided at the philosophical or abstract level, andinstead should be specified concretely in each instance with regard to what is meant by‘harms’, and how ‘the reduction of harm’ is supposed to occur and to be measured. Thus,harm reduction efforts in practice should be clear in their conception, based on evidence andimplemented in a way that allows their effectiveness to be evaluated. This, in consequence,also means that harm reduction measures should be revised or suspended, if they do notdeliver the intended or otherwise beneficial outcomes.82
Chapter 4: Perspectives on harm reduction — what experts have to say
In the field of substance use, ideology is a strong current, and a simple label (such as‘harm reduction’) can suffice to render certain interventions or measures as unacceptable.We must therefore find ways to move towards a more experimental and evidence-basedapproach to substance use policy and interventions (Campbell, 1969; Rehm, 2009).Measures such as supervised injection sites should be implemented with clear outcomeobjectives on a time-limited basis; the progress towards these objectives should bemonitored, and if not reached, the available — and typically scarce — resources shouldbe invested in other interventions. Furthermore, experiments on programming optionsshould be construed and implementeda prioriwith control groups, such as the Saturdayopening hours for alcohol in Sweden, where the policy was implemented in one part ofthe country, with another part of the country serving as the control group (Norström andSkog, 2003). Such control groups are very valuable in distinguishing effects ofinterventions from secular trends or concomitant events. Another example in this directionwould be the proposal for alcohol outlets in Canada to open on Sunday mornings incertain areas to avoid the use of surrogate alcohol by marginalised or poor alcoholaddicts (e.g. homeless people) who do not have enough funds to stock their requiredalcohol supply over the weekend.It is unlikely that the fundamental philosophical controversy regarding ‘harm reduction’ willever diminish or disappear. The only basis for a meaningful continued existence of harmreduction concepts will be a firm linkage with concrete definitions and operationalisations,and evidence-based assessments of whether the respective measures deliver on theirobjectives or not. These principles should also become a consistent standard for all policyframeworks relying on the harm reduction concept.
AcknowledgementThis contribution is based on and conceptually expands the contribution ‘Harm reduction’ byBenedikt Fischer inSubstance abuse in Canada: current challenges and choices(2005,Canadian Centre on Substance Abuse, Ottawa, pp. 11–15).
ReferencesBarbeau, E., Krieger, N. and Soobader, M-J., (2004), ‘Working class matters: socioeconomic disadvantage,race/ethnicity, gender, and smoking in NHIS 2000’,American Journal of Public Health94, pp. 269–78.Campbell, D. T. (1969), ‘Reforms as experiments’,American Psychologist24, pp. 409–29.Drinkmann, A. (2002), ‘Kontrolliertes Rauchen: Standortbestimmung und Perspektiven’,Suchttherapie3, pp. 81–6.DuPont, R. (1996), ‘Harm reduction and decriminalization in the United States: a personal perspective’,SubstanceUse and Misuse31, pp. 1929–45.EMCDDA (2003),Annual report: state of the drugs problem in the European Union and Norway,EuropeanMonitoring Centre for Drugs and Drug Addiction, Lisbon.
83
Harm reduction: evidence, impacts and challenges
Fergusson, D., Goodwin, L. and Horwood, L. (2003), ‘Major depression and cigarette smoking: results of a 21-year longitudinal study’,Psychological Medicine33, pp. 1357–67.Ferrence, R. G., Slade, J., Room, R. and Pope, M. A. (2000),Nicotine and public health,American Public HealthAssociation, Washington.Gmel, G., Rehm, J. and Kuntsche, E. (2003), ‘Binge drinking in Europe: definitions, epidemiology, andconsequences’,Sucht49, pp. 105–16.Hall, W. (2007), ‘What’s in a name?’,Addiction102, p. 692.Hatsukami, D., Henningfield, J. and Kotlyar, M. (2004), ‘Harm reduction approaches to reducing tobacco-relatedmortality’,Annual Review of Public Health25, pp. 377–95.Hedrich, D. (2004),European report on drug consumption rooms,European Monitoring Centre for Drugs and DrugAddiction, Lisbon.Hedrich, D., Kerr, T. and Dubois-Arber, F. (2010), ‘Drug consumption facilities in Europe and beyond’, in Rhodes,T. (ed.),Harm reduction: evidence, impacts and challenges,European Monitoring Centre for Drugs and DrugAddiction, Scientific Monograph Series No. 10, Publications Office of the European Union, Luxembourg.Hughes, J. (1995), ‘Applying harm reduction to smoking’,Tobacco Control4, pp. S33–S38.Hughes, J. (2000), ‘Reduced smoking: an introduction and review of the evidence’,Addiction95, pp. 3–7.Institute of Medicine (2001),Clearing the smoke: assessing the science base for tobacco harm reduction,Institute ofMedicine, Washington, DC.Kimber, J., Dolan, K., van Beek, I., Hedrich, D. and Zurhold, H. (2003), ‘Drug consumption facilities: an updatesince 2000’,Drug Alcohol Review22, pp. 227–33.Kimber, J., Palmateer, N., Hutchinson, S., Hickman, M. and Rhodes, T. (2010), ‘Harm reduction interventions forinjecting drug users: evidence of effectiveness’, in Rhodes, T. (ed.),Harm reduction: evidence, impacts andchallenges,European Monitoring Centre for Drugs and Drug Addiction, Scientific Monograph Series No. 10,Publications Office of the European Union, Luxembourg.Leshner, A. (2008), ‘By now, “harm reduction” harms both science and the public health’,Clinical Pharmacologyand Therapeutics83, pp. 513–14.Norström, T. and Skog, O. J. (2003), ‘Saturday opening of alcohol retail shops in Sweden: an impact analysis’,Journal of Studies on Alcohol and Drugs64, pp. 393–401.Pearl, R. (1926),Alcohol and longevity,Knopf, New York.Podymov, T., Turnbull, J., Coyle, D., Yetisir, E. and Wells, G. (2006), ‘Shelter-based managed alcoholadministration to chronically homeless people addicted to alcohol’,Canadian Medical Association Journal174(01), pp. 45–49.Poland, B. (2000), ‘The “considerate” smoker in public space: the micro-politics and political economy of “doingthe right thing”’,Health & Place6, pp. 1–14.Rehm, J. (2009), ‘Making connections — the questions we have to answer’, Presentation at the conference on theoccasion of the 15th anniversary of the European Monitoring Centre for Drugs and Drug Addiction, ‘IdentifyingEurope’s information needs for effective drug policy’, EMCDDA, Lisbon.Rehm, J. and Fischer, B. (1997), ‘Measuring harm reduction: implications for alcohol epidemiology’, in Plant, M.and Single, E.,Minimising the harm: what works?Free Association Books, London, pp. 248–61.
84
Chapter 4: Perspectives on harm reduction — what experts have to say
Rehm, J. and Strack, F. (1994), ‘Kontrolltechniken’, in Herrmann, T. and Tack, W.,Methodologische Grundlagender Psychologie: Enzyklopädie der Psychologie, Forschungsmethoden, Band 1,Hogrefe, Göttingen, pp. 508–55.Rehm, J., Room, R., Graham, K., et al. (2003), ‘The relationship of average volume of alcohol consumption andpatterns of drinking to burden of disease: an overview’,Addiction98, pp. 1209–28.Rehm, J., Fischer, B., Graham, K., et al. (2004a), ‘The importance of environmental modifiers of substance useand harm’,Addiction99, pp. 663–6.Rehm, J., Room, R., Monteiro, M., et al. (2004b), ‘Alcohol use’, in Ezzati, M., Lopez, A. D., Rodgers, A. andMurray, C. J. L. (eds),Comparative quantification of health risks: global and regional burden of disease attributableto selected major risk factors. Volume 1,WHO, Geneva, pp. 959–1109.Room, R. (2003), ‘Impact and implications of the international drug control treaties on IDU and HIV/AIDSprevention and policy’, in Fischer, B., Rehm, J. and Haydon, E. (eds),Reducing the risks, harms and costs of HIV/AIDS and injection drug use: a synthesis of the evidence base for development of policies and programs.Backgroundpaper #4, 2nd annual background dialogue on HIV/AIDS, Health Canada/ UNAIDS/Canadian InternationalDevelopment Agency, Warsaw, Poland.Room, R. (2004), ‘Alcohol and harm reduction, then and now’,Critical Public Health14, pp. 329–44.Shiffman, S., Gitchell, J., Warner, K., et al. (2002), ‘Tobacco harm reduction: conceptual structure andnomenclature for analysis and research’,Nicotine and Tobacco Research4, pp. S113–S129.Vlahov, D., Des Jarlais, D., Goosby, E., et al. (2001), ‘Needle exchange programs for the prevention of humanimmunodeficiency virus infection: epidemiology and policy’,American Journal of Epidemiology154, pp.S70–S77.
HCV prevention — a challenge for evidence-based harmreductionMatthew HickmanHarm reduction applied to substance use, such as injecting, is a form of secondary prevention.Harm reduction aims to prevent the consequence of drug use, that is, to reduce the burden ofdisease and improve the health of the population (Lenton and Single, 1998). Clearly whenonset of drug use or progression to dependence cannot be prevented then it is logical tointervene in order to reduce the potential consequences of drug use, in the same way that oncepeople have developed diabetes, obesity or high blood pressure primary prevention isreplaced by other strategies that aim to reduce potential health problems associated with theseconditions. In some chronic health problems the natural history requires life-long treatment(such as diabetes) whereas in others the disease or adverse condition can be reversed. Thelatter is true of substance use, which is often described as a ‘chronic relapsing condition’ — thatis, it may be of long duration with multiple periods of recovery and relapse before finalcessation (O’Brien and McLellan, 1996). Harm reduction, therefore, aims to reduce prematuremortality and long-term health and social problems during periods of substance use. Replacingthe term ‘harm reduction’ with ‘secondary prevention’ may please some or annoy others (Hall,2007; Weatherburn, 2009). But any name change is less important than recognising that harmreduction is like any other public health intervention (Institute of Medicine, 2007).85
Harm reduction: evidence, impacts and challenges
Evidence is required that a specific harm reduction activity is effective; that harm is reducedin order to justify ongoing support and investment; and that like any public healthintervention the evidence is assessed in standard ways and compiled from study designs thatcan properly test whether exposure to the harm reduction intervention has reduced harm. Inthe hierarchy of study designs randomised control trials give the strongest evidence — if theresearch question and exposure lends itself to a trial. Next in the hierarchy come cohortstudies and case control designs, which separate and attempt to clarify clearly therelationship between exposure and outcome. Cross-sectional or ecological study designs maycorroborate or raise hypotheses — but cannot by themselves test them. Nonetheless it shouldbe possible to generate good-quality evidence (even without a trial), especially byconsidering consistency of evidence across different studies, different study designs andsettings (Rutter, 2007).Harm reduction or drug harms are collective nouns and cannot be reviewed as a whole.They encompass many forms of harm reduction (encompassing psychological andpharmacological therapies, provision of sterile drug taking equipment, and changes to therisk environment) and multiple harms (from neurocognitive deficit, psychological andpsychiatric impairment, crime, family and social problems, and acute and chronic ill-health)(Horne, 2007).So let us consider a specific area — harm reduction and injecting drug use — associatedwith marked levels of harm, a range of interventions, and novel intervention development.There is good evidence from trials and well-conducted observational cohort studies thatmethadone reduces the risk of overdose, and can have a role in reducing HIV infectionamong injectors (Institute of Medicine, 2007). There is weaker direct evidence but goodevidence from cost-effectiveness models that needle and syringe programmes reduce HIVtransmission. More challenging for harm reduction, and what I want to focus on, is its role inpreventing hepatitis C virus (HCV).HCV is a comparatively common blood-borne infection that may lead to liver cirrhosis,cancer and death. In the United Kingdom — and many other countries in Europe — 80 % ofinfections are due to injecting drug use and nearly 0.5 to 1 % of the adult population maybeinfected with HCV (De Angelis et al., 2008). The risk of becoming infected with HCVincreases with injecting duration, and in many cities in Europe one in two active IDU will beinfected with HCV (Hickman et al., 2007). Two key harm reduction interventions that mayreduce HCV transmission are: (i) needle and syringe programmes (NSPs), which aim toreduce the use and sharing of injecting equipment that maybe infected with HCV; and (ii)opioid substitution treatment (OST), which in the context of HCV aims to reduce injectingfrequency and thereby reduce the probability of sharing and increase coverage of NSPs.The first challenge and obvious policy question is — what evidence is there that harmreduction reduces HCV transmission? Unfortunately there is very little direct evidence (ACMD,2009). For example, Jo Kimber, Norah Palmateer and colleagues report overwhelmingevidence from reviews and individual studies that NSP and OST reduce self-reportedinjecting risk (Kimber et al., 2010; Palmateer et al., 2010). However, there is insufficientreview-level evidence that NSP or OST are associated with a reduction in HCV incidence.86
Chapter 4: Perspectives on harm reduction — what experts have to say
Does this matter? It might simply be because the studies are too small or underpowered todetect a difference in HCV incidence; if the outcomes are combined (reported sharing andHCV incidence) then the evidence is positive. However, it does matter. Reported injecting riskbehaviour change is not a good enough marker of reduced HCV transmission. There aremany cross-sectional surveys and longitudinal surveys of IDU that find reported sharing to bea poor predictor of HCV infection — with high rates of HCV among people who report‘never sharing’, and comparatively small increased rates of infection among people whoreport sharing. Reported injecting risk may be misclassified or may be under- or over-reported due to social desirability or other reasons. More importantly, even if a reduction insharing occurred, without information on HCV incidence we cannot be certain that thereduction was sufficient to reduce HCV transmission. We cannot rule out the possibility thatNSP or OST are having no effect on HCV transmission.However, we know that OST and NSP are beneficial for other health outcomes. So thechallenge and policy question should really be — what level of harm reduction is required toreduce HCV transmission? How much extra may be required? We know that in many otherEuropean countries HCV prevalence among IDU remains persistently high. In the UnitedKingdom, HCV prevalence has doubled among recent injectors in the last 10 years —evidence that current interventions and coverage are insufficient (Sweeting et al., 2009). Incontrast, there is some evidence that HCV incidence has fallen in Amsterdam (van den Berget al., 2007a). Indeed there is emerging evidence from the Amsterdam Addiction Cohort(AAC) of a positive intervention effect of harm reduction against HCV incidence (van denBerg et al. 2007b). IDU who were on ‘full’ harm reduction’ (that is, on OST and highcoverage NSP — receiving a sufficient number of syringes for the reported number ofinjections) had an HCV incidence approximately one-third lower than those receiving eitherOST or NSP. HCV incidence among IDU-receiving ‘partial or incomplete harm reduction’ wasno different from IDU receiving no harm reduction; and there was no evidence of anintervention effect for NSP or OST alone.The implication of the evidence from AAC is stark and far-reaching. If true, and we observea similar picture in the United Kingdom (unpublished), then HCV incidence can be reduced,but providing a small amount of harm reduction is insufficient — partial harm reduction willnot have an impact on HCV transmission. Further, only the combination of interventionsseemed to have an effect. Perhaps the reason why there is no review-level evidence of anintervention effect in the literature is because studies have been investigating a singleintervention (e.g. NSP vs. no NSP), and not assessing sites and subjects in OST with highlevels of NSP coverage. It is not difficult to see why partial harm reduction may not beenough. If you live in a site where one in two IDU are infected with HCV, and the probabilityof HCV transmission after sharing an infected syringe is, say, 3.5 %, then you only need toshare about 40 times to have a 50:50 chance of being infected with HCV. If you inject 500times a year then even if you are safe 95 % or more of the time, it does not take many yearsfor your chance of being HCV positive to become very high.This evidence leads to two further challenges. We need to strengthen the evidence base onwhat level and combination of harm reduction interventions reduce HCV transmission(Hickman, 2009). This is not trivial. Randomised control trials, at least for OST and NSP,87
Harm reduction: evidence, impacts and challenges
cannot be used, as it would be unethical to randomise interventions that have proven benefiton other health outcomes. This may not be the case for other interventions, which, therefore,could be randomised alongside OST and NSP. Equally, longitudinal studies are expensiveand difficult to conduct well and achieve high rates of follow-up. Instead, innovative methodsmay be required that make use of different serological markers of HCV infection to identifyincident infections — and compare HCV incidence against different harm reductionexposures. A further complication is that these studies need to investigate and measure theimpact of different combinations of harm reduction intervention.Finally, the challenge of HCV prevention to harm reduction providers and advocates is thatservices need to interact and combine. Providing sterile equipment or offering OST may notbe enough; but the two need to work together. Reducing injecting frequency and achievinginjecting cessation must become prominent goals of HCV harm reduction in order for thereduction in injecting risk and the scale of behaviour change required to prevent HCV to besustainable.
ReferencesACMD (Advisory Council on Misuse of Drugs) (2009),The primary prevention of hepatitis C among infecting drugusers,Hickman, M. (ed.), Home Office, London.De Angelis, D., Sweeting, M., Ades, A. E., et al. (2009), ‘An evidence synthesis approach to estimating hepatitis Cprevalence in England and Wales’,Statistical Methods in Medical Research18, pp. 361–79.Hall, W. (2007), ‘What’s in a name?’,Addiction102 (5), p. 692.Hickman, M. (ed.) (2009),The primary prevention of hepatitis C among infecting drug users,Advisory Council onMisuse of Drugs,Home Office, London.Hickman, M., Hope, V., Brady, T., et al.(2007), ‘Hepatitis C virus (HCV) prevalence, and injecting risk behaviourin multiple sites in England in 2004’,Journal of Viral Hepatitis14 (9), pp. 645–52.Horne, G. (ed.) (2007), ‘Brain science’,Addiction and drugs,Academy Medical Sciences, London.Institute of Medicine (2007)Preventing HIV infection among injecting drug users in high-risk countries: an assessmentof the evidence,Committee on the Prevention of HIV Infection Among Injecting Drug Users in High-Risk Countries,Institute of Medicine, Washington, DC.Kimber, J., Palmateer, N., Hutchinson, S., et al. (2010), ‘Harm reduction among injecting drug users: evidence ofeffectiveness’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction:evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10,Publications Office of the European Union, Luxembourg.Lenton, S. and Single, E. (1998), ‘The definition of harm reduction’,Drug and Alcohol Review17 (2), pp. 213–19.O’Brien, C. P. and McLellan, A. T. (1996), ‘Myths about the treatment of addiction’,Lancet347 (8996), pp. 237–40.Palmateer, N., Kimber, J., Hickman, M., et al. (2010), ‘Evidence for the effectiveness of sterile injecting equipmentprovision in preventing hepatitis C and HIV transmission among injecting drug users: a review of reviews’,Addiction(in press).Rutter, M. (2007),Identifying the environmental causes of disease,Academy Medical Sciences, London.
88
Chapter 4: Perspectives on harm reduction — what experts have to say
Sweeting, M. J., Hope, V. D., Hickman, M., et al. (2009), ‘Hepatitis C infection among injecting drug users inEngland and Wales (1992–2006): there and back again?’,American Journal of Epidemiology170 (3), pp. 352–60.van den Berg, C. H., Smit, C., Bakker, M., et al. (2007a), ‘Major decline of hepatitis C virus incidence rate overtwo decades in a cohort of drug users’,European Journal of Epidemiology22 (3), pp. 183–93.van den Berg, C., Smit, C., van Brussel, G., Coutinho, R. and Prins, M. (2007b), ‘Full participation in harmreduction programmes is associated with decreased risk for human immunodeficiency virus and hepatitis C virus:evidence from the Amsterdam Cohort Studies among drug users’,Addiction102 (9), pp. 1454–62.Weatherburn, D. (2009), ‘Dilemmas in harm minimization’,Addiction104 (3), pp. 335–9.
Broadening the scope and impact of harm reduction for HIVprevention, treatment and care among injecting drug usersAndrew BallDrug use is associated with multiple and changing health risks and harms, requiringincreasingly diversified and complex responses. There is an emerging consensus that harmreduction programmes need to be comprehensive and flexible if they are to achievesignificant public health outcomes. The example of HIV prevention, treatment and careamong injecting drug users illustrates the importance of adopting a broader rather than amore restrictive definition of harm reduction (Ball, 2007a). Harm reduction programmes onthe ground need to move beyond single interventions (such as needle exchange programmesand opioid substitution treatment) delivered in isolation, to a comprehensive set ofinterventions linked in with broader health and social services.How broad should the harm reduction net be cast? Within the context of HIV and injectingdrug use there are multiple intervention points where HIV risk and harm can be reduced,including by decreasing HIV vulnerability and risk, preventing HIV transmission, treatingthose who are infected and mitigating the impact of HIV on communities. Considering ahierarchy of harm reduction goals, first, interventions can focus on those individuals andpopulations who are most vulnerable to adopting HIV risk behaviours (such as moving fromnon-injecting to injecting drug use) or are exposed to HIV risk settings (such as incarceration),but have yet to engage in risk behaviours. The aim of such interventions is to reducevulnerability by addressing such factors as stigma and discrimination, marginalisation,gender inequity and criminalisation (UNAIDS, 2008). Second, for those who are alreadyengaged in HIV risk behaviours interventions should target those behaviours to reduce risk,such as the use of opioid substitution treatment and needle and syringe programmes toreduce sharing of injecting equipment (Institute of Medicine, 2007). Some injecting drug usersare more vulnerable than others, such as female drug users, prisoners and those in ruralareas, because their situations prevent them from adopting safer behaviours or accessingprevention services. Third, where individuals are exposed to HIV, interventions for preventingor reducing HIV transmission may be considered, such as the use of antiretroviral drugs forpost-exposure prophylaxis and the potential use of HIV vaccines and pre-exposureprophylaxis when they become available (Smith et al., 2005). Fourth, where transmission has89
Harm reduction: evidence, impacts and challenges
already occurred interventions (including antiretroviral treatment) can aim to protect thehealth of those drug users living with HIV and to prevent onward transmission of HIV to theirsexual and drug-using partners and to infants, including via ‘positive prevention’ interventions(WHO, 2008). Fifth, for those who become ill, treatment and care can reduce HIV-relatedmorbidity and mortality and prevent and manage co-infections and co-morbidities (Ball,2007b). And finally, interventions can focus on mitigating the social and economic impact ofHIV on drug users, their families and communities, such as through social health insuranceschemes and care for HIV orphans (Souteyrand et al., 2008; UNICEF, 2007).Despite multiple opportunities for reducing HIV-related harm among injecting drug users,most harm reduction programmes still focus on a limited number of interventions, particularlythose that target specific HIV risk behaviours. Since the mid-1980s, the ‘big three’interventions have been risk reduction communication (particularly through community-basedoutreach), needle and syringe programmes and drug dependence treatment (notably opioidsubstitution treatment for opioid users). For these interventions the evidence of effectiveness isstrong and the feasibility of implementation has been demonstrated in some of the poorestand most difficult settings (Institute of Medicine, 2007; Needle et al., 2005; Wodak andCooney, 2005; Farrell et al., 2005). In recent years, HIV treatment has been added to the list,with increasing evidence that people living with HIV who use drugs can achieve goodoutcomes with antiretroviral therapy (Lert and Kazatchkine, 2007). The World HealthOrganization (WHO), the United Nations Office on Drugs and Crime (UNODC) and theJoint United Nations Programme on HIV/AIDS (UNAIDS) have defined a broader package ofinterventions for HIV prevention, treatment and care among injecting drug users, adding fiveinterventions to make nine ‘priority interventions’ (WHO et al., 2009b):• eedle and syringe programmes;n• rug dependence treatment;d• ehaviour change communication;b• IV testing and counselling (WHO and UNODC, 2009);H• IV treatment and care;H• ondom promotion;c• revention and treatment of sexually transmitted infections (Aral et al., 2005; Coffin et al., p2009);• revention and treatment of viral hepatitis (Bottecchia et al., 2007; Hellard et al., 2009; pWHO Regional Office for Europe, 2006);• nd tuberculosis prevention, diagnosis and treatment (WHO et al., 2008).aIn addition, a programmatic framework is required to take these interventions to scale,including strategies to establish supportive policy and community environments, betterengage civil society and other partners, build robust systems for service delivery, andstrengthen strategic information to guide responses.The situation is dynamic, with new developments having implications for how harm reductionprogrammes might be structured in the future. Research on new HIV prevention interventions90
Chapter 4: Perspectives on harm reduction — what experts have to say
needs to be monitored closely to determine their relevance for harm reduction programmes.For example, there is a widening discourse on the role of antiretroviral drugs in theprevention of HIV transmission. A pre-exposure prophylaxis trial in Thailand, involving 2 400HIV-negative injecting drug users, is studying the safety and efficacy of oral tenofovir forreducing HIV transmission among injecting drug users (CDC, 2009). Whereas the use ofantiretroviral post-exposure prophylaxis has become routine practice in many occupationalsettings, consideration needs to be given to its wider use in non-occupational settings,including for injecting drug users (WHO and ILO, 2007). Recent studies suggest thatsuppression of viral load through antiretroviral therapy decreases the risk of HIV transmissionbetween HIV-discordant couples (Reynolds et al., 2009). Several modelling exercises haveconsidered the role of antiretroviral therapy in preventing the sexual transmission of HIV(Montaner et al., 2006; Granich et al., 2009), and in controlling HIV epidemics amonginjecting drug users (Bastani et al., 2010).Harm reduction programmes should benefit from new developments in HIV/AIDS treatment,care and support. New evidence is emerging that earlier initiation of antiretroviral therapy isassociated with better treatment outcomes (NIAID, 2009). This has significant implications forprioritising HIV testing and counselling in harm reduction programmes, to ensure that the HIVstatus of drug users is determined early so that treatment initiation and prevention efforts maybe optimised. The majority of injecting drug users in low- and middle-income countries areunaware of their HIV status. In a survey of 44 low- and middle-income countries in 2008, some25 countries reported on the percentage of injecting drug users who had received an HIV testand test result in the past 12 months, with a median of only 23 % of injecting drug usersknowing their HIV status (WHO et al., 2009a). The promotion of provider-initiated HIV testingand counselling (PITC) and the use of rapid HIV testing technologies is particularly relevant forharm reduction programmes, given that follow-up of individuals may be difficult (WHO andUNODC, 2009). In 2006, out of 44 European countries surveyed, 32 provided PITC specificallyfor injecting drug users (EuroHIV, 2007). The emergence of simpler, better tolerated and morerobust antiretroviral therapy regimens offer opportunities for better treatment outcomes in drug-using populations where treatment adherence and toxicity continue to pose major challenges(Lert and Kazatchkine, 2007). Female drug users should benefit from new approaches to theprevention of mother-to-child transmission of HIV (WHO, 2009) and interventions foraddressing gender-based violence (WHO, 2007). There is also increasing recognition thatharm reduction programmes should address the broader health care needs of drug users livingwith HIV, including the prevention and management of common opportunistic infections(notably tuberculosis) (WHO et al., 2008), co-infections (including viral hepatitis and sexuallytransmitted infections) and co-morbidities (such as mental health disorders), in addition toaddressing their sexual and reproductive health needs and rights (GNP+ et al., 2009).While much attention is given to specific HIV prevention technologies and treatmentapproaches let us not forget about the broader range of interventions that make for a trulycomprehensive response, such as structural interventions for reducing HIV vulnerability andsocial protection for affected families and communities (Rhodes and Simić, 2005; UNAIDS,2008). Furthermore, little consideration has been given to the potential role within harmreduction programmes of new or promising biomedical technologies for the prevention ofsexual transmission of HIV, such as male circumcision and topical microbicides (Padian et al.,91
Harm reduction: evidence, impacts and challenges
2008). Today, with the global economic downturn and competing public health anddevelopment priorities, we can anticipate ever-louder calls for prioritisation of investments anddefinition of essential packages of interventions. While this may be an opportunity to bringgreater focus to our harm reduction work, we need to ensure that in doing so our public healthgoals of universal access, health equity and social health protection are not compromised.Certainly, priority must be given to protecting investments in already proven high-impactinterventions, such as needle and syringe programmes and opioid substitution treatment. Inaustere times, can we justify expanding the harm reduction package to include newinterventions when coverage of the ‘core’ harm reduction interventions remains abysmally lowin most countries? Decisions will need to be guided by solid evidence. More efficient andeffective models of service delivery are required, including the integration of harm reductioninterventions into other relevant health services, such as primary health care, sexual andreproductive health, mental health and tuberculosis services. To garner broad support, we needto demonstrate that harm reduction programmes and services contribute to, and are part of,broader health and community systems that strengthen and contribute to broader health anddevelopment outcomes — that harm reduction is a public good worth investing in.
ReferencesAral, S. O., St Lawrence, J. S., Dyatlovb, R. and Kozlovb, A. (2005), ‘Commercial sex work, drug use, andsexually transmitted infections in St. Petersburg, Russia’,Social Science and Medicine60 (10), pp. 2181–90.Ball, A. L. (2007a), ‘HIV, injecting drug use and harm reduction: a public health response’,Addiction102, pp.197–214.Ball, A. L. (2007b), ‘Universal access to HIV/AIDS treatment for injecting drug users: keeping the promise’,International Journal of Drug Policy18, pp. 241–5.Bastani, P., Hogg, R. S., Marshall, B. et al. (2010), ‘Highly active antiretroviral therapy eliminates HIV epidemicsin a network model of an injecting drug user community.’ Abstract 997. 17th Conference on Retroviruses andOpportunistic Infections, San Francisco, 16–19 February 2010. Available at http://www.retroconference.org/2010/PDFs/997.pdfBottecchia, M., Garcia-Samaniego, J. and Soriano, V. (2007), ‘The implications of antiviral drugs with activityagainst hepatitis B virus and HIV’,Current Opinion in Infectious Diseases20, pp. 621–8.CDC (Centers for Disease Control and Prevention) (2009), ‘CDC’s clinical studies of pre-exposure prophylaxis forHIV prevention’, Atlanta: Centers for Disease Control and Prevention. Available at http://www.cdc.gov/hiv/resources/qa/prep.htm.Coffin, L. S., Newberry, A., Hagan, H., et al. (2009), ‘Syphilis in drug users in low and middle income countries’,International Journal of Drug Policy,DOI: 10.1016/i.drugpo.2009.02.008.EuroHIV (2007),Report on the EuroHIV 2006 survey on HIV and AIDS surveillance in the WHO European Region,Institute de Veille Sanitaire, St Maurice.Farrell, M., Gowing, L., Marsden, J., Ling, W. and Ali, R. (2005), ‘Effectiveness of drug dependence treatment inHIV prevention’,International Journal of Drug Policy16 (Supplement 1), pp. S67–S75.GNP+, ICW, Young Positives, et al. (2009),Advancing the sexual and reproductive health and human rights ofpeople living with HIV: a guidance package,GNP+, Amsterdam.
92
Chapter 4: Perspectives on harm reduction — what experts have to say
Granich, R. M., Gilks, C. F., Dye, C., et al. (2009), ‘Universal voluntary HIV testing with immediate antiretroviraltherapy as a strategy for the elimination of HIV transmission: a mathematical model’,Lancet373, pp. 48–57.Hellard, M., Sacks-Davis, R. and Gold, J. (2009), ‘Hepatitis C treatment for injection drug users: a review of theavailable evidence’,Clinical Infectious Diseases49, pp. 561–73.Institute of Medicine Committee on the Prevention of HIV Infection Among Injecting Drug Users in High-RiskCountries (2007),Preventing HIV infection among injecting drug users in high-risk countries: an assessment of theevidence,The National Academies Press, Washington, DC.Lert, F. and Kazatchkine, M. (2007), ‘Antiretroviral HIV treatment and care for injecting drug users: an evidence-based overview’,International Journal of Drug Policy18 (4), pp. 255–61.Montaner, J. S., Hogg, R., Wood, E., et al. (2006), ‘The case for expanding access to highly active antiretroviraltherapy to curb the growth of the HIV epidemic’,Lancet368, pp. 531–6.Needle, R. H., Burrows, D., Friedman, S. R., et al. (2005), ‘Effectiveness of community-based outreach inpreventing HIV/AIDS among injecting drug users’,International Journal of Drug Policy16 (Supplement 1), pp.S45–S57.NIAID (National Institute of Allergy and Infectious Disease) (2009), ‘Starting antiretroviral therapy earlier yieldsbetter clinical outcomes: interim review leads to early end of clinical trial in Haiti’, NIH News Release, 8 June.Available at http://www3.niaid.nih.gov/news/newsreleases/2009/CIPRA_HT_01.htm.Padian, N. S., Buvé, A., Balkus, J., Serwadda, D. and Cates, W. (2008), ‘Biomedical interventions to prevent HIVinfection: evidence, challenges, and the way forward’,Lancet372 (9638), pp. 585–99.Reynolds, S., Makumbi, F., Kagaayi, J., et al. (2009), ‘ART reduced the rate of sexual transmission of HIV amongHIV-discordant couples in rural Rakai, Uganda’,16th Conference on Retroviruses and Opportunistic Infections,Abstract 52a.Rhodes, T. and Simić, M. (2005), ‘Transition and the HIV risk environment’,BMJ331, pp. 220–3.Smith, D. K, Grohskopf, L. A., Black, R. J., et al. (2005), ‘Antiretroviral postexposure prophylaxis after sexual,injection-drug use, or other nonoccupational exposure to HIV in the United States: recommendations from the USDepartment of Health and Human Services’,Morbidity and Mortality Weekly Report54 (RR02), pp. 1–20.Souteyrand, Y. P., Collard, V., Moatti, J. P., Grubb, I. and Guerma, T. (2008), ‘Free care at the point of servicedelivery: a key component for reaching universal access to HIV/AIDS treatment in developing countries’,AIDS22(Supplement 1), pp. S161–S168.UNAIDS (Joint United Nations Programme on HIV/AIDS) (2008), ‘Addressing societal causes of HIV risk andvulnerability’, in2008 report on the global AIDS epidemic,UNAIDS, Geneva.UNICEF (United Nations Children’s Fund) (2007),Enhanced protection for children affected by AIDS,UNICEF, NewYork.WHO (World Health Organization) (2007),Expert meeting on the primary prevention of intimate partner violenceand sexual violence, May 2–3 2007, Geneva, Switzerland: meeting report,WHO, Geneva. Available at http://www.who.int/violence_injury_prevention/violence/activities/who_ipv_sv_prevention_meeting_report.pdf.WHO (2008),Essential prevention and care interventions for adults and adolescents living with HIV in resource-limited settings,WHO, Geneva.WHO (2009), ‘Rapid advice: use of antiretroviral drugs for treating pregnant women and preventing HIVinfection in infants’, WHO, Geneva. Available at http://www.who.int/hiv/pub/mtct/rapid_advice_mtct.pdf
93
Harm reduction: evidence, impacts and challenges
WHO Regional Office for Europe (2006),Prevention of hepatitis A, B and C and other hepatotoxic factors in peopleliving with HIV/AIDS: clinical protocol for the WHO European Region,WHO, Copenhagen.WHO and ILO (International Labour Organization) (2007),Post-exposure prophylaxis to prevent HIV infection: jointWHO/ILO guidelines on post-exposure prophylaxis (PEP) to prevent HIV infection,WHO, Geneva.WHO and UNODC (United Nations Office on Drugs and Crime) (2009),Guidance on testing and counselling forHIV in settings attended by people who inject drugs: improving access to treatment, care and prevention,WHO, Manila.WHO, UNAIDS and UNICEF (2009),Towards universal access: scaling up priority HIV/AIDS interventions in thehealth sector: 2009 Progress report,WHO, Geneva.WHO, UNODC and UNAIDS (2008),Policy guidelines for collaborative TB and HIV services for injecting and otherdrug users: an integrated approach,WHO, Geneva.WHO, UNODC and UNAIDS (2009),Technical guide for countries to set targets for universal access to HIVprevention, treatment and care for injecting drug users,WHO, Geneva.Wodak, A. and Cooney, A. (2005), ‘Effectiveness of sterile needle and syringe programmes’,InternationalJournal of Drug Policy16 (Supplement 1), pp. S31–S44.
Translating evidence into action — challenges to scaling up harmreduction programmes in Europe and Central AsiaRifat Atun and Michel KazatchkineThe exceptionality of the HIV/AIDS epidemic has long been acknowledged: it is shaped byand yet also impacts on socio-economic, political, cultural and legal environments, as wellas individual beliefs and norms (Rhodes, 2002). This complex interplay of factorsinfluencing the epidemic is particularly evident in concentrated epidemics driven byinjecting drug use, as drug use is strongly influenced by macro-environmental factors suchas political and economic changes, as well as socio-cultural and legal norms in particularsettings. In many cases this leads to stigmatisation, marginalisation and isolation ofinjecting drug users (IDUs). Whilst evidence strongly suggests that HIV transmission drivenby injecting drug use can be halted and reversed through effective multi-component harmreduction programmes (Ball et al., 1998; Institute of Medicine, 2007), this evidence hasbeen overlooked or disregarded by policymakers in many countries. Consequently, inmany parts of the world, injecting drug use is still fuelling HIV epidemics. Europe, a settingwith contrasting policies to control HIV epidemics amongst IDUs and various levels ofsuccess with these policies, provides valuable evidence and a learning example to informpolicy decisions on harm reduction programmes.The countries of western Europe (1), through wide-scale implementation of needle and syringeprogrammes (NSPs), opioid substitution treatment (OST), outreach, and education(1)These include Albania, Andorra, Austria, Belgium, Bosnia and Herzegovina, Bulgaria, Croatia, Czech Republic,Denmark, Estonia, Finland, former Yugoslav Republic of Macedonia, France, Germany, Greece, Hungary, Iceland,Ireland, Italy, Latvia, Liechtenstein, Lithuania Luxembourg, Malta, Monaco, Montenegro, Netherlands, Norway, Poland,Portugal, San Marino, Serbia, Slovenia, Slovakia, Romania, Spain, Sweden, Switzerland and United Kingdom.
94
Chapter 4: Perspectives on harm reduction — what experts have to say
programmes implemented in the late 1980s and 1990s, were able to halt (such as the UnitedKingdom) or control (such as France, Italy, Spain) IDU-driven HIV epidemics (Stimson, 1995;Matic et al., 2008; Atun et al., 2008). Similarly, the central European countries of the CzechRepublic, Poland, Slovakia, and Slovenia, which experienced rapid socio-economic, politicaland cultural transitions, were also able to stabilise their HIV epidemics at low prevalence byresponding early through the implementation of effective control measures andcomprehensive harm reduction (Donoghoe, 2006). Consequently, in western and centralEurope, as of 2008, the reported number of new cases of HIV amongst injecting drug usershad declined: accounting for a smaller proportion of the HIV burden than previously(UNAIDS and WHO, 2008). By contrast, former Soviet Union countries in eastern Europeand central Asia (2), which, following the dissolution of the Soviet Union in the early 1990s,were subject to rapid socio-economic, political and cultural transitions, experienced IDU-driven HIV epidemics (Rhodes et al., 1999), which today are persisting and worsening. Ineastern European countries, the response to the IDU HIV transmission was slow andcompromised by health systems unequipped to handle the rapid increase in the burden ofHIV (Rhodes and Simic, 2005). Even now, though harm reduction programmes are beingimplemented in all countries of eastern Europe, coverage is woefully inadequate to have anyimpact on the epidemics these countries face (Donoghoe, 2006). This is evidenced by thecurrent trend of rising HIV incidence amongst injecting drug users in eastern Europe(Wiessing et al., 2008). Of particular concern are the persistent inequities in access toprevention and treatment services and access to antiretroviral therapy (Atun et al., 2008;Donoghoe et al., 2007).To stem the HIV epidemics in eastern Europe, and to address the unacceptable inequities inaccess to antiretroviral therapy, it is essential to establish and scale-up comprehensive harmreduction programmes that incorporate NSPs and OST and ensure they are implemented inprisons in both western and eastern Europe. However, in many countries this expansion ishindered by inadequate provision in the legislation that protects the human rights of IDUsand by laws that criminalise injecting drug use and harm reduction programmes. Thiscontributes to deep stigmatisation, and further isolation of this particularly at-risk group.However, in addition to legislative and regulatory barriers, other factors influence the scale-up of harm reduction programmes. We consider here the published literature to identify‘barriers’ and ‘enablers’ to scaling up harm reduction programmes in Europe in order tobetter understand the challenges that need to be addressed to translate evidence into action.
Health system organisationMany countries in eastern Europe have inherited vertically organised health systems, withparallel subsystems for HIV prevention and care, and substance use. These services aredelivered by highly specialised providers, with little structural and operational integration of theservices provided. This leads to fragmentation of services, prevents continuity of care andcreates barriers for IDUs, a marginalised group who have poor access to services (Atun, 2006).(2)These include Armenia, Azerbaijan, Belarus, Georgia, Moldova, Russian Federation, Ukraine, while central Asiancountries include Kazakhstan, Kyrgyz Republic, Tajikistan, Turkmenistan and Uzbekistan.
95
Harm reduction: evidence, impacts and challenges
This structural anomaly, which served well in the past, is not suited to the rapid implementationand scale-up of integrated responses to the IDU-driven HIV (and hepatitis) epidemics faced bythese countries. Consequently, services that offer a suitable package of prevention, treatmentand care are very limited in number, and when available they are largely inaccessible(Bobrova et al., 2007). For example, in Ukraine, the policy that permits only narcologists toprescribe OST has hindered scale-up of integrated harm reduction services (Bruce et al., 2006).As a result, only 0.1 % of IDUs are reached by this effective treatment (Matic et al., 2008).Ukraine is not alone in this practice; limiting the prescribing of OST to narcologists is commonin most east European health systems — a feature that deters IDUs from seeking and adheringto effective treatment (Donoghoe, 2006). However, experience suggests that with appropriateservice design these structural barriers can be overcome. In the Russian Federation, wheresimilar structural rigidities exist and where consequently only 1–4 % of IDUs are reached byNSPs (Wiessing et al., 2009), decentralisation of these activities by including peer network andpharmacy distribution has boosted service coverage in areas where new service deliverymodels have been adopted (Sarang et al., 2008; Sharma et al., 2007). In contrast, evidencefrom transition countries such as Croatia, Lithuania, Poland and Slovenia, which soon aftertransition in the 1990s adopted integrated models of treatment and care for HIV positive IDUs,suggests increased service accessibility for patients (Sarang et al., 2007). In countries such asIreland, the Netherlands, Norway, Sweden, and the United Kingdom, where in addition tospecialised community- or hospital-based clinics general practitioners also provide HIV careand treatment services, service coverage and usage are high, with users reporting highsatisfaction with services provided in the community and by general practitioners (Atun, 2006).
Political support and leadershipIn western Europe, early in the HIV epidemic, support for harm reduction programmes bypolitical leaders created an enabling environment for rapid introduction and scale-up of OST,NSPs and treatment and care programmes for IDUs. For example, in 1993 an initiative thatintroduced harm reduction in France was followed between 1995 and 2003 by the rapidscale-up of OST services. This led to a reduction in unsafe injection practices and a decline inHIV prevalence from 40 % to 20 % in the same period (Emmanuelli and Desenclos, 2005). Inthe United Kingdom, the health authorities, which enjoy substantial operational autonomy,were able to provide local leadership to establish service delivery units to quickly implementNSPs, outreach services, and integrated models of OST where a range of doctors couldprescribe methadone (Stimson, 1995).In contrast, experience in eastern Europe is one of lack of leadership and politicalcommitment to harm reduction. In Armenia, Russia, Tajikistan and Turkmenistan lack ofobvious political support for harm reduction has meant that critical activities such as needleand syringe provision were not mainstreamed within the national HIV response, while thetotal prohibition of OST meant a comprehensive programme could not be mounted. A lack ofpolitical support and negative perceptions on harm reduction as a ‘Western concept’ at oddswith the culture and norms in Russia has meant limited public funds being allocated toprogrammes to address the needs of IDUs (Tkatchenko-Schmidt et al., 2007). A strongly96
Chapter 4: Perspectives on harm reduction — what experts have to say
hostile legislative environment and socio-cultural intolerance in many countries to drug usefurther hindered attempts to develop NSPs and fuelled the practice of syringe sharingamongst IDUs who feared searches by police for injection equipment and possibleincarceration (Rhodes et al., 2004). Likewise, Ukraine, one of the first eastern Europeancountries to implement OST pilot projects, has been slow in scaling up these programmesdue to resistance amongst the political leadership and some providers coupled with ashortage of financial resources and trained healthcare professionals. To date, there are onlyhigh-threshold services in the country (Matic et al., 2008, Schumacher et al., 2007).
Insufficient domestic financingAn important barrier to scaling up harm reduction programmes in eastern Europe relatesto limited domestic funding allocated to HIV programmes, especially to prevention activitiesand targeted interventions for high-risk groups (Matic et al., 2008; Dehne et al., 2000).Though Belarus in its national AIDS programme had plans to set up NSPs nationwide,these could not be established due to financial shortfalls for programme implementation(Sarang et al., 2007).The Global Fund to Fight AIDS, Tuberculosis and Malaria has provided much-needed fundingfor programmes targeting injecting drug users and other at-risk groups, such as sex workersand men who have sex with men. Between 2004 and the end of 2008 the Global Fund, thelargest donor globally for harm reduction programmes, had invested US $920 million infunding to support HIV programmes that include harm reduction components. Of this $920million, around $180 million was specifically for harm reduction activities (Atun andKazatchkine, 2010). In many countries of eastern Europe, the Global Fund is the sole funderof harm reduction programmes. In Ukraine, a Global Fund grant enabled the scale-up of apilot buprenorphine substitution programme (Matic et al., 2008).Whilst the much-needed expansion in international funding for harm reduction is a welcomedevelopment, domestic investment targeting the needs of IDUs must also be expanded toincrease access and service coverage, and to ensure sustainability. There are encouragingsigns of increased investment and good coverage levels in some central and easternEuropean countries. For example, in the Czech Republic, where harm reduction programmesare primarily government funded, a coverage level of 82 % has been reached (Atun, 2006),while Estonia has agreed to continue funding through domestic activities that were initiatedwith Global Fund investments (Matic et al., 2008).
Involvement of the civil societyEvidence points to a critically important role played by civil society and grassrootsorganisations in the establishment of harm reduction activities (Sharma et al., 2008). Inwestern Europe, early in the epidemic, the engagement of civil society positively influencedthe national policies on HIV control and enabled the development of a multisectoral responseto IDU-driven HIV epidemics. A multisectoral response, which was instrumental in the control97
Harm reduction: evidence, impacts and challenges
of the HIV epidemic, also resulted in the design of community-driven user-friendly services(Atun et al., 2008). In France, non-governmental organisations (NGOs) played a central rolein persuading the government to develop policies that enabled the establishment of harmreduction programmes for IDUs (Emmanuelli and Desenclos, 2005). In contrast, when theIDU-driven epidemics began in eastern Europe few NGOs were working there, particularlyin the field of drug-use, and those that were had little or no government support (Sarang etal., 2007). In these countries a lack of civil society involvement in the response has severelyhandicapped efforts aimed at scaling up prevention and harm reduction services to reachhigh-risk populations (Atun et al., 2008). In spite of a lack of political support, networksadvocating for harm reduction, such as the Open Society Institute and the Eurasian HarmReduction Network, have played an instrumental role in advocacy, raising awareness aboutthe problems faced by injecting drug users and disseminating and developing vitalinformation to key stakeholders (Sarang et al., 2007). And in recent years, the World HealthOrganization Regional Office for Europe has appointed both a harm reduction adviser anda communicable diseases advocacy and community relations adviser, two positions unique inWHO and which have facilitated UN work on these issues across Europe.
ConclusionThe evidence shows a variable and generally weak response to IDU-driven HIV epidemics ineastern Europe. This contrasts with the successful responses mounted in western Europeancountries. While the evidence for a positive impact of harm reduction programmes incontrolling IDU-driven HIV epidemics is strong, in Europe the introduction and scaling up ofharm reduction programmes has been driven less by the evidence and more by the socio-cultural and political context prevailing in different countries. Evidence from published studiesclearly demonstrates that success in the scaling up of harm reduction activities is shaped bypolitical leadership, the legal environment, health system organisation, the availability ofdomestic financing and the engagement of civil society.Countries in western Europe that have implemented integrated, multisectoral and multi-component interventions, supported by legal and social policies, have succeeded incontrolling IDU-driven HIV epidemics. By contrast, in much of eastern Europe a lack ofenabling socio-cultural and political environment and weak civil society has hindered thedevelopment of policies to translate evidence into action, in spite of the obvious need torapidly scale-up harm reduction programmes to curb the HIV epidemic amongst IDUs.In eastern Europe, as well as Central Asia, evidence alone is not enough to influence thedevelopment of policies that will enable the scaling up of comprehensive harm reductionprogrammes. Translating evidence into action will depend not on the strength of the evidenceon the effectiveness of harm reduction but on addressing many of the complex factors thatinteract to create a receptive or, in the case of some eastern European countries, a hostilecontext for its adoption.In eastern European countries successful scaling up and effective service coverage willdepend on strong political leadership, a reform of the legal and regulatory norms to create98
Chapter 4: Perspectives on harm reduction — what experts have to say
a more enabling environment and respect the human rights of IDUs, sustained domesticfunding, the strengthening of civil society and their robust engagement in advocacy andservice provision, the planning and delivery of harm reduction programmes, as well as theorganisation of vertically structured health systems to create client-centred services. Mostcritically, in eastern Europe, harm reduction interventions must be rooted in anunderstanding of the social and economic factors that lead to the initiation of drug use andthat increase drug users’ vulnerability. This, in turn, demands the greater engagement ofdrug users in programme design to provide insights on how best to address and serve theirneeds. But first, this marginalised group must be given the opportunity to enjoy humanrights — like any other citizen. However, in many European settings we are far fromachieving this objective.
ReferencesAtun, R. A. (2006), ‘How European health systems have reacted to HIV/AIDS epidemic’, in Matic, S., Lazarus, J.V. and Donoghoe, M. C. (eds),HIV/AIDS in Europe: moving from death sentence to chronic disease management,World Health Organization Regional Office for Europe, Denmark.Atun, R. A. (2008), ‘Scaling up of harm reduction programs: the Global Fund Experience’, presented at theInternational Harm Reduction Association’s 20th International Conference,Harm Reduction and Human Rights,20–23 April, Bangkok, Thailand.Atun, R. and Kazatchkine, M. (2010), ‘The Global Fund’s leadership on harm reduction: 2002–09’,InternationalJournal of Drug Policy(in press).Atun, R. A., McKee, M., Coker, R. and Gurol-Urganci, I. (2008), ‘Health systems’ responses to 25 years of HIV inEurope: inequities persist and challenges remain’,Health Policy86, pp. 181–94.Ball, A. L. (2007), ‘HIV, injecting drug use and harm reduction: a public health response’,Addiction102, pp.684–90.Ball, A. L., Rana, S. and Dehne, K. L. (1998), ‘HIV prevention among injecting drug users: responses indeveloping and transitional countries’,Public Health Reports113 (S1), pp. 170–81.Bobrova, N., Sarang, A., Stuikyte, R. and Lezhentsev, K. (2007), ‘Obstacles in provision of anti-retroviraltreatment to drug users in Central and Eastern Europe and Central Asia: a regional overview’,InternationalJournal of Drug Policy18, pp. 313–18.Bruce, D. R., Dvoryak, S., Sylla, L. and Altice, F. L. (2006), ‘HIV treatment access and scale-up for delivery ofopiate substitution therapy with buprenorphine for IDUs in Ukraine: program description and policy implications’,International Journal of Drug Policy18, pp. 326–8.Dehne, K. L., Pokrovskiy, V., Kobyshcha, Y. and Schwartlander, B. (2000), ‘Update on the epidemics of HIV andother sexually transmitted infections in the newly independent states of the former Soviet Union’,AIDS,14 (S3),pp. S75–S84.Donoghoe, M. C. (2006), ‘Injecting drug use, harm reduction and HIV/AIDS’, in Matic, S., Lazarus, J. V. andDonoghoe, M. C. (eds),HIV/AIDS in Europe: moving from death sentence to chronic disease management,WorldHealth Organization Europe, Denmark.
99
Harm reduction: evidence, impacts and challenges
Donoghoe, M. C., Bollerup, A. R., Lazarus, J. V., Nielsen, S. and Matic, S. (2007), ‘Access to highly activeantiretroviral therapy for injecting drug users in the European region 2002–2004’,International Journal of DrugPolicy18, pp. 271−80.Emmanuelli, J. and Desenclos, J. C. (2005), ‘Harm reduction interventions, behaviors and associated healthoutcomes in France, 1996–2003’,Addiction100, pp. 1690–700.Institute of Medicine (2007),Preventing HIV infection among injecting drug users in high-risk countries: an assessmentof the evidence,National Academy of Sciences, Washington, DC.Matic, S., Lazarus, J. V., Nielsen, S. and Laukamm-Josten, U. (eds) (2008),Progress on implementing the DublinDeclaration on partnership to fight HIV/AIDS in Europe and Central Asia,World Health Organization Europe,Denmark.Rhodes, T. (2002), ‘The “risk environment”: a framework for understanding and reducing drug-related harm’,International Journal of Drug Policy13, pp. 85–94.Rhodes, T. and Simic, M. (2005), ‘Transition and HIV risk environment’,BMJ331, pp. 220–3.Rhodes, T., Ball, A., Stimson, G. V., et al. (1999), ‘HIV infection associated with drug injecting in the NewlyIndependent States, eastern Europe: the social and economic context of epidemics’,Addiction94 (9), pp. 1323–36.Rhodes, T., Sarang, A., Bobrik, A., Bobkov, E. and Platt, L. (2004), ‘HIV transmission and HIV preventionassociated with injecting drug use in the Russian Federation’,International Journal of Drug Policy15, pp. 1–16.Sarang, A., Stuikyte, R. and Bykov, R. (2007) ‘Implementation of harm reduction in Central and Eastern Europeand Central Asia’,International Journal of Drug Policy18, pp. 129–35.Sarang, A., Rhodes, T. and Platt, L. (2008), ‘Access to syringes in three Russian cities: implications for syringedistribution and coverage’,International Journal of Drug Policy19S, pp. S25–S36.Schumacher, J. E., Fischer, G. and Qian, H. Z. (2007), ‘Policy drives harm reduction for drug abuse and HIV/AIDS prevention in some developing countries’,Drug and Alcohol Dependence91, pp. 300–05.Sharma, M., Burrows, D. and Bluthenthal, R. N. (2008), ‘Improving coverage and scale-up of HIV prevention,treatment and care for injecting drug users: moving the agenda forward’,International Journal of Drug Policy19S,pp. S1–S4.Stimson, G. V. (1995), ‘AIDS and injecting drug use in the United Kingdom, 1987–1993: the policy response andthe prevention of the epidemic’,Social Sciences & Medicine41 (5), pp. 669–716.Tkatchenko-Schmidt, E., Renton, A., Gevorgyan, R., Davydenko, L. and Atun, R. A. (2007), ‘Prevention of HIV/AIDS among injecting drug users in Russia: opportunities and barriers to scaling-up of harm reductionprogrammes’,Health Policy85, pp. 162–71.UNAIDS (Joint United Nations Programme on HIV/AIDS) and WHO (World Health Organization) (2008),2008report on the global AIDS epidemic,UNAIDS, WHO, Geneva. Available at http://data.unaids.org/pub/GlobalReport/2008/jc1510_2008_global_report_pp29_62_en.pdf.Wiessing, L., van de Laar, M. J., Donoghoe, M. C., et al. (2008), ‘HIV among injecting drug users in Europe:increasing trends in the East’,Eurosurveillance13 (50), pp. 1–3.Wiessing, L., Likatavicius, G., Klempova, D., et al. (2009), ‘Associations between availability and coverage ofHIV-prevention measures and subsequent incidence of diagnosed HIV infection among injection drug users’,American Journal of Public Health99 (6), pp. 1049–52.
100
Chapter 4: Perspectives on harm reduction — what experts have to say
People who use drugs and their role in harm reductionMat SouthwellDrug taking is in part about an engagement with risk and it is therefore unsurprising to findthat people who use drugs tend to be ‘risk takers’ (Measham et al., 2001). People come todrug taking with an understanding that drug use involves risk, and that this may be attractivein and of itself. Most people who use drugs engage in drug use with an understanding thatthey are managing the interplay between the positive effects of a drug (pleasuremaximisation) and the risks associated with administering or taking a drug (harm reduction).As such, people who use drugs can be defined as calculated risk takers. This challenges theorthodox addiction archetypes that describe people who use drugs as victims either ofsubstances with some type of pseudo-magical quality or of the ‘evil drug dealers’ who peddlethese drugs (Booth, 1997). Those of us who choose and defend the right to take mind-alteringsubstances are not denying or minimising the actual risks involved in taking drugs. However,risk does not automatically result in harm and the factors informing harm are complex,multifaceted, and influenced by both internal and external factors. Too often drug policiesseek simple and universal solutions to the complex world of drug taking. This results in amismatch between political and policy discourses and the reality of drug taking on theground, which serves to distance people who use drugs, resulting in a general distrust ofofficial guidance.It is important to understand that the term ‘risk’ normally defines the likelihood of specificeventualities, which may have either beneficial or adverse consequences. For the personusing drugs, the risk or potential of pleasure maximisation is judged against the risk thatharm may arise from drug taking. This assessment of comparative risk is best undertaken in avalue-free context, which allows people to make hopefully informed decisions about whetherto use drugs or not, and, for some, to make informed decisions about which drugs to use, bywhich routes and in what amounts.Such a value-free environment may be desirable but it clearly does not exist. Drugsprevention measures are driven by a moralistic opposition to intoxication, which has its rootsin the temperance movement. Drug prevention sets out to persuade young people inparticular not to take drugs, by ignoring the pleasure features of these drugs and by playingup risks.
Learning to live with drugsIn fact, anti-drugs campaigns are arguably primarily about a discourse between politiciansand adult voters, designed to show that a particular political party is ‘tough on crime’. Thisabuse of drugs prevention is unethical and can have dangerous, if unintended,consequences. Drugs prevention is usually pharmacocentric, focusing on drug-related risks inisolation from an understanding of youth culture or the individual lives of young people.Historically, drug use has been part of an ‘outsider’ identity and some come to drug use in101
Harm reduction: evidence, impacts and challenges
search of belonging and community (Fleming, 2001). The United Kingdom Government’santi-heroin campaign of the 1980s, ‘Heroin screws you up’ (http://drugtrain.net/drugs/heroin/heroin_screws_you_up.html), was shown in post-campaign testing to have attractedyoung people to adopt heroin use, as they identified with the alienated and isolated youngpeople portrayed in the campaign’s gritty black and white posters (Hastings et al., 2004).When this information entered the public domain, government responded by condemningthe researcher and excluding him from undertaking further official research. This hardlyreflects a commitment to science but effectively illustrates the value-laden nature of this field.The harm reduction movement has been ambivalent about its engagement with drugsprevention, fearing that opposition might lead to further accusations of being ‘pro-drugs’.However, the harm reduction movement needs to lobby for value-free drugs education thatprovides young people with objective information about different drugs, their effects and riskprofiles. If governments are serious about reducing young people’s engagement in drugtaking and, particularly, in harmful drug use, then it is likely that addressing young people’smotivation, education, and social circumstances will have a greater impact than pushingsimplistic anti-drugs messages.The need for harm reduction is becoming ever more pressing as young people gain access to adiverse range of drugs. Significantly, these drugs are increasingly taken outside the cultural andsocial settings that often hold community knowledge and learning. In archaic societies, Shamansacted as the guardians of the oral history of a community, gathering and disseminating learningbetween groups and generations. The demonisation of drugs, and the people who take them,creates a huge disincentive for peer leaders to stand up and model this function within modern-day communities. As such, young people often operate as if they are the first group ever to takedrugs (Jay, 2000). This maximises risk by forcing new generations to engage in drug takingwithout the benefit of the knowledge and learning of previous generations.
User involvement in harm reductionHarm reduction is most comfortably and effectively delivered with people who have chosento have a sustained relationship with drug taking. However, even in this setting there aretensions about the role and contribution of people who use drugs. It is important to recognisethat while many harm reduction services are delivered by professionals, much harmreduction innovation emerges from within drug using communities. Let us not forget that adrug user group established the world’s first needle exchange back in 1984 (Buning et al.,1990; Stimson, 2007), in response to hepatitis B.This structural response follows the natural desire to avoid risk where possible while in searchof pleasure maximisation. Friedman identified that people who injected drugs in New Yorkresponded to seeing their peers falling sick in the 1980s, with what was later identified asHIV/AIDS, by reducing needle sharing and this led to a leveling off of infection rates(Friedman et al., 1999). Needle exchange subsequently provided injectors with thetechnology to act on this organic learning, leading to actual reductions in infection rates.102
Chapter 4: Perspectives on harm reduction — what experts have to say
This process of organic harm reduction has been seen among a number of drug usingpopulations. For example, people who smoke crack correctly sought to exclude the cause of‘black lung’, cigarette ash and other impurities, by constructing or sourcing ash-free glasspipes while continuing to smoke crack. While such strategies have been known about sincethe mid-1990s, stimulant pipe distribution schemes have not been widely adopted. Thereneeds to be greater investment in the interface between drug using communities and theprofessional field. Drug user organisations should be key players in this environment. It isnoteworthy that innovation around crack harm reduction has largely come from drug usergroups or practitioners with experiential, as well as professional, expertise. Partnershipsbetween academics, practitioners and drug user organisations need to be strengthened toensure that knowledge in all three domains is considered and where appropriate translatedinto accessible practice or peer support interventions.Spontaneous trends away from injecting, towards non-injecting routes of administration, havebeen identified in a number of European settings and in New York. Research would indicatethat such switches in route of administration reflect a commitment to health, a desire toreduce levels of dependency, or a wish to increase self-control. However, these changes havealso been shown to be significantly influenced by the type, cost and quality of drugs. Assuch, route transition changes are only likely to occur when reasonably priced, good qualitydrugs are available in a suitable form. Strang and colleagues have questioned whether sometype of market manipulation might be helpful in supporting such trends (Hunt et al., 1999).However, in reality this conflicts with demand reduction thinking that sees the disruption ofthe drug supply chain as a positive objective.Finally, people who use drugs and their organisations can uniquely operate as ‘consumeradvocates’ within illicit drug scenes. These models are still underdeveloped and have yet tobe subjected to scientific scrutiny. However, strategies for promoting consumer rights andethical trading standards offer another positive opportunity for influencing the context withinwhich drug taking takes place. Some suppliers of drugs have shown themselves willing tosupport harm reduction messages, operating as secondary needle exchange providers andacting as conduits for health education messages to be transmitted to key populations ofdrugs users (Southwell, 2008).People who use drugs need to become routine partners in harm reduction, supporting theidentification, development and promotion of harm reduction strategies. Resources need tobe allocated to properly support the translation and dissemination of peer and academiclearning into practice and peer support interventions.
ReferencesBooth, J. B. (1997),The myth of addiction(2nd edition), Harwood Academic Publishers, Newark.Buning, E. C., van Brussel G. H. and van Santen, G. (1990), ‘The “methadone by bus” project in Amsterdam’,British Journal of Addiction85, pp. 1247–50.Fleming, P. (2001),The role of treatment services in motivating and deterring treatment entry: exploring the views ofopioid-dependent drug users,Wells Healthcare Communications Ltd, England.
103
Harm reduction: evidence, impacts and challenges
Friedman, S. R., Curtis, R., Neaguis, A., Jose, B. and Des Jarlais, D. D. (1999),Social networks, drug injectors’ livesand HIV/AIDS,Kluwer Academy, New York.Hastings, G., Stead, M. and Webb, J. (2004), ‘Fear appeals in social marketing: strategic and ethical reasons forconcern’,Psychology and Marketing21, pp. 961–86.Hunt, N., Griffiths, P., Southwell, M., Stillwell, G. and Strang, J. (1999), ‘Preventing and curtailing injecting druguse: opportunities for developing and delivering “route transition interventions’’,Drug and Alcohol Review18, pp.441–51.Jay, M. (2000),Emperors of dreams: drugs in the nineteenth century,Dedalus, Cambridge.Measham, F., Aldridge, J. and Parker, H. (2001),Dancing on drugs: risk, health, and hedonism in the British clubscene,Free Association Books, London.Southwell, M. (2008), ‘Consumer action and drug supply networks’, unpublished report. Available at http://tinyurl.com/consumeractiondealers.Stimson, G. V. (2007), ‘Harm reduction — coming of age: a local movement with global impact’,InternationalJournal of Drug Policy18, pp. 67–9.
Harm reduction — an ‘ethical’ perspectiveCraig FryIn its short history, the harm reduction specialty field of public health has routinely pushed theboundaries of evidence and policy, and tested our moral imagination in relation to the placeof drug use and users in society and possible community responses. Each new harmreduction policy and programme proposal has been met with intense and often ongoingpublic scrutiny (e.g. condom distribution, needle and syringe programmes, maintenance andsubstitution pharmacotherapy, heroin prescription, supervised injecting).The unwavering response to this scrutiny from within the harm reduction movement has beento argue that its ‘pragmatic’ drug policies and interventions are justified because theavailable evidence shows they work to reduce drug harms (Hunt et al., 2006; Ritter andCameron, 2006). The reduction of harms associated with the use and misuse of psychoactivesubstances would appear to be a straightforward goal, and one on which there ought to bewidespread agreement. Harm reduction in the most general sense can be considered anethical project if we accept that harm reduction measures assist in alleviating drug-relatedharm. Less drug harm is a good thing.But there is more. Harm reduction has only recently started to grapple critically with thedefinitional challenges and uncertainties inherent in its core goal (for example, what is drugharm? How can drug harms be measured? How do we balance drug harms and benefits?).Likewise, this field is only now beginning to awaken to the difficult normative questions thatcome with a focus on drug use harm (for example, what should we do to address drugharms? Whose drug harms matter most? Are some types of drug harm acceptable?).104
Chapter 4: Perspectives on harm reduction — what experts have to say
Harm reduction, at least mainstream harm reduction, has for the most part argued that thebest way to address the definitional, measurement and evaluative challenges it faces isthrough evidence-based scientific approaches. Here, ‘facts’ are separated from ‘values’ in thequest for universally valid (and therefore compelling) and value-neutral or ‘objective’ scientificfacts that are untainted by ‘subjective’ moral evaluations (Weatherburn, 2009).As this monograph shows, the evidence base in support of harm reduction policies,programmes and interventions has grown in size, complexity and sophistication. Indeed, sosuccessful has harm reduction been judged by its advocates that we are starting to see claimsemerge that the scientific debate about the value or positive impact of harm reduction is nowover (Wodak, 2007). Harm reduction works.However, there is still significant government opposition to harm reduction measures in someof the world’s most populous countries that arguably need such measures the most. Thisopposition has been mostly attributed to the moralising by some powerful interests in societyabout the permissibility of drug misuse and of policy responses that are not abstinence-based. However, the debate has also increasingly been about the authority of science andscientific knowledge as the primary arbiter of what may be regarded as acceptable socialpolicy. Indeed, in the health and drug policy arena we are finally coming to accept theexistence of ‘blurred boundaries’ between science and politics (Gottweis, 2008), and theirimplications for both the definition of and proposed responses to ‘health problems’.Diverse perspectives exist on drug policy issues and these are informed, for better or worse,by a variety of value and belief systems. ‘Evidence’ has a social character in terms of theunderlying values and beliefs that influence how it is defined, collected, reported and used.Harm reduction today must accommodate uncertainty and diverse values.When there are disputes and uncertainty about the ‘facts’ in harm reduction, ‘values’ cannotbe separated from the equation, precisely because value positions are the reason disputesand uncertainty exist in the first place. In the broader context of science and public policycritique there is a growing recognition that disputes on what constitutes ‘good evidence’ cancompromise communication among scientists, policymakers and the public, and in turnconstrain the types of public policy questions that are addressed (Kinzig et al., 2003).We may well ask, then, whether the continued emphasis on evidence-based over values-based approaches is consistent with the ‘pragmatism’ that has so often been attributed as aharm reduction hallmark. It has been suggested that harm reduction’s silence on moral andvalue issues (in favour of scientific argument) undermines the movement’s ability to engagecritics who would claim that abstinence and law enforcement are the only morally acceptablesolutions to drug problems (Hathaway and Tousaw, 2008).The time has come for harm reduction to establish its ethical credentials (Irwin and Fry,2007). I use ‘ethical’ and ‘ethics’ here to refer to a critical orientation towards values andnormative considerations, and less so to moral philosophy or any particular ethical theory orframework. For me the question ‘Is harm reduction ethical?’ is first and foremost a query105
Harm reduction: evidence, impacts and challenges
about whether or not harm reduction is, or perhaps can be, reflexive or ‘in touch’ with thediverse value perspectives underpinning it.In the last few years there has been increasing attention to the task of articulating the moralunderpinnings of harm reduction. It has been discussed in relation to communitarian ethics(Fry et al., 2005), virtue ethics (Christie et al., 2008), deontology and utilitarianism and more(Kleinig and Einstein, 2006; Kleinig, 2008). Special theme issues in leading journals haveappeared on harm reduction ethics (Fry et al., 2008), scholarly monographs (Kleinig andEinstein, 2006) and empirical research on this theme is also emerging (Solai et al., 2006;Phillips and Bourne, 2008).What is particularly encouraging is that a range of perspectives, both theoretical andapplied, are emerging on harm reduction ethics. Contributions are coming from moralphilosophy, public health, nursing, anthropology, sociology, human rights and so on. Theseprovide rich and varied sources to draw from, and help to highlight an appropriatelypluralistic ‘harm reduction ethics’. Values-based approaches such as these are starting to gainrecognition as an additional resource that can be employed to guide and evaluate harmreduction initiatives.Harm reduction as defined in this monograph is a sophisticated evidence-based approach todrug policy, programmes and interventions. For a long time now in harm reduction the goalhas been to strive for agreement around what the scientific evidence shows is the impact ofharm reduction initiatives. Despite significant achievements in this area, tensions anduncertainties remain about the authority of scientific knowledge here.Diverse value perspectives exist in the harm reduction domain, and we might rightly ask whatelse could harm reduction do in addition to devising ever-more sophisticated models andcollecting more precise data? Evidence-based harm reduction has rendered harm reduction/drug policymaking no less a political project.An appropriate new focus for the future may be to ask, ‘What should be the relative placesof evidence and ethics in harm reduction/drug policy decision-making?’ Considering such aquestion would require us to adopt the perspective of ‘interested participants’ rather than‘detached observers’. In doing so we would need to also accept that science alone isinsufficient for making the case for harm reduction and achieving a wider consensus on thefull range of normative criteria for action in this area.For example, beyond the usual utilitarian ‘cost–benefit’ analyses, we might also strive toclarify what competing interests exist in harm reduction (e.g. in the case of funding sourcesand regulation from different industries) and how these may be reconciled. We might alsoconsider, what are the obligations and responsibilities of harm reduction professionals? Whatare the justifications (if any) for prioritising the desires and preferences of individuals over theinterests of wider groups and collectivities?‘Ethics engagement’ in harm reduction does not commit us to a punitive moral stance ondrug use or users; rather, it can help to evaluate these perspectives directly (Fry et al., 2005).
106
Chapter 4: Perspectives on harm reduction — what experts have to say
One practical form this could take is the development of a harm reduction code of ethics as away to orientate practitioners, researchers, policymakers and the community towardsconsidering core values in harm reduction work. A harm reduction code of ethics could assistpractitioners in balancing diverse value sets and ethical perspectives in relation to the ethicalchallenges encountered. It could also serve to facilitate debate on topical ethical dilemmas,and the development of applied ethics resources to enhance harm reduction practice (forexample, guidelines, professional development, etc).We are entering a new phase in public health where the central place of values and ethicalconsiderations is gaining greater acknowledgment. A commitment to making harmreduction values explicit requires that we consider ‘ethics’ as a tool to enhance, rather thanrestrict, harm reduction practice (in the same way we think of scientific, empirical, clinicaland other practice tools). The future focus of harm reduction advocates will be to worktowards enhancing intervention coverage and intensity. Evidence-based approaches will ofcourse continue to guide these developments. The harm reduction field could also benefitfrom applying values-based approaches in order to establish once and for all its ethicalcredentials.
AcknowledgementsCraig Fry is supported by an NHMRC Australian Public Health Training Fellowship #519556,the Murdoch Childrens Research Institute (Children’s Bioethics Center), and the University ofMelbourne (Centre for Applied Philosophy and Public Ethics).
ReferencesChristie, T. K., Groarke, L. and Sweet, W. (2008), ‘Virtue ethics as an alternative to deontological andconsequential reasoning in the harm reduction debate’,International Journal of Drug Policy19, pp. 52–8.Fry, C., Treloar, C. and Maher, L. (2005), ‘Ethical challenges and responses in harm reduction research:promoting applied communitarian ethics’,Drug and Alcohol Review24, pp. 449–59.Fry, C. L., Khoshnood, K., Power, R. and Sharma, M. (2008), ‘Harm reduction ethics: acknowledging the valuesand beliefs behind our actions’,International Journal of Drug Policy19, pp. 1–3.Gottweis, H. (2008), ‘Participation and the new governance of life’,BioSocieties3, pp. 265–86.Hathaway, A. D. and Tousaw, K. I. (2008), ‘Harm reduction headway and continuing resistance: insights fromsafe injection in the city of Vancouver’,International Journal of Drug Policy19, pp. 11–16.Hunt, N., Trace, M. and Bewley-Taylor, D. (2006),Reducing drug related harms to health: an overview of the globalevidence,Report 4, Beckley Foundation Drug Policy Programme, United Kingdom.Irwin, K. and Fry, C. L. (2007), ‘Strengthening drug policy and practice through ethics engagement: an oldchallenge for a new harm reduction’,International Journal of Drug Policy18, pp. 75–83.Kinzig, A., Starrett, D., Arrow, K., et al. (2003), ‘Coping with uncertainty: a call for a new science–policy forum’,Ambio32, pp. 330–5.
107
Harm reduction: evidence, impacts and challenges
Kleinig, J. (2008), ‘The ethics of harm reduction’,Substance Use and Misuse43, pp. 1–16.Kleinig, J. and Einstein, S. (eds) (2006),Ethical challenges for intervening in drug use: policy, research and treatmentissues,Sam Houston State University, Huntsville.Phillips, R. E. and Bourne, H. (2008), ‘The impact of worker values on client outcomes within a drug treatmentservice’,International Journal of Drug Policy19, pp. 33–41.Ritter, A. and Cameron, J. (2006). ‘A review of the efficacy and effectiveness of harm reduction strategies foralcohol, tobacco and illicit drugs’,Drug and Alcohol Review25 (6), pp. 611–24.Solai, S., Dubois-Arber, F., Benninghoff, F. and Benaroyo, L. (2006), ‘Ethical reflections emerging during theactivity of a low threshold facility with supervised drug consumption room in Geneva, Switzerland’,InternationalJournal of Drug Policy17, pp. 17–22.Weatherburn, D. (2009), ‘Dilemmas in harm minimization’,Addiction104, pp. 335–9.Wodak, A. (2007), ‘Ethics and drug policy’,Psychiatry6, pp. 59–62.
The ambiguity of harm reduction — goal or means, and whatconstitutes harm?Robin RoomHarm reduction, or harm minimisation, is at the heart of classic approaches to public health,so it is no surprise that the modern use of the terms with reference to illegal drugs has beenanticipated in other fields. For instance, in 1970 the sociologist Kettil Bruun wrote a policypiece in Finnish entitled, ‘The minimisation of alcohol damage’ (Bruun, 1970), and the sameformulation and way of thinking was soon picked up in English language discussions (e.g.Room, 1975).As applied initially in the alcohol field, the focus of the terms was clearly on the intendedoutcome of the action. The terms identified an overall goal, without specifying the means ofachieving it, which could be diverse, including market controls that reduce levels ofconsumption and interventions to make the drinking environment safer. In the context of the1970s, the implicit contrast of a ‘harm minimisation’ approach was not with abstinence as auniversal goal, but with an ‘alcoholism’ approach, which tended to channel all interventionsthrough the gate of clinical care and cure of alcoholism (Room, 1984).In the alcohol field, ‘harm minimisation’ was later reinvented as a term imported from thedrugs field (e.g. Plant et al., 1997), and with a correspondingly narrower focus on contextualmeans of reducing harm from heavy use. There are certainly earlier examples of such classic‘harm reduction’ approaches in the alcohol field (e.g. Dumont, 1967; Drew, 1980), but therehad been no explicit general framing for them.In the drug field, the meaning in terms of a focus on goals has also been implicit since ‘harmreduction’ emerged as a term and indeed as a social and professional movement in the1980s. But the dominant meaning of the term has focused not on goals but on means: harm108
Chapter 4: Perspectives on harm reduction — what experts have to say
reduction, in the context of the AIDS epidemic, was primarily applied to strategies thatreduced the risk for heavy injection drug users, by such means as offering a switch to an oralopiate, offering sterile needles, or offering a safe place to inject. The discussion of ‘what isharm reduction?’ currently on the International Harm Reduction Association’s website startsfrom a definition in terms of approaches that ‘aim to reduce the … harms’. But then itimplicitly contrasts harm reduction with ‘approaches that aim for reductions in …consumption’. However, there is still ambiguity about whether reducing consumption can be aharm reduction goal; the IHRA discussion goes on to backtrack slightly, contrasting anapproach requiring abstinence with a harm reduction approach involving ‘more pragmaticchoices such as limiting … intake’ (IHRA, 2009).For many in the drugs harm reduction movement, the term also includes an ethicalcomponent, and should be defined in such a way that punitive abstinence-orientedapproaches, even if reducing harm was their goal, would be contrasted to harm reductionrather than included in the term (CCSA, 1996). The IHRA website discussion expresses this interms of a second ‘pillar’ of harm reduction, a ‘human rights approach’ alongside the‘pragmatic public health approach’.A specific adaptation in the context of Australian politics has been the differentiation of‘harm minimisation’ from ‘harm reduction’. In the era of a national government that rejectedsafe injection sites as a strategy, and tended to reject ‘harm reduction’ as an overall policy, acompromise formulation was reached that drug policies aimed at ‘harm minimisation’ as agoal, with abstinence-based strategies included as one set of strategies fitting within harmminimisation (Blewett, 2004).The distinction between ‘harm minimisation’ and ‘harm reduction’ served the political needsof a particular time in Australia, but it invites confusion, so that even researchers focused onpolitical rhetoric may miss the distinction (e.g. Bessant, 2008). In general, the meaning of theterms remains somewhat ambiguous, with some wavering over time. Thus in 2004 the‘definitive interpretation’ of ‘harm reduction’ on the website of the International HarmReduction Association explicitly included an abstinence strategy as a ‘special subset of harmreduction’ (Room, 2004); now, as we have noted, the discussion of the term on the samewebsite contrasts harm reduction with aiming to reduce consumption. The issue of whetherharm reduction refers to goals or to means remains unsettled.Another issue that is of increasing importance in the context of ideas of harm reduction iswhat counts as harm. The usual procedure in economic studies of the social costs of drug useis to count up all public expenditures and many private costs that are considered to beattributable to drug use (e.g. Collins and Lapsley, 2008). These costs include many that wouldnot occur if the drug use remained at the same level but the societal response to it changed— for instance, if possession and use are decriminalised. The argument has been putforward for some time that an effort should be made to ‘separately take into account theresources expended in social responses to drug use and its control, and the subsidiary harmscaused by those responses’ (Fischer et al., 1997). As attention increases to measuringspecifically the harms from illicit drug use (Melberg, 2009), rather than just the fact of thedrug use itself, this issue of separating out the harms arising from the societal response (easy109
Harm reduction: evidence, impacts and challenges
in principle, not so easy in practice) will take on greater salience. Reducing the two kinds ofharm can point policy in very different directions. If the harm arises from heavy use per se,reducing or eliminating use or changing the mode of use are the logical first choices forreducing the harm. But if the harm results from the criminalisation per se, decriminalising is alogical way of reducing the harm.Few would argue against the proposition that harm reduction or harm minimisation as a goalwill have a continuing importance in drug policy. In this context, it is time to get serious aboutdefining what constitutes harm, and to what it can be attributed — whether to the drug useitself and consequent events and behaviours, or to the social and societal reactions to thedrug use. Harm reduction as a set of strategies in reducing the problems of heavy drug usewill have a continuing place in the overall set of strategies for managing drug use andreducing drug problems. But, as the passions of the era of the ‘war on drugs’ fade, they arelikely to be fitted into place as a routine part of the treatment and other social handling ofheavy drug use.
ReferencesBessant, J. (2008), ‘From “harm minimization” to “zero tolerance” drugs policy in Australia: how the Howardgovernment changed its mind’,Policy Studies29 (2), pp. 197–214.Blewett, N. (2004), ‘Harm minimization and Australia’s national drug strategies’, presented at the 15thInternational Conference on the Reduction of Drug Related Harm, Melbourne, Australia, 20–24 April.Bruun, K. (1970), ‘Alkoholihaitat mahdollisimman vähäisiksi’ (The minimisation of alcohol damage),Alkoholipolitiikka35, pp. 185–91. Abstracted inDrinking and Drug Practices Surveyor8 (15), p. 47 (1973).CCSA National Working Group on Policy (1996),Harm reduction: concepts and practices — a policy discussionpaper,Canadian Centre on Substance Abuse, Ottawa. Also published as a paper by D. Riley et al. inSubstanceUse and Misuse34, pp. 9–24 (1999).Collins, D. J. and Lapsley, H. M. (2008),The costs of tobacco, alcohol and illicit drug abuse to Australian society in2004/05,National Drug Strategy Monograph Series No. 64, Canberra. Available at http://www.health.gov.au/internet/drugstrategy/publishing.nsf/Content/mono64.Drew, L. R. H. (1980), ‘Prevention of alcohol-related brain damage’,Medical Journal of Australia672, p. 48.Dumont, M. P. (1967), ‘Tavern culture: the sustenance of homeless men’,American Journal of Orthopsychiatry37(5), pp. 935–45.Fischer, B., Kendall, P., Rehm, J. and Room, R. (1997), ‘Charting WHO-goals for licit and illicit drugs for the year2000: are we “on track”?’Public Health111, pp. 271–5.IHRA (2009), ‘What is harm reduction?’ International Harm Reduction Association, North Melbourne, Vic.,Australia. Available at http://www.ihra.net/Whatisharmreduction (accessed 23 May 2009).Melberg, H-O. (2009), ‘Is it possible to quantify human suffering? Results from a Nordic survey’, presented at the3rd annual meeting of the International Society for the Study of Drug Policy, Vienna, 2–3 March.Plant, M., Single, E. and Stockwell, T. (eds) (1997),Alcohol: minimizing the harm — what works?Free AssociationBooks, London.
110
Chapter 4: Perspectives on harm reduction — what experts have to say
Room, R. (1975), ‘Minimizing alcohol problems’, in Chafetz, M. (ed.),Proceedings of the fourth annual alcoholismconference of the National Institute on Alcohol Abuse and Alcoholism: research, treatment and prevention,DHEWPublication No. (ADM)76-284, US Government Printing Office, Washington, DC, pp. 379–93.Room, R. (1984), ‘Alcohol control and public health’,Annual Review of Public Health5, pp. 293–317.Room, R. (2004), ‘Alcohol and harm reduction, then and now’,Critical Public Health14, pp. 329–44.
111
Evidence andimpacts
PARTII
Chapter 5Harm reduction among injecting drug users — evidence ofeffectivenessJo Kimber, Norah Palmateer, Sharon Hutchinson, Matthew Hickman, David Goldberg andTim Rhodes
AbstractThis chapter synthesises and evaluates the available direct evidence relating to the impact ofneedle and syringe programmes (NSPs), opioid substitution treatment (OST), drugconsumption rooms (DCRs), and peer naloxone distribution (PND) on HIV/hepatitis C (HCV)incidence/prevalence, injecting risk behaviour and overdose-related mortality. To achievethis, we conducted a review of reviews; a systematic and explicit method used to identify,select and critically appraise relevant findings from secondary level research (systematicreviews and/or meta-analyses) into an evidence briefing. In the absence of high-qualityreviews, appraisal of the evidence was supplemented with a targeted review of the primaryliterature. We find that there is sufficient review-level evidence that OST reduces HIVtransmission, while the evidence in support of NSPs reducing HIV transmission is moretentative, and for DCRs currently insufficient. There is tentative evidence that OST has limitedeffectiveness in reducing HCV transmission, and insufficient evidence to support or discountNSPs or DCRs’ ability to reduce HCV transmission. There is sufficient review-level evidencethat NSPs, OST and DCRs reduce self-reported injecting risk behaviour. There is sufficientreview evidence that OST reduces risk of overdose mortality, but insufficient evidence tosupport or discount the effect of DCRs or PND on overdose deaths at the community level.Our review shows evidence in support of a variety of harm reduction interventions buthighlights an uneven presence of high-quality review evidence. Future evaluation of harmreduction programmes should prioritise methodologically robust study designs.Keywords:injecting drug use, review methods, and needle syringe programmes, opioidsubstitution treatment, drug consumption rooms, peer naloxone distribution.
IntroductionInjecting drug use is a global and regional public health problem, with an estimated 15.9million injecting drug users (IDUs) worldwide and prevalence rates in European Union (EU)Member States ranging between 0.6 and 15.1 per 1 000 population aged 15–65 years(EMCDDA, 2009; Mathers et al., 2008). IDUs, especially opiate users, experience excessmorbidity and mortality, being approximately 10 times more likely to die compared to theirnon-IDU peers (Bargagli et al., 2006; Degenhardt et al., 2004; Degenhardt et al., 2006).The primary causes of IDU-related morbidity and mortality are blood-borne viruses(BBVs) and drug overdose (Degenhardt et al., 2006). The prevention of BBV infections and115
Harm reduction: evidence, impacts and challenges
drug overdose deaths among IDUs in community and custodial settings is a key objectiveof the EU drug strategy (European Commission, 2007). Interventions that directly targetthese harms include: needle and syringe programmes (NSPs) and opioid substitutiontreatment (OST); supervised drug consumption rooms (DCRs), and peer naloxonedistribution (PND).NSPs provide sterile needle/syringes and other injecting equipment to IDUs. Delivery isdiverse and can include ‘primary’ fixed site, mobile and/or outreach services and‘secondary’ access via community pharmacies, other health services and/or vendingmachines (WHO, 2007). NSPs operate across all EU Member States (EMCDDA, 2008; seealso Cook et al., 2010).OST is prescribed to dependent users to diminish the use and effects of illicit opiates.Treatment is most efficacious when it is continuous and given at adequate doses (Amato etal., 2005; Faggiano et al., 2003; Ward et al., 1997). Community-based OST is availableacross all EU Member States and prison-based OST is officially available in the majority ofMember States, although overall accessibility is limited (EMCDDA, 2008; see also Stevens etal., 2010). It is estimated that in 2007 more than 650 000 opioid users received OST inEurope, and the most commonly prescribed forms are methadone maintenance treatment(MMT) and buprenorphine maintenance treatment (BMT) (EMCDDA, 2008).DCRs offer a low-threshold environment to use pre-obtained drugs hygienically and to accesstargeted safer injecting advice and intervention in case of overdose (Kimber et al., 2003; seealso Hedrich et al., 2010). DCRs have been operating in Europe for more than 25 years andare available in 59 cities across Germany, Luxembourg, the Netherlands, Norway, Spainand Switzerland (EMCDDA, 2008).Peer naloxone distribution (PND) or ‘take-home naloxone’ programmes provide theantagonist drug, with training to IDUs and/or carers to improve their capacity for effectiveintervention at opioid-related overdose (Darke and Hall, 1997). Naloxone is currentlyavailable on a take-home basis in Italy (where it is widely dispensed by addiction services),Germany, Spain, Lithuania and Norway (Reitox, 2008). PND pilots have also taken place(Dettmer et al., 2001; McAuley et al., 2009; Strang et al., 2008) and are underway (NationalTreatment Agency, 2009; Parmar, 2008) in the United Kingdom.The availability and delivery of harm reduction interventions can be controversial outside ofthe public health arena and vulnerable to shifts in the political environment at the local,national and international level (Bewley-Taylor, 2002; Broadhead et al., 1999; Small, 2007).This re-enforces the need for policymakers to have access to up-to-date evidence briefings onthe targeted outcomes and effectiveness of the relevant interventions.In this chapter we synthesise and evaluate the available evidence relating to the impact ofNSPs, OST and DCRs on HIV and HCV incidence/prevalence, injecting risk behaviour, andOST, DCRs and PND on overdose-related mortality. We will focus on evidence synthesised inprevious evidence reviews, and where necessary supplement with a review of the recentlypublished primary literature.116
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
MethodsOur evaluation of the evidence is based primarily on the ‘review of reviews’, or tertiary levelresearch method (Kelly et al., 2002). This is a systematic and explicit method to identify,select, and critically appraise relevant findings from secondary level research (i.e. systematicreviews and/or meta-analyses) into an evidence briefing.We have drawn substantively on our recent review of reviews of harm reduction interventions(Palmateer et al., 2008; Palmateer et al., 2010). Our inclusion criteria were English languagesystematic reviews, syntheses, or meta-analyses that examined the effectiveness of NSPs, OSTand DCRs in relation to HIV and HCV incidence/prevalence and/or injecting risk behaviouroutcomes. For this chapter we have updated our previous review of reviews (Palmateer et al.,2008) by searching for any new reviews published between March 2007 and August 2009and by conducting additional searches for relevant English language systematic reviews,syntheses, or meta-analyses that examined the effectiveness of OST, DCRs and PND inpreventing overdose.Databases searched were: CINAHL, Cochrane Library, EMBASE, IBSS, MEDLINE, andPsycINFO. To identify grey literature and minimise English language publication bias we alsosearched publications of key international agencies for harm reduction. These included: theEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA), the National Instituteon Drug Abuse (NIDA), the United States Institute of Medicine, the United Nations Office onDrugs and Crime (UNODC), and the World Health Organization (WHO). All databaseswere searched from 1980 to March 2009 except CINAHL, which was searched from 1982 toMarch 2009. At the screening stage it was apparent that reviews from the 1980s and 1990shad been superseded by more recent reviews and we restricted our appraisal of reviewspublished from 2000 onwards.Abstracts were screened and evaluated by two reviewers to determine if the paper met theinclusion criteria. If there was disagreement regarding the relevance of an abstract the fullpaper was retrieved for further evaluation. In the event of a lack of consensus a decision wasreached by discussing points of disagreement.Selected reviews were critically appraised using a tool that considers the rigour of themethods used to identify the relevant literature, the appraisal of the primary literature, thequality of the analysis in the case of meta-analysis, and the appropriateness of theconclusions (Kelly et al., 2002; Palmateer et al., 2010).Reviews rated 1 or 2 were included as high-quality (‘core’) reviews. Reviews rated 3 wereretained as ‘supplementary’, not considered to be of sufficient quality to rely on the author’sconclusions but viewed as providing complementary information on the effectiveness of theinterventions.From each review, we extracted information on the reviewers’ assessment of the evidenceand the number, design and findings of the relevant primary studies. The level of reviewevidence that supported or discounted the effect of an intervention was classified as: (i)117
Harm reduction: evidence, impacts and challenges
sufficient; (ii) tentative; (iii) insufficient; or (iv) no evidence from reviews. These classificationsare based on a framework (Table 5.1) that considers the quality of the reviews, the reviewers’conclusions and the designs/findings of the primary studies (Ellis et al., 2003).
Table 5.1:Types of evidence statements and the level of evidence that wasrequired to support each statementEvidence statementSufficient evidence from reviews to eithersupport or discount the effectiveness of anintervention
Level of evidence• lear statement from one or more core Creviews based on multiple robust studies.Or,• onsistent evidence across multiple robust Cstudies within one or more core reviews, inthe absence of a clear and consistentstatement in the review(s).• tentative statement from one or more core Areviews based on consistent evidence from asmall number of robust studies or multipleweaker studies.Or,• onsistent evidence from a small number of Crobust studies or multiple weaker studieswithin one or more core reviews, in theabsence of a clear and consistent statementin the review(s).Or,• onflicting evidence from one or more core Creviews, with the stronger evidenceweighted towards one side (eithersupporting or discounting effectiveness) anda plausible reason for the conflict.Or,• onsistent evidence from multiple robust Cstudies within one or more supplementaryreviews, in the absence of a core review.• statement of insufficient evidence from a Acore review.Or,• nsufficient evidence to either support or Idiscount the effectiveness of an intervention(either because there is too little evidence orthe evidence is too weak), in the absence ofa clear and consistent statement of evidencefrom (a) core review(s).Or,• nything less than consistent evidence from Amultiple robust studies within one or moresupplementary reviews.• o core or supplementary reviews of the Ntopic identified, possibly due to a lack ofprimary studies.
Tentative evidence from reviews to eithersupport or discount the effectiveness of anintervention
Insufficient evidence from reviews to eithersupport or discount the effectiveness of anintervention
No evidence
Source:Modified from Ellis et al., 2003.
118
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Consistent with an evidence-based medicine approach (Glaziou and Heneghan, 2009;Sackett et al., 1996), study designs considered to provide more ‘robust’ evidence of effectwere controlled trials, longitudinal cohort and case-control designs, while ecological, serialcross-sectional and cross-sectional designs were considered to provide ‘weaker’ evidence ofeffect. We do not discount the importance of different study designs and data sources,including cross-sectional and qualitative studies, to evaluate the process and impact of publichealth interventions (Petticrew, 2009), but our aim here is to assess quality of the review-levelevidence.With regard to our interpretation of the reviews’ reported results of primary studies, a‘positive’ finding refers to an observed reduction in the stated outcome associated with theintervention, a ‘negative’ finding refers to an increase in the outcome associated with theintervention, and ‘no association’ refers to no statistically significant effect. Where a reviewreported a finding as positive or negative, it was assumed that the result was statisticallysignificant at the 5 % level even if this was not explicitly stated; where a review reported ‘noassociation’ it was assumed that this indicated a non-statistically significant result (Palmateeret al., 2010).A priori we recognise that no or weak evidence of effectiveness may primarily reflectthe quality and/or number of studies available and does not necessarily indicate alack of intervention effectiveness. We also acknowledge that the history of harmreduction interventions has to a large extent (and necessarily) been driven by communityactions and pragmatic public health policies (See also Cook et al., 2010), with someinterventions implemented in the absence of high-quality trials or intervention-basedresearch.Additionally, in the absence of a recent review for an intervention and/or outcome, wesupplemented our evaluation of the review-level evidence with a review of subsequentlypublished primary literature using the same search strategy and assessment of evidencequality. Thus we undertook primary literature searches for NSPs and HCV incidenceprevalence from 2003, OST and overdose from 2003, DCRs for all outcomes from 2004,and PND and overdose from 2004.
119
Harm reduction: evidence, impacts and challenges
ResultsThe results of the review of reviews literature search are presented in Figure 5.1. We identifiednine (five core and four supplementary) reviews of the effectiveness of NSPs, 11 (three core,six supplementary, two meta-analyses) of OST, four (three supplementary, one meta-analysis)of DCRs, and one supplementary review of PND (Table 5.2).Figure 5.1:Papers identified in the review of reviewsAbstracts and titles identified(n=1334)
Abstracts excluded as notrelevant (n=1065):• id not examine the selected Dinterventions and/oroutcomes; and/or• ot a systematic, meta-Nanalytic or narrative review
Remaining abstracts(excluding duplicates)screened(n=1183)
Remaining full text reviewsretrieved(n=118)
Papers excluded as not relevant(n= 95):• ublished pre-2000 P• ot a review of the literature N• id not address evidence of Deffectiveness of interventions• id not examine selected Doutcomes or interventions• eviews of cost effectiveness R
Remaining reviewscritically appraised(n=23)
Core reviews (n=10)
Meta-analyses (n=3)
Supplementary reviews(n=10)
Source:Adapted from Palmateer et al., 2010.
120
Table 5.2:Summary of reviews by intervention and outcomes
A) Needlesyringe provision: needle syringe programmes, pharmacy access and vending machinesInclusion criteria/terms of referenceReview published and unpublishedstudies on prison NSPs andinterviews with prison NSP expertsReview published studies of the1989 to end NSPseffectiveness of syringe exchange1999programs in reducing HIV risk behaviourand HIV seroconversion among IDUs,regardless of design. Also included studiesthat examined effects of syringe exchangeon HBV and HCV seroconversionExamine the available evidence for theeffectiveness of syringe dispensingmachines and mobile van or bus basedNSPs in making services accessible tohard-to-reach and high-risk groups ofIDUs1990 to(notspecified).Publicationdates to2008NotspecifiedVendingmachinesCore reviewNotPrison NSPsspecified.Publicationsup to 2002Supplementaryreview6 HIV6 HCV
Authorsand date
Title
Datescovered
Interventionscovered
Criticalassessment
No. of studiesby outcome
Dolan et al.,Prison-based syringe exchange2003aprogrammes: a review ofinternational research anddevelopment
Gibson etal., 2001
Effectiveness of syringe exchangeprograms in reducing HIV riskbehaviour and HIVseroconversion among IDUs
3 HCV6 HIV23 self-reportedinjecting riskbehaviour (SR-IRB)
Islam andConigrave,2007
Assessing the role of syringedispensing machines andmobile van outlets in reachinghard-to-reach and high-riskgroups of injecting drug users(IDUs): a review
Supplementaryreview
1 SR-IRB
Jones et al.,A review of the effectiveness2008and cost-effectiveness of needleand syringe programmes forinjecting drug users
NSPs
Core review— ‘review ofreviews’
4 HIV2 HCV5 SR-IRB
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
121
Review of review of NSPeffectiveness in BBV prevention.Primary review NSP effectivenessand cost effectiveness with respectto optimal provision of NSPs bytype, coverage, additional serviceprovision, and provision alongsideOST
Harm reduction: evidence, impacts and challenges
122
Table 5.2(continued)Inclusion criteria/terms of referenceReview studies of NSPs with HIVincidence or prevalence outcomesSummarise results of prison NSPsbased on 10 years’ experience inSwitzerland, Germany, Spain andMoldovaReview published and unpublishedliterature on the effectiveness of HIVprevention interventions (drugdependence treatment, sterileneedle and syringe access, andoutreach and educationprogrammes) for IDUsEvaluate evidence on theeffectiveness of sterile needle andsyringe programming (includingother injecting paraphernalia) forHIV prevention among IDUs indifferent contexts using Bradford-Hill criteriaReview intervention or observational Up to endstudies describing a primary2002prevention intervention targeting IDUsto reduce HCV incidence/prevalence1989 to2002NSPs,pharmacyNSPs, vendingmachines1980 toJanuary2006NSPs,pharmacyNSPs, vendingmachines,provision ofother injectingequipmentCore reviewNotspecified.Publicationdates up to2003Prison NSPsSupplementaryreview6 HIV6 HCV9 SR-IRBUp to Dec2005NSPsCore review13 HIV
Authorsand date
Title
Datescovered
Interventionscovered
Criticalassessment
No. of studiesby outcome
Käll et al.,2007
The effectiveness of needleexchange programmes for HIVprevention: a critical review
Stöver andNelles,2003
Ten years of experience withneedle and syringe exchangeprogrammes in Europeanprisons
Tilson et al.,Preventing HIV infection among2007injecting drug users in high-riskcountries: an assessment of theevidence
5 HCV11 HIV24 SR-IRB
Wodak andEffectiveness of sterile needleCooney,and syringe programming in2004reducing HIV/AIDS amonginjecting drug users
Core review
1 HCV10 HIV28 SR-IRB
Wright andTompkins,2006
A review of the evidence for theeffectiveness of primaryprevention interventions for hepatitisC among injecting drug users
NSPs
Supplementaryreview
11 HCV
Source:Adapted from Palmateer et al., 2010.
B) Opiatesubstitution treatmentInclusion criteria/terms of referenceSummarise major findings of fiveCochrane reviews on OST foropioid dependenceUp to 2003 Outcomesincludedretention intreatment, useof heroin andother drugs,and mortalityNotspecified.Publicationdates up to20001966 to (not MMTspecified).Publicationdates up to2005OST, PND,DCRsSupplementaryreviewMeta-analysis2 OD
Authorsand date
Title
Datescovered
Interventionscovered
Criticalassessment
No. studies byoutcome
Amato etal., 2005
Overview of the systematicreviews of the effectiveness ofopiate maintenance therapies:available research to informclinical practice and research
Best et al.,2000
Overdosing on opiates
Review how opiate overdoses occurand can be prevented
6 OD
Caplehornet al., 1996
Methadone maintenance andaddicts’ risk of fatal heroinoverdose
Use data on dependent heroinusers’ risk of death or the effect ofMMT on that risk
Meta-analysis
5 OD
Darke andHall, 2003
Heroin overdose: research andevidence based intervention
Examine research on heroinoverdose and how this informsevidence-based intervention
Not specified. Drug treatment, SupplementaryPublicationPND, non-reviewdates to 2002 injecting routesof administration,DCRsUp to July2003OSTCore review
5 OD
Gowing etal., 2008
Substitution treatment ofinjection opioid users forprevention of HIV infection
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Systematic review to assess theeffect of OST for opioid dependentIDUs on rates of HIV infections, andhigh-risk behaviours
5 HIV24 SR-IRB
123
Harm reduction: evidence, impacts and challenges
124
Table 5.2, B)(continued)Inclusion criteria/terms of referenceSystematically review evidence onwhether drug abuse treatmentprevents HIV infection1988 to1998MMT and otherdrug treatments(e.g. inpatient,outpatient, drugfree, residential)MMT, PNDSupplementaryreview6 ODCore review6 HIV19 SR-IRB
Authorsand date
Title
Datescovered
Interventionscovered
Criticalassessment
No. of studiesby outcome
SorensenandCopeland,2000Notspecified.Publicationdates to20021990 to (not MMTspecified).Publicationdates up to2006OST and NSPSupplementaryreview
Drug abuse treatment as anHIV prevention strategy: areview
Sporer,2003
Strategies for preventing heroinNot specifiedoverdose
Stallwitzand Stöver,2007
The impact of substitution treatmentReview published an unpublishedin prisons: a literature reviewliterature on effectiveness ofprison-based OST
4 SR-IRB
Tilson et al.,Preventing HIV infection amongReview published and unpublished Up to2007injecting drug users in high-riskliterature on the effectiveness of HIV Januarycountries: an assessment of theprevention interventions for IDUs2006evidence
Core review
4 HIV21 SR-IRB
Wright andTompkins,2006
A review of the evidence for theReview evidence on interventionsUp to Aprileffectiveness of primary preventiontargeting IDUs to reduce prevalence 2003interventions for hepatitis C amongor incidence of HCVinjecting drug usersNotspecified.Publicationdates up to2006
MMT, NSP,behaviouralinterventions,bleach, DCRs,
Supplementaryreview
6 HCV
WHO,2007
Effectiveness of interventions toReview published and unpublishedmanage HIV in prisons: opioidevidence on drug treatment insubstitution therapies and otherpreventing HIV in prisondrug dependence treatment
Prison settings: SupplementaryOST, therapeutic reviewcommunities,counselling,‘boot camp’
2 HCV1 HIV8 SR-IRB
C) Drugconsumption roomsInclusion criteria/terms of referenceDescribe DCR history, practice andevidence on individual and publichealth outcomesReview published articles, novelabstracts, and reviews of grey andnon-English literature on healthimpacts of DCRsUse available peer reviewedestimates of relationship betweenDCR use and syringe sharingSummarise key evaluation findingsincluding HIV risk behaviour and use ofaddiction treatment services2005 to2006Overview ofVancouver DCRevaluationstudiesUp to 2009 DCRsUp to June2007DCRsSupplementaryreviewUp to end2003DCR processSupplementaryindicators andreviewhealth outcomes1 HCV1 HIV13 SR-IRB2 OD10 SR-IRB5 OD
Authorsand date
Title
Datescovered
Interventionscovered
Criticalassessment
No. studies byoutcome
Hedrich,2004
European report on drugconsumption rooms
Kerr et al.,2007
The role of safer injectionfacilities in the response to HIV/AIDS among injection drugusers
Milloy andWood,2009
Emerging role of supervisedinjecting facilities in humanimmunodeficiency virus prevention
Meta-analysis
3 SR-IRB
Wood etal., 2006
Summary of findings from theevaluation of a pilot medicallysupervised safer injecting facility
Supplementaryreview
3 SR-IRB1 OD process
D) Peernaloxone distributionInclusion criteria/terms of referenceDatescoveredJanuary1990 toJune 2004
Authorsand date
Title
Interventionscovered
CriticalassessmentSupplementaryreview
No. studies byoutcome2 OD processProcessindicators ofnaloxonedistribution
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Baca andGrant,2005
Take home naloxone to reduceheroin death
125
Summarise evidence on take homenaloxone, focusing on evidencefrom addiction and emergencymedicine
Harm reduction: evidence, impacts and challenges
Needle and syringe programmes (1)Effects on HIV incidence/prevalenceEvidence of the effects of NSPs on HIV incidence/prevalence was considered in four corereviews (Gibson et al., 2001; Käll et al., 2007; Tilson et al., 2007; Wodak and Cooney,2004), which included a total of 18 primary studies with HIV incidence or prevalenceoutcomes.Tilson et al., 2007 the most recent and rigorous of these reviews, identified 13 relevant studies:,four prospective cohort (Bruneau et al., 1997; Mansson et al., 2000; Schechter et al., 1999;Strathdee et al., 1997), two case-control (Patrick et al., 1997; van Ameijden et al., 1992), threeecological (Des Jarlais et al., 2005b; Hurley et al., 1997; MacDonald et al., 2003), and twoserial cross-sectional studies (Des Jarlais et al., 2005a; Hammett et al., 2006). Other studiesincluded in their discussion were Des Jarlais et al. (1995) and Coutinho (2005).Two of the prospective cohort studies (Bruneau et al., 1997; Strathdee et al., 1997) foundNSP participation was associated with a higher incidence of HIV seroconversion. Tilson etal., 2007 highlighted that these findings may have been related to several factors,including: restrictive service delivery characteristics; high-risk IDUs being more likely to usethe NSP (selection bias); and the availability of clean injecting equipment from othersources (dilution bias).The authors also refer to four ecological studies demonstrating declining HIV incidence/prevalence in the context of NSP provision or expansion (Des Jarlais et al., 1995; Des Jarlaiset al., 2005b; Hurley et al., 1997; MacDonald et al., 2003). Tilson et al. concluded that: ‘Theevidence of the effectiveness of [NSPs] in reducing HIV prevalence is considered modest,based on the weakness of these study designs’ (2007, p. 149). Their conclusions are consistentwith the equivocal results from cohort and case-control studies; this review also undertook themost rigorous evaluation of the primary studies and also considered outcomes related to HIVincidence/prevalence separately from injecting risk behaviour.Käll and colleagues (2007) identified 13 studies examining NSPs and changes in HIVincidence/prevalence outcomes published to the end of 2005, including 11 studies identifiedin other reviews and two additional studies (Amundsen et al., 2003; Valente et al., 2001).With regard to HIV seroincidence, in seven studies there was no reported association withNSPs (Amundsen et al., 2003; MacDonald et al., 2003; Patrick et al., 1997; Schechter et al.,1999; Schoenbaum et al., 1996; Valente et al., 2001; van Ameijden et al., 1992); one studyfound a positive effect (Des Jarlais et al., 1996), and one study found a negative effect(Bruneau et al., 1997).The authors also highlighted three longitudinal studies with a negative baseline associationbetween NSP use and HIV seroprevalence (Bruneau et al., 1997; Millson et al., 2003;Strathdee et al., 1997) and three ecological studies of seroprevalence that found protective(1) This section on NSPs is largely based on Palmateer et al., 2010.
126
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
effects of NSPs (Health Outcomes International et al., 2002; Hurley et al., 1997), butargued that these studies did not control for probable confounding from differences in thestage of the HIV epidemic relative to the introduction of NSPs. Käll and colleaguesconcluded that ‘the effectiveness of NEPs to reduce HIV among IDUs is overrated. Errors incategorising studies in favour of NEPs have been made (Wodak and Cooney, 2004;Wodak and Cooney, 2006) and studies claiming positive results have not been adequatelyscrutinized’ (2007, p. 6).Wodak and Cooney (2004) did not consider separately the effects of NSPs on HIVtransmission versus injecting risk behaviour, and this may have led to the evidence of reducedinjecting risk behaviour having a bearing on conclusions drawn with respect to HIVincidence/prevalence: ‘There is compelling evidence that increasing the availability andutilization of sterile injecting equipment by IDU reduces HIV infection substantially’ (p. 28). Ofthe 38 studies they reviewed, 10 were relevant to HIV (Bruneau et al., 1997; Des Jarlais et al.,1996; Heimer et al., 1993; Hurley et al., 1997; Ljungberg et al., 1991; MacDonald et al.,2003; Monterroso et al., 2000; Patrick et al., 1997; Schechter et al., 1999; Strathdee et al.,1997); five had positive findings (Des Jarlais et al., 1996; Heimer et al., 1993; Hurley et al.,1997; Ljungberg et al., 1991; MacDonald et al., 2003), two had negative findings (Bruneau etal., 1997; Strathdee et al., 1997), and three did not find an association (Monterroso et al.,2000; Patrick et al., 1997; Schechter et al., 1999). Four of the five positive findings weregenerated by studies with weaker designs (Heimer et al., 1993; Hurley et al., 1997; Ljungberget al., 1991; MacDonald et al., 2003).Gibson et al. (2001) reviewed studies published up until 1999, all of which were coveredin the reviews discussed above. They gave consideration to potential bias in studies withnegative results, but not for those with protective findings. They concluded that there is‘Substantial evidence that syringe exchange programmes are effective in preventing [HIVrisk behaviour and] HIV seroconversion among IDU’ (p. 1338). However, as for Wodakand Cooney, their conclusions seemed inconsistent with the HIV studies reviewed: twocohort studies showed an increased risk of HIV infection associated with NSPs (Bruneau etal., 1997; Strathdee et al., 1997), one (meta-analysis using cohort data) showed aprotective effect of NSPs (Des Jarlais et al., 1996), and three (one cohort, two case-control)showed no association (Patrick et al., 1997; Schechter et al., 1999; van Ameijden et al.,1992).The United Kingdom National Institute for Clinical Excellence’ review of optimal NSP servicedelivery (Jones et al., 2008) included a review of reviews component on HIV prevention thatevaluated the four reviews considered above. Consistent with our assessment, theyconcluded:There is evidence from two good-quality systematic reviews [Wodak and Cooney, 2004; Gibsonet al., 2001] to support the effectiveness of NSPs in reducing HIV infection among IDUs. However,findings from two other systematic reviews [Tilson et al., 2007; Käll et al., 2007], including onegood quality review [Tilson et al., 2007], suggest that the evidence may be less convincing.(Jones et al., 2008, pp. 31–2)
127
Harm reduction: evidence, impacts and challenges
Pharmacy accessEvidence of the effectiveness of pharmacy access to needles/syringes in reducing HIVprevalence was examined in one core review (Wodak and Cooney, 2004), whichidentified two relevant studies (Hunter et al., 1995; Nelson et al., 1991). A serial cross-sectional study observed that declines in HIV prevalence in the United Kingdom coincidedwith a period of increased access to needles/syringes through pharmacies and NSPs(Hunter et al., 1995). Second, a cross-sectional survey found a lower HIV prevalence indiabetic IDUs, who had ready access to sterile syringes through pharmacies, comparedwith non-diabetic IDUs (Nelson et al., 1991). They also referred to two studies as evidenceof ‘replication of findings’: an ecological study that found pharmacy exchange was acommon characteristic of cities that had maintained HIV prevalence rates of less than 5 %over the previous five years (Des Jarlais et al., 1995), and a rapid assessment study thatattributed a low HIV infection rate in Georgia in part to the availability of syringes inpharmacies (De Jong et al., 1999).Wodak and Cooney (2004) concluded that ‘There is reasonable evidence that pharmacyavailability of sterile injecting equipment does provide specific benefits in addition to thosederived from NSPs’ (p. 29). We note, however, that this is based on a small number ofprimary studies with weaker designs.Vending machinesOne core review (Wodak and Cooney, 2004) reported the results of a cross-sectional studyof IDUs (Obadia et al., 1999), which found that primary users of vending machines were lesslikely to be HIV positive, although this was not significant after adjustment in a multivariablemodel. The authors stated that ‘Access to sterile needles and syringes from communitypharmacies and syringe vending machines was shown in all nine studies to be effective inreducing risk behaviour and HIV seroprevalence’ (p. 18). We note, however, that thisconclusion is drawn on one study of vending machines with a weak design.PrisonTwo supplementary reviews (Dolan et al., 2003a; Stöver and Nelles, 2003) reported on HIVand HCV incidence from six prison NSP evaluations in Switzerland, Germany and Spain(Jacob and Stöver, 1997; Jacob and Stöver, 2000; Meyeno et al., 2000; Nelles et al., 1997;Villaneuva, 2002). Based on serological testing in five studies and self-report in one study, nonew cases of HIV (or HCV) infections were observed in these prisons during one to two years offollow-up. Both reviews provided limited details about the design and quality of theseevaluation studies.A subsequent German cohort study of prison NSPs and BBV incidence observed four HCVseroconversions among 22 prisoners who were seronegative at baseline during a median 12months of follow-up (incidence rate 18/100 person years). At least one of these exposureswas associated with injecting risk behaviour while in prison (Stark et al., 2006).128
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Evidence statement for NSPs and HIV incidence/prevalencePrimary NSPBased on a tentative statement from one core review, supported by consistent evidence fromless robust primary studies, we conclude that there is tentative evidence to support theeffectiveness of NSPs in reducing HIV incidence/prevalence among IDUs.Pharmacy accessDespite a tentative statement of effectiveness from a core review, the evidence is based on asmall number of primary studies with weak designs. We conclude that there is insufficientreview-level evidence to either support or discount the effectiveness of pharmacy access toneedles/syringes in reducing HIV prevalence among IDUs.Vending machinesThere is insufficient review evidence to either support or discount the effectiveness of needle/syringe vending machines in reducing HIV transmission among IDUs.PrisonGiven a lack of evidence from core reviews, and evidence of uncertain quality fromsupplementary reviews, we conclude that there is insufficient review-level evidence to eithersupport or discount the effectiveness of prison NSPs in reducing HIV transmission amongIDUs.
Effects on HCV incidence/prevalenceEvidence of the effects of NSPs on HCV incidence/prevalence was considered in three corereviews of NSPs and HIV (Gibson et al., 2001; Tilson et al., 2007; Wodak and Cooney, 2004)and one supplementary review (Wright and Tompkins, 2006). The core reviews, however,were focused on HIV outcomes and none examined HCV in any detail, covering sevenprimary studies between them. Wodak and Cooney included one study (Hagan et al., 1995),Tilson et al. identified six (Des Jarlais et al., 2005b; Hagan et al., 1995; Hagan and Thiede,2000; Mansson et al., 2000; Sarkar et al., 2003; Taylor et al., 2000), and Gibson et al.included three (Hagan et al., 1995; Hagan et al., 1999; Lamden et al., 1998).Wright and Tompkins (2006) focused exclusively on HCV outcomes, and identified nineadditional papers (Goldberg et al., 2001; Goldberg et al., 1998; Hernandez-Aguado et al.,2001; Hutchinson et al., 2002; MacDonald et al., 2000; Patrick et al., 2001; Smyth et al.,1999; Somaini et al., 2000; van Ameijden et al., 1993), although three of these presentduplicate data (Goldberg et al., 2001; Goldberg et al., 1998; Hutchinson et al., 2002), andthe search only included studies published up until 2002. There were seven primary studieswith positive findings, but these mainly involved weaker study designs. The stronger studydesigns (cohorts) mainly showed either no association or negative findings between NSPsand HCV seroconversion.
129
Harm reduction: evidence, impacts and challenges
Tilson et al. (2007) concluded there was moderate evidence that ‘HIV preventionprogrammes that include NSPs have less of an impact on HCV transmission than onHIV transmission’ (p. 149). Similarly, in their review of reviews Jones et al. (2008)concluded, ‘There is insufficient evidence from two systematic reviews [Wright andTompkins, 2006; Tilson et al., 2007] to determine the impact of NSPs on hepatitis Cinfection in IDUs’ (p. 32).In our search of the primary literature published since Wright and Tompkins’ we identifiedthree additional cohort studies of HCV incidence and NSP use (Hagan et al., 2004; Roy etal., 2007; van den Berg et al., 2007). Time to HCV seroconversion was not associatedwith being an NSP user at baseline after a median of 2.1 years’ follow-up (Hagan et al.,2004) or with NSP use in the preceding six months (Roy et al., 2007). In the AmsterdamCohort Study among ever IDUs, NSP use alone was not associated with lower risk of HCVseroconversion but full participation in both NSPs and MMT was associated with a lowerrisk of HCV infection in ever IDU compared to no participation (van den Berg et al.,2007).No core or supplementary reviews were identified that examined HCV incidence/prevalenceoutcomes in relation to pharmacy access or vending machines. For details on prison NSPsand HCV incidence/prevalence see the section ‘Prisons’, p. 128.
Evidence statement for NSPs and HCV incidence/prevalencePrimary NSPBased on an absence of clear statements from the core reviews, and inconsistent evidencefrom the primary studies identified in the core reviews and supplementary review, we concludethere is insufficient review-level evidence to either support or discount the effectiveness ofNSPs in reducing HCV transmission among IDUs. Evidence from subsequently publishedlongitudinal primary studies suggests no independent association of NSP use on HCVincidence.Pharmacy access and vending machinesThere is no review-level evidence of the effects of pharmacy access to needles/syringes orvending machines on HCV prevalence/incidence among IDUs.PrisonGiven a lack of evidence from core reviews, and evidence of uncertain quality fromsupplementary reviews, we conclude that there is insufficient review-level evidence to eithersupport or discount the effectiveness of prison NSPs in reducing HCV transmission amongIDUs.
130
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Effects on injecting risk behaviourThe largest body of evidence on the effect of NSPs relates to changes in self-reportedinjecting risk behaviour. Three core reviews reported on a total of 43 studies, 39 of whichshowed a positive effect of NSPs in reducing injecting risk behaviour, and 20 of these werecohort studies.Tilson et al. (2007) identified 25 studies (Bluthenthal et al., 2000; Cox et al., 2000; DesJarlais et al., 2000; Gibson et al., 2002; Hagan et al., 1993; Hagan and Thiede, 2000;Hammett et al., 2006; Hart et al., 1989; Hartgers et al., 1992; Huo et al., 2005; Keene etal., 1993; Klee et al., 1991; Longshore et al., 2001; Monterroso et al., 2000; Ouellet et al.,2004; Schoenbaum et al., 1996; van Ameijden and Coutinho, 1998; van Ameijden et al.,1994; van den Hoek et al., 1989; Vazirian et al., 2005; Vertefeuille et al., 2000; Vlahov etal., 1997; Watters, 1994; Wood et al., 2002; Wood et al., 2003), 14 of which werelongitudinal cohort studies (Bluthenthal et al., 2000; Cox et al., 2000; Gibson et al., 2002;Hagan and Thiede, 2000; Hart et al., 1989; Huo et al., 2005; Monterroso et al., 2000;Ouellet et al., 2004; Schoenbaum et al., 1996; van Ameijden and Coutinho, 1998; vanden Hoek et al., 1989; Vertefeuille et al., 2000; Vlahov et al., 1997; Wood et al., 2002)and demonstrated reductions in self-reported needle sharing (lending or borrowingneedles/syringes). They concluded that there was ‘moderate evidence to show that multi-component HIV prevention programmes that include needle and syringe exchange’ areassociated with a reduction in self-reported sharing of needles and syringes’ (Tilson et al.,2007, p. 154).Wodak and Cooney (2004) identified 28 primary studies of injecting risk behaviour (definedas needle/syringe borrowing, lending, or reuse). Among these studies, there were 24 positive(Bluthenthal et al., 1998; Bluthenthal et al., 2000; Cox et al., 2000; Des Jarlais et al., 1994;Des Jarlais et al., 2000; Donoghoe et al., 1989; Frischer and Elliott, 1993; Gibson et al.,2002; Gleghorn et al., 1998; Guydish et al., 1995; Guydish et al., 1998; Hartgers et al.,1989; Heimer et al., 1998; Keene et al., 1993; Oliver et al., 1994; Paone et al., 1994; Peak etal., 1995; Power and Nozhkina, 2002; Schoenbaum et al., 1996; Singer et al., 1997; vanAmeijden and Coutinho, 1998; van Ameijden et al., 1994; Vlahov et al., 1997; Watters,1994), one negative (Klee et al., 1991), and three indeterminate (Donoghoe et al., 1992;Hartgers et al., 1992; Klee and Morris, 1995) results relating to the association betweenNSPs and injecting risk behaviour. The reviewers did not formulate any conclusionsspecifically regarding injecting risk behaviour.The 23 studies identified by Gibson et al. (2001) (Bluthenthal et al., 1998; Broadhead et al.,1999; Des Jarlais et al., 1994; Donoghoe et al., 1989; Donoghoe et al., 1992; Frischer andElliott, 1993; Guydish et al., 1995; Guydish et al., 1998; Hagan et al., 1994; Hartgers et al.,1989; Hartgers et al., 1992; Keene et al., 1993; Klee et al., 1991; Klee and Morris, 1995;Oliver et al., 1994; Paone et al., 1994; Peak et al., 1995; Schoenbaum et al., 1996; Singeret al., 1997; van Ameijden and Coutinho, 1998; van Ameijden et al., 1994; Vlahov et al.,1997; Watters, 1994) were covered in the later core reviews, with the exception ofBroadhead et al., 1999, and Hagan et al., 1994. Both studies suggested a protective effectof NSP: Broadhead et al. noted an increase in the reported reuse and sharing of syringes131
Harm reduction: evidence, impacts and challenges
after the closure of an NSP, and Hagan et al. observed a decline in the proportionborrowing used syringes among NSP attendees (pre- vs. post-intervention comparison).The authors concluded that there is substantial evidence that NSPs are effective inpreventing HIV risk behaviour among IDUs.
Pharmacy accessTwo core reviews examined evidence of the effects of pharmacy access to needle/syringesand injecting risk behaviour and identified a total of seven studies. Tilson et al. (2007)identified two serial cross-sectional studies that compared injecting risk behaviour beforeand after liberalisation of the laws permitting syringe sale from pharmacies in New York(Pouget et al., 2005) and Connecticut (Groseclose et al., 1995); both found that reports ofsyringe sharing among IDUs declined. The authors concluded, ‘A few studies haveexamined the impact on drug-related HIV risk, and found suggestive evidence of areduction’ (p. 160). Wodak and Cooney (2004) reported on a further five cross-sectionalstudies (Caslyn, 1992; Gleghorn et al., 1995; Ingold and Ingold, 1989; Nelson et al., 1991;Richard et al., 2002) and all found pharmacy access was associated with lower levels ofinjecting risk behaviour.
Vending machinesTwo core reviews, Tilson et al. (2007) and Wodak and Cooney (2004), both referred to apilot study of vending machines in a German prison (Heinemann and Gross, 2001), althoughtheir reporting of the study results differs. Wodak and Cooney reported that significantdecreases in needle-sharing subsequent to the introduction of the programme were found,whereas Tilson et al. stated that this study showed that IDUs will use vending machines as asource of sterile needles/syringes. Tilson et al. concluded that there was insufficient evidenceof the effectiveness of vending machines in reducing HIV risk; the conclusions of Wodak andCooney are as above, for HIV.A supplementary review of vending machines (Islam and Conigrave, 2007) identified 37studies of vending machines that reportedly engaged ‘hard to reach and high risk’ IDUs, butno details were provided on these studies or changes in injecting risk behaviour associatedwith access to vending machines.
PrisonA supplementary review (Stöver and Nelles, 2003) reported on nine prison NSP evaluationsthat had examined injecting risk behaviour. Seven studies found large declines in needle/syringe sharing or reuse, one study found single cases of sharing and one study found nochange in needle sharing. However, few details were provided on the primary study designsor formal data analysis.132
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Evidence statement for NSPs and self-reported injecting risk behaviourPrimary NSPBased on consistent evidence across multiple robust studies, as well as moderate to strongstatements of evidence in support of an effect of NSPs on self-reported injecting risk behaviourfrom two core reviews, there is sufficient review-level evidence to support the effectiveness ofNSPs in reducing self-reported injecting risk behaviour among IDUs.Pharmacy accessBased on less robust studies identified within two core reviews, there is tentative review-levelevidence to support the effectiveness of pharmacy access to needles/syringes — in additionto dedicated NSPs — in reducing self-reported injecting risk behaviour among IDUs.Vending machinesGiven conflicting statements of evidence from core reviews based on one primary study witha weak design, there is insufficient review-level evidence to either support or discount theeffectiveness of vending machines in reducing injecting risk behaviour among IDUs.PrisonDespite consistent findings across multiple studies in a supplementary review suggestingreductions in injecting risk behaviour, due to a lack of information on the quality of the studieswe conclude that there is insufficient review-level evidence to either support or discount theeffectiveness of prison NSPs in reducing self-reported injecting risk behaviour among IDUs.
Opiate substitution treatment (2)Effects on HIV incidence/prevalenceEvidence of the effects of OST on HIV incidence/prevalence was considered in three corereviews (Gowing et al., 2008; Sorensen and Copeland, 2000; Tilson et al., 2007), whichidentified eight studies between them (Dolan et al., 2003b; Hartel and Schoenbaum, 1998;Metzger et al., 1993; Moss et al., 1994; Novick et al., 1990; Rhoades et al., 1998; Serpelloniet al., 1994; Williams et al., 1992). These comprised two randomised control trials (RCTs)(Dolan et al., 2003b; Rhoades et al., 1998), four cohort studies (Hartel and Schoenbaum,1998; Metzger et al., 1993; Moss et al., 1994; Williams et al., 1992), one case-control study(Serpelloni et al., 1994), and one cross-sectional study (Novick et al., 1990).
(2) Most of the review-level evidence on the effectiveness of OST relates to MMT, but the findings can be largely taken torefer to OST in general.
133
Harm reduction: evidence, impacts and challenges
Three cohort studies showed the odds of HIV seroconversion were greater for untreatedindividuals or those with interrupted MMT compared to those who remained continuouslyin MMT (Metzger et al., 1993; Moss et al., 1994; Williams et al., 1992). A cohort study andcase control study showed lower daily dose and more time out of MMT was alsoassociated with higher risk of HIV seroconversion (Hartel and Schoenbaum, 1998;Serpelloni et al., 1994). In an RCT of 50mg versus 80mg MMT no seroconversions occurredin six months of follow-up (Rhoades et al., 1998). A retrospective cohort study found noHIV seroconversions among long-term MMT patients (Novick et al., 1990). An RCT of MMTin prison found no difference in HIV incidence between those in MMT and waitlist controls,although this was in the context of a short period of follow-up and low HIV prevalence(Dolan et al., 2003b).The conclusions from all three reviews allowed that continuous MMT is associated with lowerrates of HIV seroconversion while acknowledging that those who resist treatment or leavetreatment may inherently engage in more HIV risk behaviours than those who stay intreatment longer.Specifically, Gowing et al. (2008), in their Cochrane Review (updated from an earlier versionin 2004), concluded, ‘Few data … limit the conclusiveness of any analysis, but these studiesconsistently indicate lower rates of [HIV] seroconversion associated with substitutiontreatment. This suggests that reductions in risk behaviour do translate into actual reduction incases of HIV infection’ (p. 22); Tilson et al. (2007) concluded that:Modest evidence from prospective cohort and case-control studies shows that continuous opioidagonist maintenance treatment is associated with protection against HIV seroconversion. Thisassociation persists after controlling for many confounders. These studies also show that the riskof HIV seroconversion is inversely related to length of time in treatment. However the possibilityof bias in these findings from self selection cannot be ruled out.(Tilson et al., 2007, p. 92)
Finally, Sorensen and Copeland (2000) concluded that:Four out of the six studies reviewed … provided firm evidence for the protective effect of MMTagainst HIV seroconversion. These findings are more convincing because they are based onbiologically verified outcomes … [but] nearly all the studies are inherently limited by a self-selected treatment sample.(Sorensen and Copeland, 2000, p. 27)
PrisonOne core review of OST (Gowing et al., 2008) and two supplementary reviews of prisonOST (Stallwitz and Stöver, 2007; WHO et al., 2007) identified the same RCT describedabove (Dolan et al., 2003b).134
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Evidence statement for OST and HIV incidence/prevalenceBased on consistent evidence from three core reviews, there is sufficient review-level evidenceto conclude that OST in community settings is effective in reducing HIV seroconversion,especially among those in continuous treatment.There is insufficient review-level evidence to draw conclusions about the effect of OST on HIVseroconversion in prison settings. Data from one RCT in a jurisdiction with low HIV prevalencefound no difference in HIV incidence between those receiving MMT and controls.
Effects on HCV incidence/prevalenceOne supplementary review (Wright and Tompkins, 2006) examined evidence of the effectsof OST on HCV incidence/prevalence and identified six studies. A cohort and a case-control study found a non-significant trend toward lower HCV incidence among those inMMT compared to those not in treatment (Rezza et al., 1996) or those who have lefttreatment (Thiede et al., 2000). A Dutch cohort study found MMT (in combination withNSPs) was not associated with any decreases in annual HCV incidence over four years(van Ameijden et al., 1993). Three cohort studies did not find any differences in HCVincidence between those in MMT and those not in MMT (Chamot et al., 1992; Crofts et al.,1997; Selvey et al., 1997).Wright and Tompkins (2006) concluded that, ‘As regards methadone maintenance therapy,whilst it has been successful in reducing the incidence of HIV, the evidence for its effectivenessin reducing HCV incidence is less convincing’ (p. 5).In our primary literature search we identified five community-based studies of HCV and OSTpublished since Wright and Tompkins’ review. Three cohort studies suggested a positive impactof OST: HCV incidence was lower among those in continuous OST compared with those withinterrupted OST (Hallinan et al., 2004); MMT in the past six months was protective against bothprimary (non-infected IDUs) and secondary (mono-infected IUDs) HIV and HCV infection (Milleret al., 2004); and HCV incidence was similar among those who were not in OST during follow-up or in OST for up to six months, but was lower amongst those in treatment for 7 to 12 months(Craine et al., 2009). One cohort study found no difference in risk of HCV seroconversionamong IDUs recruited from MMT clinics and IDUs recruited from NSPs (Maher et al., 2006)and in the Amsterdam Cohort Study, as described earlier, MMT alone was not associated withlower risk of HCV seroconversion but full participation in both MMT and NSPs was associatedwith a lower risk of HCV infection (van den Berg et al., 2007).PrisonTwo supplementary reviews of prison OST (Stallwitz and Stöver, 2007; WHO et al., 2007)identified two linked studies (Dolan et al., 2003b; Dolan et al., 2005). There was no135
Harm reduction: evidence, impacts and challenges
difference in HCV incidence between RCT prison MMT and waitlist control groups at five-month follow-up (Dolan et al., 2003b). However, at four-year follow-up, retention in MMTwas associated with reduced HCV infection, while short MMT episodes (less than five months)were significantly associated with greater risk of HCV (Dolan et al., 2005).
Evidence statement for OST and HCV incidence/prevalenceBased on consistent evidence showing weak or no association from multiple longitudinalstudies within a supplementary review, we conclude that there is tentative review-levelevidence of OST having limited impact on HCV transmission. However, taken together withrecently published primary studies, the available evidence suggests OST contributes to areduction in the risk of HCV seroconversion among those in continuous treatment.There is insufficient review-level evidence to either support or discount the effectiveness ofOST with respect to HCV transmission in prison settings. One RCT suggests that retention inMMT from prison to community settings is associated with reduced HCV incidence.
Effects on injecting risk behaviourThree core reviews examined the effect of OST on injecting risk behaviour. The evidence fallsinto three broad categories: prevalence and frequency of injection; sharing of injectingequipment; and scores of drug-related risk.Gowing et al. (2008) identified one RCT (Dolan et al., 2003b) and six cohort studies thatreported the prevalence of injecting drug use before and after OST (Camacho et al.,1996; Chatham et al., 1999; Gossop et al., 2000; King et al., 2000; Magura et al., 1991;Teeson et al., 2006); three RCTs (Dolan et al., 2003b; Lott et al., 2006; Strang et al.,2000) and six cohort studies that reported frequency of injection at baseline and follow-up (Batki et al., 1989; Brooner et al., 1998; Camacho et al., 1996; Chatham et al., 1999;Kwiatkowski and Booth, 2001; Simpson et al., 1995); and two cohort studies thatexamined both the proportion and frequency of injection (Camacho et al., 1996; Chathamet al., 1999). Tilson et al. identified the same studies except Teeson et al., 2006 and Lott etal., 2006. The studies varied in terms of follow-up periods (range 3 to 12 months) and themeasurement of frequency of injecting, but all studies showed statistically significantdecreases in injecting risk behaviour from baseline to follow-up (Gowing et al., 2008;Tilson et al., 2007).Sorensen and Copeland (2000) refer to a further nine studies with data on injectionprevalence and frequency: one RCT and four cohort studies of in-treatment samples showedretention in MMT was associated with decreases in injection frequency (Abbott et al., 1998;Ball et al., 1998; Iguchi, 1998; Saxon et al., 1994; Shore et al., 1996); and one cohort andthree cross-sectional studies comparing those in treatment with non-treatment samples found136
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
MMT associated with fewer injections (Baker et al., 1995; Greenfield et al., 1995; Meandzijaet al., 1994; Stark et al., 1996).Gowing et al. (2008) identified three RCT and six cohort studies that examined theproportion who reported sharing equipment before and after a period of MMT. Tilson etal. (2007) identified the same studies except Teeson et al. (2006) and Schroeder et al.(2006). Eight out of nine (Camacho et al., 1996; Chatham et al., 1999; Dolan et al., 2003b;Gossop et al., 2000; Grella et al., 1996; Margolin et al., 2003; Schroeder et al., 2006;Teeson et al., 2006) found a significant reduction in sharing between baseline and follow-up. The ninth study (King et al., 2000), found a non-significant reduction in reportedsharing.Sorensen and Copeland (2000) additionally reported on one RCT and three cohort studies ofin-treatment samples that showed that retention in MMT was associated with decreases insharing of injecting equipment (Camacho et al., 1996; Magura et al., 1998; Rhoades et al.,1998; Saxon et al., 1994) and one cross-sectional study that found no differences in sharingbetween new treatment entrants and the rest of the sample (Caslyn et al., 1991). One cohortstudy and four cross-sectional studies comparing those in treatment with non-treatment foundMMT was associated with decreased sharing (Caplehorn and Ross, 1995; Greenfield et al.,1995; Klee et al., 1991; Longshore et al., 1993; Stark et al., 1996) and one cross-sectionalstudy found no differences in sharing (Baker et al., 1995).Gowing et al. (2008) identified four RCTs, one cohort and two cross-sectional studiescomparing drug-related HIV risk scores among those in and out of OST (Abbott et al.,1998; Avants et al., 1998; Baker et al., 1995; Chatham et al., 1999; Mark et al., 2006;Marsch et al., 2005; Sees et al., 2000). Tilson et al. (2007) identified the same studiesexcept Mark et al. (2006) and Marsch et al. (2005). Four studies (Abbott et al., 1998;Avants et al., 1998; Chatham et al., 1999; Marsch et al., 2005) found significant decreasesin drug-related HIV risk behaviour scores before and after OST. Sees et al. (2000) foundno significant difference in mean risk scores between intake and six-month follow-upbetween MMT and methadone detoxification groups. Finally, Baker et al. (1995) and Market al. (2006) compared the drug risk scores for those currently in OST and not in OST andin both studies the mean score was significantly lower for the cohort receiving OST at thetime of interview.The conclusions of all three core reviews allowed that OST was associated with reductions inself-reported prevalence and frequency of injection, sharing of injecting equipment andinjecting risk behaviour risk scores. Gowing et al. (2008) concluded:Substitution treatment is associated with a significant decrease in the proportion of participantsreporting injecting drug use and in the frequency of injection … [and] a significant decrease inthe sharing of injecting equipment … studies that reported [injecting risk behaviour] scores alsoshowed a significant reduction is risk associated with substitution treatment.(Gowing et al., 2008, pp. 19–20)
137
Harm reduction: evidence, impacts and challenges
Tilson et al. (2007) concluded:Moderate to strong evidence from one RCT and a number of observational studies show that patientsreceiving methadone maintenance treatment report reductions in several drug-related HIV riskbehaviours, including frequency of injecting and sharing of injecting equipment. These patients alsohad lower summary scores of drug-related risk behaviour compared with pre-treatment levels.(Tilson et al., 2007, p. 89)
Sorensen and Copeland (2000) concluded,26 out of 28 studies showed positive results in reducing HIV risk behaviours … In this review bothlongitudinal studies of in-treatment samples and studies comparing treatment patients with othersamples found very strong evidence that drug abuse treatment decreases the risk of HIV infectionby decreasing needle-use. The evidence is less strong, but still substantial, that drug abusetreatment changes the needle use patterns of participants (e.g. less needle-sharing, more use ofsterile needles).(Sorensen and Copeland, 2000, pp. 27–8)
PrisonTwo supplementary reviews examined prison OST and injecting risk behaviour (Stallwitzand Stöver, 2007; WHO et al., 2007). WHO et al. identified seven studies of prison-basedOST and injecting risk behaviour (Bayanzadeh et al., undated; Boguña, 1997; Dolan etal., 1996; Dolan et al., 1998; Dolan et al., 2003b; Heimer et al., 2005; Heimer et al.,2006), although some of these studies reported very similar findings from the same dataset (i.e. Heimer et al., 2005 and 2006; Dolan et al., 1996 and 1998). Stallwitz and Stöver(2007) also referred to three studies included in WHO et al. (Boguña, 1997; Dolan et al.,1998; Dolan et al., 2003b). Across all studies, opioid-using IDUs who received MMT inprison reported injecting significantly less frequently than those not receiving MMT inprison. WHO et al. concluded: ‘Prison-based OST programmes appear to be effective inreducing the frequency of injecting drug use and associated sharing of injectingequipment, if a sufficient dosage is provided and treatment is provided for longer periodsof time’ (p. 9).
Evidence statement for OST and injecting risk behaviourBased on consistent evidence from multiple robust studies in three core reviews there is sufficientreview-level evidence to support the effectiveness of OST in reducing the frequency of injection,the sharing of injecting equipment and injecting risk behaviour scores.Based on consistent evidence from two supplementary reviews there is tentative evidence tosupport the effectiveness of prison-based OST in reducing injecting risk behaviour amongIDUs in prison by reducing frequency of injection of heroin and other opiate use.
138
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Effects on overdose-related mortalityWe identified two meta-analyses (Amato et al., 2005; Caplehorn et al., 1996) and threesupplementary narrative reviews that considered OST and overdose-related mortality (Best etal., 2000; Darke and Hall, 2003; Sporer, 2003). Between them they referred to 14 primarystudies (Caplehorn et al., 1994; Cushman, 1977; Darke and Ross, 1999; Darke et al., 2000;Davoli et al., 1993; Fugelstad et al., 1995; Gearing and Schweitzer, 1974; Gronbladh et al.,1990; Gunne and Gronbladh, 1981; McGregor et al., 2002; Poser et al., 1995; vanAmeijden et al., 1999; Yancovitz et al., 1991; Zador et al., 1996).Amato et al. (2005) synthesised the results of five systematic reviews of OST effectiveness intreating opioid dependence. However, they were only able to pool data for all causemortality for MMT versus waiting list/no treatment from two controlled studies (Gunne andGronbladh, 1981; Yancovitz et al., 1991) and found non-significant trend suggestive of areduced risk of death in MMT (RR 0.15, CI 0.02-1.0). The authors concluded, ‘Death within thetime frames of a clinical trial is a rare event, even in a high risk population like opiate users… for the statistical power needed to study mortality, big RCTs or long follow-up periods arerequired’ (p. 325).Caplehorn et al. (1996) conducted a meta-analysis of mortality in and out of MMT based onthe results of the aforementioned RCT (Gunne and Gronbladh, 1981) and five cohort studies(Caplehorn et al., 1994; Cushman, 1977; Gearing and Schweitzer, 1974; Gronbladh et al.,1990; Poser et al., 1995) from Sweden, Germany, Australia and the United States. MMTreduced risk of death by 75 % (relative risk 0.25, CI 0.19-0.33), due almost entirely todecreases in deaths due to overdose. Notably the included results were all from high-doseprogrammes. They concluded:Addicts were one-quarter as likely to die while in methadone maintenance treatment becausethey were less likely to die from heroin overdose or suicide. These are most probably direct,pharmacological effects of methadone and are likely to be dose-dependent. This conclusion givesstrong support to the argument that all heroin addicts should have access to high-dose, long termmaintenance treatment.(Caplehorn et al., 1996, p. 190)
Other studies referred to in the three supplementary reviews (Best et al., 2000; Darke andHall, 2003; Sporer, 2003) highlight that overall risk of overdose death is reducedsignificantly while in treatment compared to never being in treatment or after leavingtreatment. An Italian case-control study of 4 200 IDUs found the risk of overdose deathwas over three times higher among those who left MMT compared to those still intreatment, and over seven times higher in the first 12 months after leaving treatment (Davoliet al., 1993). In a Swedish cohort study of 472 HIV-infected IDUs, risk of death by overdoseor trauma was reduced by 75 % while in MMT compared to never being in treatment(Fugelstad et al., 1995).A trend toward a dose-dependent reduction in the risk of overdose death was alsoobserved in a Dutch cohort study, where the risk of death among those on 55 mg or more139
Harm reduction: evidence, impacts and challenges
was a third of that in patients on lower doses (van Ameijden et al., 1999). Additionallysystematic audits of coronial data on heroin-related deaths in Australia have shown thataround 98 % of deaths occurred among individuals not enrolled in MMT at the time oftheir death (Darke and Ross, 1999; Darke et al., 2000; McGregor et al., 2002; Zador etal., 1996).Conclusions from all three supplementary reviews consistently supported that being inOST is associated with a substantial reduction in the risk of opioid overdosecompared to no treatment or after leaving treatment. Best et al. (2000) also highlightedthat the risk of overdose death during treatment is greatest during induction and thatrisk of death out of treatment is greatest immediately after leaving/being droppedfrom treatment.We identified four longitudinal primary studies of OST and overdose-related mortalitypublished since 2003, which all found significant reductions in mortality risk during treatmentcompared to when out of treatment (Brugal et al., 2005; Clausen et al., 2008; Davoli et al.,2007; Degenhardt et al., 2009).An Italian prospective cohort study of 10 454 heroin users entering treatment found thoseretained in MMT had a 90 % reduced risk of death compared to those not in treatment(Davoli et al., 2007). Similarly in a Spanish cohort of 5 049 heroin users enteringtreatment, risk of overdose death was seven times greater for those not in MMT at the timeof death (Brugal et al., 2005). A Norwegian prospective data linkage study of mortalityamong 3 789 heroin users who applied for OST showed risk of overdose death wasreduced by 80 % while in treatment compared to OST waiting list or after leavingtreatment (Clausen et al., 2008). In an Australian state-wide OST retrospective data linkagestudy of 42 676 individuals entering treatment over a 20-year period, OST contributed to a29 % reduction in mortality (mostly due to overdose and trauma) across the entire cohort(Degenhardt et al., 2009).Finally, an ecological study of access to OST and overdose deaths in France during a rapidscale-up of OST (particularly BMT) suggests that as the number of drug users in OSTincreased, there was a concurrent rapid decline in the annual number of opioid relatedoverdose deaths (Emmanuelli and Desenclos, 2005).PrisonWHO et al. (2007) note recent release from prison as a significant risk factor for drugoverdose and the importance of drug treatment through-care. They identified one study ofprison MMT and post-release mortality (Dolan et al., 2005). In a four-year follow-up of 382prison-based MMT RCT participants, no deaths occurred while participants were in MMT, but17 died out of MMT (untreated mortality rate of 2.0 per 100 person-years, 95 % CI, 1.2-3.2).Eight deaths were from drug overdose, four had never received MMT and four had ceasedMMT prior to release from prison.140
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Evidence statement for OST and overdoseBased on consistent evidence from one meta-analysis and multiple robust studies insupplementary reviews, there is sufficient review-level evidence to support the effectiveness ofOST in reducing the risk of opioid overdose death. Recently published high-quality primarystudies also support that OST reduces risk of overdose death for those retained in treatmentcompared to those waiting for treatment or who have left treatment.There is insufficient review evidence to support or discount the effectiveness of prison-basedOST and overdose prevention. Findings from one post-RCT follow-up study suggest thatretention in prison based OST after release was associated with reduced mortality.
Supervised drug consumption facilitiesEffects on HIV and HCV incidence/prevalenceA supplementary review (Hedrich, 2004) identified two linked studies that examined the effectof DCR on operation BBV incidence/prevalence in Sydney (MSIC Evaluation Committee, 2003).No evidence of an increase or decrease in the incidence of notifications for HIV, HCV or HBVinfections in the DCR locality compared to control localities were attributable to the operation ofthe DCR (MSIC Evaluation Committee, 2003). It was acknowledged a priori that low populationprevalence of these infections and the limited coverage of one DCR made it unlikely therewould be a detectable community-level impact on BBV incidence (MSIC Evaluation Committee,2003). Complimentary case-control and serial cross-sectional studies of HCV incidence andHCV prevalence respectively among IDUs in the DCR locality found HCV incidence was stableand that a trend towards increased HCV prevalence was consistent with national trends amongIDUs (MSIC Evaluation Committee, 2003).Hedrich (2004) concluded:Few data are available regarding the impact of the rooms on the incidence of infectious diseasesamong clients. Methodologically, it is difficult to establish a causal effect of the rooms per se thatcan be distinguished from the effects of the gamut of health promotion and harm reductionactivities aimed at preventing drug-related infectious diseases.(Hedrich, 2004, p. 77)
Evidence statement for DCRs and HIV/HCV incidence/prevalenceThere is insufficient review-level or primary evidence to support or discount the effect of DCRson HIV or HCV prevalence/incidence.
141
Harm reduction: evidence, impacts and challenges
Effects on injecting risk behaviourTwo supplementary reviews (Hedrich, 2004; Kerr et al., 2007), a synthesis of Vancouverevaluation findings (Wood et al., 2006) and a meta-analysis (Milloy and Wood, 2009)examined evidence of the effect of DCR use on self-reported (and in some instances staff-reported) injecting risk behaviour.Hedrich (2004) identified 13 studies of DCRs and injecting risk behaviour (Benninghoff andDubois-Arber, 2002; Benninghoff et al., 2003; Jacob et al., 1999; Linssen et al., 2000; Meijeret al., 2001; Minder Nejedly and Bürki, 1996; MSIC Evaluation Committee, 2003; Poschadelet al., 2003; Reyes Fuentes, 2003; Ronco et al., 1996; van der Poel et al., 2003; Zurhold etal., 2001). These comprised mostly serial and single cross-sectional studies with small samplesizes. However, they consistently showed a positive impact of DCR use on injecting-relatedrisk behaviour, including: improved knowledge and/or practice of injecting hygiene andsafer use (Benninghoff and Dubois-Arber, 2002; Benninghoff et al., 2003; Jacob et al., 1999;Linssen et al., 2000; Meijer et al., 2001; MSIC Evaluation Committee, 2003; Poschadel et al.,2003; van der Poel et al., 2003; Zurhold et al., 2001); increased use of sterile injectingequipment for all injections (Minder Nejedly and Bürki, 1996; MSIC Evaluation Committee,2003; Reyes Fuentes, 2003; Ronco et al., 1996); decreases in needle syringe and otherequipment sharing (Benninghoff and Dubois-Arber, 2002; Benninghoff et al., 2003; Dubois-Arber et al., 1999; MSIC Evaluation Committee, 2003).Hedrich concluded:Clients of consumption rooms report improved knowledge of safer use and injection techniquesas well as reductions in risk behaviour. Positive behavioural changes are confirmed by staff,although this process is sometimes slow. Despite methodological limitations, it is likely that saferuse education given at consumption rooms has contributed to this. Effects increase with lengthand frequency of service use and behaviour changes are sustained outside the facilities.(Hedrich, 2004, p. 77)
Kerr et al. (2007) referred to seven of the same studies as Hedrich (2004) (Benninghoff andDubois-Arber, 2002; Benninghoff et al., 2003; Jacob et al., 1999; Meijer et al., 2001; MinderNejedly and Bürki, 1996; Ronco et al., 1996; van der Poel et al., 2003) and Kerr et al. (2007)and Wood et al. (2006) both referred to three studies of DCR use and injecting riskbehaviour from the prospective IDU cohort studies of the Vancouver evaluation (Kerr et al.,2005; Stoltz et al., 2007; Wood et al., 2005). The prevalence of syringe sharing decreased inthe cohort after the facility opened and only among DCR users (Kerr et al., 2005). RegularDCR use was associated with reduced syringe lending by HIV-infected IDUs and reducedsyringe borrowing by HIV-negative IDUs (Wood et al., 2005). DCR use was independentlyassociated with decreased reuse of syringes, increased use of sterile water and increased useof alcohol swabbing of injection sites (Stoltz et al., 2007).Milloy and Wood (2009) combined the effects of DCR use on syringe sharing from Canadian(Kerr et al., 2005; Wood et al., 2005) and Spanish (Bravo et al., 2009) cohort studies. Their142
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
pooled estimate of 0.31 (95 % confidence interval 0.17-0.55) represented a 69 % reduction inthe likelihood of syringe sharing among DCR users.
Evidence statement for DCRs and injecting risk behaviourBased on consistent evidence from multiple studies identified in two supplementary reviewsand a meta-analysis we conclude there is tentative review-level evidence that DCR use isassociated with reduced injecting risk behaviour and improvements in injecting practices andhygiene, especially for injections that occur on DCR premises, and among those who areregular DCR users.
Effects on overdose mortalityTwo supplementary reviews (Hedrich, 2004; Kerr et al., 2007) identified an ecological studyof DCRs and overdose mortality. A time series study of drug-related deaths in four Germancities found a significant association between the operation of DCRs (often in multiple sites)and the reduction of drug-related deaths (Poschadel et al., 2003). Hedrich (2004) alsodescribed another time series study of DCR operation and overdose deaths and ambulancecall-outs to suspected opioid overdoses in Sydney, which was inconclusive due toconfounding changes in the drug market after the opening of the DCR that led to a significantreduction in heroin use (MSIC Evaluation Committee, 2003).Potential deaths prevented by DCR operation have also been estimated. Hedrich (2004)reported on a multiplier estimation study from Sydney that suggested that clinical interventionstaff prevented at least four deaths per year (MSIC Evaluation Committee, 2003). Hedrich(2004) also applied a mortality rate of 2 % to data on annual supervised drug consumptionepisodes in Germany (Poschadel et al., 2003), assuming that one ‘person year of active use’equals 1 000 consumptions, and estimated that at least 10 deaths per year were preventedby the operation of DCRS in Germany.Hedrich (2004) concluded:There is some evidence ... that consumption rooms can contribute to a reduction in drug-relateddeaths at community level. The robustness of these analyses remains to be verified by furtherresearch data based on longitudinal analyses in different contexts that reproduce these resultsacross time or geographic location … There is no evidence at all that consumption roomscontribute to increased morbidity or mortality risks among drug users. Millions of drugconsumptions have been supervised and thousands of emergencies been treated — with nodeaths from overdose.(Hedrich, 2004, p. 77)
143
Harm reduction: evidence, impacts and challenges
Evidence statement for DCRs and overdose deathsThere is insufficient review-level evidence to support or discount the effect of DCRs on reductionof overdose deaths at the community level. One time-series study found DCR operation wasassociated with reduced drug-related deaths at a city level. Process data show no overdosedeaths have occurred on DCR premises and clinical and epidemiological data suggest it islikely that a proportion of overdoses treated in DCR settings would have been fatal if they hadoccurred elsewhere.
Peer naloxone distributionWe identified one supplementary review of PND to reduce heroin deaths (Baca and Grant,2005), which reported limited process outcomes of two early PND programmes (Bigg, 2002;Dettmer et al., 2001).The process evaluation literature on PND has grown considerably since that review and weidentified nine subsequently published primary studies (Galea et al., 2006; Green et al.,2008; Piper et al., 2008; Seal et al., 2005; Sherman et al., 2009; Strang et al., 2008; Tobinet al., 2009; Wagner et al., 2009).Taken together, the evidence from four prospective studies (Seal et al., 2005; Strang et al.,2008; Tobin et al., 2009; Wagner et al., 2009) and three cross-sectional studies (Green et al.,2008; Piper et al., 2008; Sherman et al., 2009) suggests that overdose prevention trainingwith PND increases participants’ knowledge, confidence and skills to respond effectively incase of overdose. Evidence from five prospective studies (Galea et al., 2006; Seal et al.,2005; Strang et al., 2008; Tobin et al., 2009; Wagner et al., in press) and three cross-sectional studies (Dettmer et al., 2001; Piper et al., 2008) suggests PND trainees subsequentlyintervene at overdose using naloxone with very high reported rates of survival in cases wherethe outcome of intervention is known.
Effects on overdose mortalityWe identified one ecological study that examined the impact of PND on overdose mortalityat the community level. In Chicago, a large-scale PND programme has been operating since2001 with more than 3 500 vials of naloxone prescribed and 319 naloxone reversalsreported by programme participants. Coronial data showed that the upward trend in heroinoverdose deaths annually in Chicago prior to the PND programme, which increased four-fold between 1996 and 2000, reversed in 2001, with a 20 % decrease in 2001 and a 10 %decreases in 2002 and 2003 (Maxwell et al., 2006).144
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Evidence statement for PND and overdoseThere is insufficient review-level evidence to draw conclusions about the effect of PND onoverdose deaths. Recently published primary studies consistently point to the feasibility anduptake of PND programmes. One ecological study suggests the operation of a large PNDprogramme may have played a role in reducing overdose deaths at the city level.
DiscussionDrawing substantively upon our previous work in this area (Palmateer et al., 2008; Palmateeret al., 2010), we have used a review of reviews methodology to evaluate the evidencerelating to the effectiveness of selected harm reduction interventions on key indicators ofinjecting-related morbidity and mortality: NSPs, OST, DCRs on HIV and HCV incidence/prevalence and injecting risk behaviour; and OST, DCRs, and PND on overdose-relateddeaths.We find that there is sufficient review-level evidence that OST reduces HIV transmission, whilethe review evidence in support of NSPs reducing HIV transmission is more tentative, and forDCRs currently insufficient. We find there is tentative review-level evidence that OST haslimited effectiveness in reducing HCV transmission, and insufficient evidence to support ordiscount that NSPs or DCRs reduce HCV transmission. We find there is sufficient review-levelevidence that NSPs, OST and DCRs reduce self-reported injecting risk behaviour andtentative review-level evidence to suggest that pharmacy access, in addition to primary NSP,is effective in reducing injecting risk behaviour. There is sufficient review-level evidence thatOST is effective in reducing opioid overdose related mortality but insufficient review-levelevidence to support or discount the effectiveness of DCRs and PND in reducing overdosedeaths at the community level.Our findings highlight a lack of high-quality reviews for some harm reductioninterventions and/or outcomes we considered. In some cases this reflects a lack of primarystudies (e.g. DCRs and PND). It also appears that previous reviews of NSPs may haveoverstated the evidence of effectiveness in BBV prevention from the available studies. Ingeneral, we found that reviews gave more consideration to issues of bias and limitationsin studies with negative findings than in studies with positive (protective) findings, and thusmay have ascribed less importance to negative studies when synthesising the evidence(Palmateer et al., in press).As highlighted earlier, an assessment of insufficient or tentative review-level evidence doesnot equate to evidence for lack of intervention effectiveness. Such assessments are inevitablyrelated to the methodological limitations of primary studies as well as the reviews (Palmateeret al., 2010). For example, one of the criticisms of studies investigating NSPs’ effectiveness inpreventing BBVs is that they do not accurately measure the coverage or intensity of theintervention delivered (that is, the amount of injecting equipment distributed) (Lurie, 1997).145
Harm reduction: evidence, impacts and challenges
Further consideration of the limitations of the primary studies helps to explain our finding of adiscrepancy between the results of individual-level (i.e. cohort and case-control) andecological studies of NSP effectiveness (Palmateer et al., 2010). First, individual-level, non-randomised studies are highly susceptible to bias. In cohort studies, for example, two groups,such as NSP attenders and non-attenders, are usually compared to the outcome. Thismeasurement of the exposure to the intervention has generally been limited because: (i) thesegroups are ‘self-selecting’ and thus may be inherently different with respect to characteristics,including injecting risk, that can influence the outcome (Lurie, 1997), and (ii) the distinctionbetween exposed and unexposed groups may also be inadequate (for example, unexposedindividuals may have access to clean needles/syringes from other sources or exposedindividuals may still be engaging in injecting risk despite high uptake of NSP), potentiallydiluting the effect size (Gibson et al., 2001).Ecological studies, by contrast, are more likely to report a positive association: because onecannot isolate the effects of a single intervention in an ecological study, such studies may infact be measuring the impact of several interventions. This is illustrated in the AmsterdamCohort Study (ACS), which found that MMT or NSP use alone were not associatedsignificantly with HIV or HCV seroconversion, but that full participation in both programmeswas associated with a lower incidence of HCV and HIV infection, suggesting that only thecombination of these interventions might contribute to the reduction of the transmission ofthese infections (van den Berg et al., 2007).All of the evidence for NSP, DCR and PND effectiveness is based on observational studydesigns, that is, exposure has not been randomised. Observational studies, as discussedabove, are generally at risk of confounding and selection bias. However, it is logisticallyand ethically difficult to conduct a randomised trial for interventions such as NSPs andDCRs, which have face validity and have already been widely introduced (Hall andKimber, 2005; Lurie, 1997). A feasible alternative study design is a community-randomisedtrial (e.g. comparing a basic package of harm reduction services with an enhancedpackage) where participants are randomised on a group basis, rather than an individualbasis, thereby avoiding some of the biases associated with observational designs (Tilson etal., 2007).Another methodological issue is that the primary studies might not have been adequatelypowered to detect an impact. Few of the reviews addressed this issue in their reporting of thestudies and, therefore, it was usually unclear whether equivocal findings were due to a lackof power or truly represented no association (Palmateer et al., 2010).The reliance on self-reported behaviour is a problem for epidemiological studiesexamining the effectiveness of harm reduction interventions. Self-reported behaviour bydrug users can be reliable (Darke, 1988; Goldstein et al., 1995); however, it is unclearwhether this applies to all behaviours. Limitations, for example, in the reliability self-reported injecting risk behaviour may explain our finding of greater strength of evidencefor behavioural measures than for biological measures. Differential reporting of riskbehaviour between exposed and unexposed groups could bias measures of theeffectiveness of an intervention, for example if IDUs exposed to NSPs are more sensitised146
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
to the risks of sharing and more reluctant to report this behaviour than unexposedindividuals (Palmateer et al., 2010). Second, some modelling studies (Vickerman et al.,2006) have suggested that the association between injecting risk behaviour and HIV/HCV transmission does not follow a dose-response relationship; rather, a reduction ininjecting risk has to surpass a threshold level before changes in HIV/HCV transmissionare observed. Consequently, a sub-threshold change in injecting risk behaviour mayhave no impact on HIV/HCV incidence, thereby limiting the usefulness of injecting riskbehaviour as a proxy measure for the effectiveness of an intervention (Palmateer et al.,2010).We acknowledge that we may have missed potentially relevant reviews by limiting our searchto English language reviews, although we attempted to expand the search, and reducepublication bias, by examining the grey literature. In particular in the reviews of DCRs, prisonNSPs and prison OST there is good coverage of non-English language studies. We alsoaimed to address potential gaps in the review evidence by undertaking searches of recentlypublished primary literature.Another limitation of the review of reviews methodology is the reliance on the reviewers’identification of the relevant studies and their accounts of the designs and findings of theprimary studies. In considering the primary evidence, we used the study design as a proxyfor study quality; however, other factors — for example sample size and recruitment strategy— affect the integrity of a study’s results. The likelihood of having missed primary studies is apossibility for outcomes that core reviews did not specifically set out to examine: weattempted to compensate for this by including the studies identified by supplementary reviews(Palmateer et al., 2010).We have also focused our evaluation of harm reduction programmes on a subset ofinterventions and outcomes. This is not to suggest that other interventions (e.g. educationinformation and counselling) or outcomes (e.g. health and social functioning) that we havenot examined are not important components of these programmes. Additionally, we havefocused on the ‘direct’ evidence of effectiveness of the selected interventions (that is, changesin biological or behavioural outcomes).Implications for harm reduction practice and evaluationIn most European countries, harm reduction interventions developed in response tocommunity-level identified needs, and were often introduced in the absence ofmethodologically rigorous evaluation. We have found the quality of evidence on interventionimpacts to be lacking in some cases, but this is not uncommon for behavioural interventionsin public health more generally and harm reduction interventions in HIV prevention are thesubject of much evaluation research. Our assessment of the quality of evidence does notsuggest that policymakers should disinvest from harm reduction programmes. Rather, theprovision and increase in coverage of interventions needs to be used as an opportunity toconduct better research into the effectiveness of these interventions.147
Harm reduction: evidence, impacts and challenges
Conclusions and recommendationsEuropean countries face a challenge in reducing/maintaining low prevalence of BBVs amongIDUs and reducing drug overdose mortality. Good quality research is fundamental toformulating policy on the development, scale-up and continued investment in public healthinterventions targeting IDUs. We recommend a step change in evaluations of harm reductioninterventions so that future evaluations: (i) include both biological and behavioural outcomesand are powered to detect changes in the outcome of interest; (ii) consider completepackages of harm reduction interventions rather than single interventions; (iii) considerrandomised, especially community-level, designs where possible, and report evaluationfindings to CONSORT and TREND guidelines (Des Jarlais et al., 2004; Moher et al., 2001);(iv) and compare additional interventions or increased coverage/intensity of interventionswith current availability (Palmateer et al., 2010).
ReferencesAbbott, P. J., Weller, S. B., Delaney, H. D. and Moore, B. A. (1998), ‘Community reinforcement approach in thetreatment of opiate addicts’,American Journal of Drug and Alcohol Abuse24 (1), pp. 17–30.Amato, L., Davoli, M., Perucci, C. A., et al. (2005), ‘An overview of systematic reviews of the effectiveness ofopiate maintenance therapies: available evidence to inform clinical practice and research’,Journal of SubstanceAbuse Treatment28, pp. 321–9.Amundsen, E. J., Eskild, A., Stigum, H., Smith, E. and Aalen, O. O. (2003), ‘Legal access to needles andsyringes/needle exchange programmes versus HIV counselling and testing to prevent transmission of HIV amongintravenous drug users: a comparative study of Denmark, Norway and Sweden’,European Journal of Public Health13, pp. 252–8.Avants, S. K., Margolin, A., Kosten, T. R., Rounsaville, B. J. and Schottenfeld, R. S. (1998), ‘When is lesstreatment better? The role of social anxiety in matching methadone patients to psychosocial treatments’,Journal ofConsulting and Clinical Psychology66 (6), pp. 924–31.Baca, C. T. and Grant, K. J. (2005), ‘Take-home naloxone to reduce heroin death’,Addiction100 (12), pp.1823–31.Baker, A., Kochan, N., Dixon, J., Wodak, A. and Heather, N. (1995), ‘HIV risk-taking behaviour among injectingdrug users currently, previously and never enrolled in methadone treatment’,Addiction90 (4), pp. 545–54.Ball, J. C., Lange, W. R., Myers, R. P. and Friedman, S. (1998), ‘Reducing the risk of AIDS through methadonemaintenance treatment’,Journal of Health and Social Behavior29, pp. 214–26.Bargagli, A. M., Hickman, M., Davoli, M., et al. (2006), ‘Drug-related mortality and its impact on adult mortalityin eight European countries’,European Journal of Public Health16 (2), pp. 198–202.Batki, S. L., Sorensen, J. L., Gibson, D. R. and Maude-Griffin, P. (1989), ‘HIV-infected i.v. drug users inmethadone treatment: outcome and psychological correlates: a preliminary report’,NIDA Research Monograph95, pp. 405–6.Bayanzadeh, S. A., et al. (2004), ‘A study of the effectiveness of psychopharmacological intervention in reducingharm/high risk behaviours among substance user prisoners’.
148
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Benninghoff, F. and Dubois-Arber, F. (2002), ‘Résultats de l’étude de la clientèle du Cactus BIEL/BIENNE 2001’,Institut universitaire de médecine sociale et préventive, Lausanne.Benninghoff, F., Solai, S., Huissoud, T. and Dubois-Arber, F. (2003), ‘Evaluation de Quai 9 “Espace d’acceuil etd’injection” à Genéve: période 12/2001–12/2000’, Institut universitaire de médecine sociale et préventive,Lausanne.Best, D., Man, L. H., Zador, D., et al. (2000), ‘Overdosing on opiates: part II — prevention’,Drug and AlcoholFindings(5), pp. 4–18.Bewley-Taylor, D. (2002), ‘Challenging the UN drug control conventions: problems and possibilities’,InternationalJournal of Drug Policy14 (2), pp. 171–9.Bigg, D. (2002), ‘Data on take home naloxone are unclear but not condemnatory’,BMJ324 (7338), p. 678.Bluthenthal, R. N., Kral, A. H., Erringer, E. A. and Edlin, B. R. (1998), ‘Use of an illegal syringe exchange andinjection-related risk behaviors among street-recruited injection drug users in Oakland, California, 1992 to 1995’,Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology18 (5), pp. 505–11.Bluthenthal, R. N., Kral, A. H., Gee, L., Erringer, E. A. and Edlin, B. R. (2000), ‘The effect of syringe exchangeuse on high-risk injection drug users: a cohort study’,AIDS14 (5), pp. 605–11.Boguña, J. (1997), ‘Methadone maintenance programmes’, in O’Brien, O. (ed.),Report of the 3rd EuropeanConference on Drug and HIV/AIDS Services in Prison,Cranstoun Drug Services, London, pp. 68–70.Bravo, M. J., Royuela, L., Brugal, M. T., Barrio, G. and Domingo-Salvany, A. (2009), ‘Use of supervised injectionfacilities and injection risk behaviours among young drug injectors’,Addiction104 (4), pp. 614–19.Broadhead, R. S., van Hulst, Y. and Heckathorn, D. D. (1999), ‘The impact of a needle exchange’s closure’,PublicHealth Reports114, pp. 439–47.Brooner, R., Kidorf, M., King, V., et al. (1998), ‘Drug abuse treatment success among needle exchangeparticipants’,Public Health Reports113 Supplement 1, pp. 129–39.Brugal, M. T., Domingo-Salvany, A., Puig, R., et al. (2005), ‘Evaluating the impact of methadone maintenanceprogrammes on mortality due to overdose and AIDS in a cohort of heroin users in Spain’,Addiction100 (7), pp.981–9.Bruneau, J., Lamothe, F., Franco, E., et al. (1997), ‘High rates of HIV infection among injection drug usersparticipating in needle exchange programs in Montreal: results of a cohort study’,American Journal ofEpidemiology146 (12), pp. 994–1002.Camacho, L. M., Bartholomew, N. G., Joe, G. W., Cloud, M. A. and Simpson, D. D. (1996), ‘Gender, cocaineand during-treatment HIV risk reduction among injection opioid users in methadone maintenance’,Drug andAlcohol Dependence41 (1), pp. 1–7.Caplehorn, J. and Ross, M. (1995), ‘Methadone maintenance and the likelihood of risky needle-sharing’,International Journal of the Addictions30, pp. 685–98.Caplehorn, J., Dalton, M. and Petrenas, A. (1994), ‘Retention in methadone maintenance and heroin addicts’ riskof death’,Addiction89, pp. 203–07.Caplehorn, J., Dalton, M. S., Haldar, F., Petrenas, A. M. and Nisbet, J. G. (1996), ‘Methadone maintenance andaddicts’ risk of fatal heroin overdose’,Substance Use and Misuse31 (2), pp. 177–96.Caslyn, D. A. (1992), ‘Ineffectiveness of AIDS education and HIV antibody testing in reducing high riskbehaviours among injecting drug users’,American Journal of Public Health82, pp. 573–5.
149
Harm reduction: evidence, impacts and challenges
Caslyn, D. A., Saxon, A., Freeman, G. and Whittaker, S. (1991), ‘Needle practices among intravenous drug usersin an area where needle purchase is still legal’,AIDS5, pp. 187–93.Chamot, E., de Saussure, P., Hirschel, B., Deglon, J. J. and Perrin, L. H. (1992), ‘Incidence of hepatitis C, hepatitisB and HIV infections among drug users in a methadone-maintenance programme’,AIDS6 (4), pp. 430–1.Chatham, L. R., Hiller, M. L., Rowan-Szal, G. A., Joe, G. W. and Simpson, D. D. (1999), ‘Gender differences atadmission and follow-up in a sample of methadone maintenance clients’,Substance Use and Misuse34 (8), pp.1137–65.Clausen, T., Anchersen, K. and Waal, H. (2008), ‘Mortality prior to, during and after opioid maintenancetreatment (OMT): a national prospective cross-registry study’,Drug and Alcohol Dependence94, pp. 151–7.Cook, C., Bridge, J. and Stimson, G. V. (2010), ‘The diffusion of harm reduction in Europe and beyond’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Coutinho, R. (2005), ‘Needle exchange: the Amsterdam experience’, inInstitute of Medicine workshop on theprevention of HIV among injecting drug users in high-risk countries,Institute of Medicine Committee on thePrevention of HIV Infection Among Injecting Drug Users in High-Risk Countries, Geneva.Cox, G. M., Lawless, M. C., Cassin, S. P. and Geoghegan, T. W. (2000), ‘Syringe exchanges: a public healthresponse to problem drug use’,Irish Medical Journal93, pp. 143–6.Craine, N., Hickman, M., Parry, J. V., et al. (2009), ‘Incidence of hepatitis C in drug injectors: the role ofhomelessness, opiate substitution treatment, equipment sharing, and community size’,Epidemiology and Infection137 (9), pp. 1255–65.Crofts, N., Nigro, L., Oman, K., Stevenson, E. and Sherman, J. (1997), ‘Methadone maintenance and hepatitis Cvirus infection among injecting drug users’,Addiction92 (8), pp. 999–1005.Cushman, P. J. (1977), ‘Ten years of methadone maintenance treatment: some clinical observations’,AmericanJournal of Drug and Alcohol Abuse4, pp. 543–53.Darke, S. (1988), ‘Self-report among injecting drug users: a review’,Drug and Alcohol Dependence51 (3), pp.253–63.Darke, S. and Hall, W. (1997), ‘The distribution of naloxone to heroin users’,Addiction92 (9), pp. 1195–9.Darke, S. and Hall, W. (2003), ‘Heroin overdose: research and evidence-based intervention’,Journal of UrbanHealth80 (2), pp. 189–200.Darke, S. and Ross, J. (1999), ‘Heroin-related deaths in south western Sydney: 1992–1996’,Drug and AlcoholReview18, pp. 39–45.Darke, S., Ross, J., Zador, D. and Sunjic, S. (2000), ‘Heroin-related deaths in New South Wales, Australia,1992–1996’,Drug and Alcohol Dependence60, pp. 141–50.Davoli, M., Perucci, C. A., Forastiere, F., et al. (1993), ‘Risk factors for overdose mortality: a case control studywithin a cohort of intravenous drug users’,International Journal of Epidemiology22 (2), pp. 272–7.Davoli, M., Bargagli, A. M., Perucci, C. A., et al. (2007), ‘Risk of fatal overdose during and after specialist drugtreatment: the VEdeTTE study, a national multi-site prospective cohort study’,Addiction102 (12), pp. 1954–9.De Jong, W., Tsagarelli, T. and Schouten, E. (1999), ‘Rapid assessment of injection drug use and HIV in theRepublic of Georgia’,Journal of Drug Issues29 (4), pp. 843–60.
150
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Degenhardt, L., Hall, W., Lynskey, M. and Warner-Smith, M. (2004), ‘Illicit drug use’, in Ezzati, M., Lopez, A.,Rodgers, A. and Murray, C. (eds),Comparative quantification of health risks: global and regional burden of diseaseattributable to selected major risk factors,World Health Organization, Geneva.Degenhardt, L., Hall, W. and Warner-Smith, M. (2006), ‘Using cohort studies to estimate mortality amonginjecting drug users that is not attributable to AIDS’,Sexually Transmitted Infections82, pp. 56–63.Degenhardt, L., Randall, D., Hall, W., et al. (2009), ‘Mortality among clients of a state-wide opioidpharmacotherapy program over 20 years: risk factors and lives saved’,Drug and Alcohol Dependence105 (1–2),pp. 9–15.Des Jarlais, D. C., Friedman, S. R., Sotheran, J. L., et al. (1994), ‘Continuity and change within an HIV epidemic:injecting drug users in New York City, 1984 through 1992’,JAMA271 (2), pp. 121–7.Des Jarlais, D. C., Hagan, H., Friedman, S. R., et al. (1995), ‘Maintaining low HIV seroprevalence in populationsof injecting drug users’,JAMA274 (15), pp. 1226–31.Des Jarlais, D. C., Marmor, M., Paone, D., et al. (1996), ‘HIV incidence among injecting drug users in New YorkCity syringe-exchange programmes’,Lancet348 (9033), pp. 987–91.Des Jarlais, C., Perlis, T., Friedman, S. R., et al. (2000), ‘Behavioral risk reduction in a declining HIV epidemic:injection drug users in New York City, 1990–1997’,American Journal of Public Health90 (7), pp. 1112–16.Des Jarlais, D., Lyles, C., Crepaz, N. and TREND Group (2004), ‘Improving the reporting quality ofnonrandomized evaluations of behavioral and public health interventions: the TREND statement’,AmericanJournal of Public Health94 (3), pp. 361–6.Des Jarlais, D. C., Perlis, T., Arasteh, K., et al. (2005a), ‘HIV incidence among injection drug users in New YorkCity, 1990 to 2002: use of serologic test algorithm to assess expansion of HIV prevention services’,AmericanJournal of Public Health95 (8), pp. 1439–44.Des Jarlais, D. C., Perlis, T., Arasteh, K., et al. (2005b), ‘Reductions in hepatitis C virus and HIV infections amonginjecting drug users in New York City, 1990–2001’,AIDS19 (Supplement 3), pp. S20–S25.Dettmer, K., Saunders, B. and Strang, J. (2001), ‘Take home naloxone and the prevention of deaths from opiateoverdose: two pilot schemes’,British Medical Journal322 (7291), pp. 895–6.Dolan, K., Hall, W. and Wodak, A. (1996), ‘Methadone maintenance reduces injecting in prison’,British MedicalJournal312, p. 1162.Dolan, K., Wodak, A. and Hall, W. (1998), ‘Methadone maintenance treatment reduces heroin injection in NSWprisons’,Drug and Alcohol Review17 (2), pp. 153–8.Dolan, K., Rutter, S. and Wodak, A. D. (2003a), ‘Prison-based syringe exchange programmes: a review ofinternational research and development’,Addiction98 (2), pp. 153–8.Dolan, K. A., Shearer, J., MacDonald, M., et al. (2003b), ‘A randomised controlled trial of methadonemaintenance treatment versus wait list control in an Australian prison system’,Drug and Alcohol Dependence72(1), pp. 59–65.Dolan, K. A., Shearer, J., White, B., et al. (2005), ‘Four-year follow-up of imprisoned male heroin users andmethadone treatment: mortality, re-incarceration and hepatitis C infection’,Addiction100 (6), pp. 820–8.Donoghoe, M. C., Stimson, G. V., Dolan, K. and Alldritt, L. (1989), ‘Changes in HIV risk behaviour in clients ofsyringe-exchange schemes in England and Scotland’,AIDS3 (5), pp. 267–72.
151
Harm reduction: evidence, impacts and challenges
Donoghoe, M. C., Dolan, K. and Stimson, G. V. (1992), ‘Life-style factors and social circumstances of syringesharing in injecting drug users’,British Journal of Addiction87, pp. 993–1003.Dubois-Arber, F., Jeannin, A. and Spencer, B. (1999), ‘Evaluation of the AIDS prevention strategy in Switzerland(6th synthesis report 1996–1998)’, Institut universitaire de medicine sociale e preventitive, Lausanne.Ellis, S., Barnett-Page, E., Morgan, A., et al. (2003),HIV prevention: a review of reviews assessing the effectivenessof interventions to reduce the risk of sexual transmission,Health Development Agency, London.EMCDDA (2008),The state of the drugs problem in Europe: annual report 2008,European Monitoring Centre forDrugs and Drug Addiction, Lisbon.EMCDDA (2009),The state of the drugs problem in Europe: annual report 2009,European Monitoring Centre forDrugs and Drug Addiction, Lisbon.Emmanuelli, J. and Desenclos, J. C. (2005), ‘Harm reduction interventions, behaviours and associated healthoutcomes in France, 1996–2003’,Addiction100 (11), pp. 1690–700.European Commission (2007),Report from the Commission to the European Parliament and the Council on theimplementation of the Council recommendation of 18 June 2003 on the prevention and reduction of health-relatedharm associated with drug dependence,COM (2007) 199 final, Commission of the European Communities,Brussels.Faggiano, F., Vigna-Taglianti, F., Versino, E. and Lemma, P. (2003), ‘Methadone maintenance at different dosagesfor opioid dependence’,Cochrane Database of Systematic Reviews3, p. CD002208.Frischer, M. and Elliott, L. (1993), ‘Discriminating needle exchange attenders from non-attenders’,Addiction88(5), pp. 681–7.Fugelstad, A., Rajs, J., Böttiger, M. and Gerhardsson de Verdier, M. (1995), ‘Mortality among HIV-infectedintravenous drug addicts in Stockholm in relation to methadone treatment’,Addiction90 (5), pp. 711–16.Galea, S., Worthington, N., Piper, T. M., et al. (2006), ‘Provision of naloxone to injection drug users as anoverdose prevention strategy: early evidence from a pilot study in New York City’,Addictive Behaviors31 (5), pp.907–12.Gearing, F. R. and Schweitzer, M. D. (1974), ‘An epidemiologic evaluation of long term methadone maintenancetreatment for heroin addiction’,American Journal of Epidemiology100, pp. 101–12.Gibson, D. R., Flynn, N. M. and Perales, D. (2001), ‘Effectiveness of syringe exchange programs in reducing HIVrisk behavior and HIV seroconversion among injecting drug users’,AIDS15 (11), pp. 1329–41.Gibson, D. R., Brand, R., Anderson, K., et al. (2002), ‘Two- to sixfold decreased odds of HIV risk behaviorassociated with use of syringe exchange’,Journal of Acquired Immune Deficiency Syndromes31 (2), pp. 237–42.Glaziou, P. and Heneghan, C. (2009), ‘A spotter’s guide to study designs’,Evidence Based Medicine14, pp. 37–8.Gleghorn, A. A., Jones, T. S., Doherty, M. C., Celentano, D. D. and Vlahov, D. (1995), ‘Acquisition and use ofneedles and syringes by injecting drug users in Baltimore, Maryland’,Journal of Acquired Immune DeficiencySyndromes and Human Retrovirology10 (1), pp. 97–103.Gleghorn, A. A., Wright-De Aguero, L. and Flynn, C. (1998), ‘Feasibility of one-time use of sterile syringes: astudy of active injection drug users in seven United States metropolitan areas’,Journal of Acquired ImmuneDeficiency Syndromes and Human Retrovirology18 (Supplement 1), pp. S30–S36.Goldberg, D., Cameron, S. and McMenamin, J. (1998), ‘Hepatitis C virus antibody prevalence among injectingdrug users in Glasgow has fallen but remains high’,Communicable Disease and Public Health1 (2), pp. 95–7.
152
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Goldberg, D., Burns, S., Taylor, A., et al. (2001), ‘Trends in HCV prevalence among injecting drug users inGlasgow and Edinburgh during the era of needle/syringe exchange’,Scandinavian Journal of Infectious Diseases33 (6), pp. 457–61.Goldstein, M. F., Friedman, S. R., Neaigus, A., et al. (1995), ‘Self-reports of HIV risk behavior by injecting drugusers: are they reliable?’Addiction90 (8), pp. 1097–104.Gossop, M., Marsden, J., Stewart, D. and Rolfe, A. (2000), ‘Patterns of improvement after methadone treatment:1 year follow-up results from the National Treatment Outcome Research Study’,Drug and Alcohol Dependence60(3), pp. 275–86.Gowing, L., Farrell, M., Bornemann, R., Sullivan, L. and Ali, R. (2008), ‘Substitution treatment of injecting opioidusers for prevention of HIV infection’,Cochrane Database of Systematic Reviews(2), DOI: 10.1002/14651858.CD004145.pub3.Green, T. C., Heimer, R. and Grau, L. E. (2008), ‘Distinguishing signs of opioid overdose and indication fornaloxone: an evaluation of six overdose training and naloxone distribution programs in the United States’,Addiction103 (6), pp. 979–89.Greenfield, L., Bigelow, G. E. and Brooner, R. (1995), ‘Validity of intravenous drug abusers’ self-reported changesin HIV high-risk drug use behaviors’,Drug and Alcohol Dependence39 (2), pp. 91–98.Grella, C. E., Anglin, M. D., Rawson, R., Crowley, R. and Hasson, A. (1996), ‘What happens when ademonstration project ends: consequences for a clinic and its clients’,Journal of Substance Abuse Treatment13 (3),pp. 249–56.Gronbladh, L., Ohlund, L. S. and Gunne, L. M. (1990), ‘Mortality in heroin addiction: impact of methadonetreatment’,Acta Psychiatrica Scandinavica82, pp. 22–37.Groseclose, S. L., Weinstein, B., Jones, T. S., et al. (1995), ‘Impact of increased legal access to needles andsyringes on practices of injecting-drug users and police officers: Connecticut, 1992–1993’,Journal of AcquiredImmune Deficiency Syndromes and Human Retrovirology10 (1), pp. 82–9.Gunne, L. M. and Gronbladh, L. (1981), ‘The Swedish methadone maintenance program: a controlled study’,Drug and Alcohol Dependence7, pp. 249–56.Guydish, J., Clark, G., Garcia, D. and Bucardo, J. (1995), ‘Evaluation of needle exchange using street-basedsurvey methods’,Journal of Drug Issues25, pp. 33–41.Guydish, J., Bucardo, J., Clark, G. and Bernheim, S. (1998), ‘Evaluating needle exchange: a description of clientcharacteristics, health status, program utilization, and HIV risk behavior’,Substance Use and Misuse33 (5), pp.1173–96.Hagan, H. and Thiede, H. (2000), ‘Changes in injection risk behavior associated with participation in the Seattleneedle-exchange program’,Journal of Urban Health77 (3), pp. 369–82.Hagan, H., Des Jarlais, D. C., Purchase, D., et al. (1993), ‘An interview study of participants in the Tacoma,Washington, syringe exchange’,Addiction88 (12), pp. 1691–7.Hagan, H., Des Jarlais, D. C. and Friedman, S. (1994),Risk for human immunodeficiency virus and hepatitis B virusin users of the Tacoma syringe exchange program,National Academy Press, Washington, DC.Hagan, H., Des Jarlais, D. C., Friedman, S. R., Purchase, D. and Alter, M. J. (1995), ‘Reduced risk of hepatitis Band hepatitis C among injection drug users in the Tacoma syringe exchange program’,American Journal of PublicHealth85 (11), pp. 1531–7.
153
Harm reduction: evidence, impacts and challenges
Hagan, H., McGough, J. P., Thiede, H., et al. (1999), ‘Syringe exchange and risk of infection with hepatitis B andC viruses’,American Journal of Epidemiology149 (3), pp. 203–13.Hagan, H., Thiede, H. and Des Jarlais, D. C. (2004), ‘Hepatitis C virus infection among injection drug users:survival analysis of time to seroconversion’,Epidemiology15 (5), pp. 543–9.Hall, W. and Kimber, J. (2005), ‘Being realistic about benefits of supervised injecting facilities’,Lancet366(9482), pp. 271–2.Hallinan, R., Byrne, A., Amin, J. and Dore, G. J. (2004), ‘Hepatitis C virus incidence among injecting drug userson opioid replacement therapy’,Australian and New Zealand Journal of Public Health28 (6), pp. 576–8.Hammett, T. M., Kling, R., Johnston, P., et al. (2006), ‘Patterns of HIV prevalence and HIV risk behaviors amonginjection drug users prior to and 24 months following implementation of cross-border HIV prevention interventionsin northern Vietnam and southern China’,AIDS Education and Prevention18 (2), pp. 97–115.Hart, G. J., Carvell, A. L., Woodward, N., et al. (1989), ‘Evaluation of needle exchange in central London:behaviour change and anti-HIV status over one year’,AIDS3 (5),pp. 261–5.Hartel, D. M. and Schoenbaum, E. (1998), ‘Methadone treatment protects against HIV infections: two decades ofexperience in the Bronx, New York City’,Public Health Reports113 (Supplement 1), pp. S107–S115.Hartgers, C., Buning, E. C., van Santen, G. W., Verster, A. D. and Coutinho, R. A. (1989), ‘The impact of theneedle and syringe-exchange programme in Amsterdam on injecting risk behaviour’,AIDS3 (9), pp. 571–6.Hartgers, C., van Ameijden, E. J., van den Hoek, J. A. and Coutinho, R. A. (1992), ‘Needle sharing andparticipation in the Amsterdam Syringe Exchange program among HIV-seronegative injecting drug users’,PublicHealth Reports107 (6), pp. 675–81.Health Outcomes International, National Centre in HIV Epidemiology & Clinical Research and Drummond, M.(2002),Return on investment in needle & syringe programs,Commonwealth Department of Health and Aging,Canberra.Hedrich, D. (2004),European report on drug consumption rooms,European Monitoring Centre for Drugs and DrugAddiction, Lisbon.Hedrich, D., Kerr, T. and Dubois-Arber, F. (2010), ‘Drug consumption facilities in Europe and beyond’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Heimer, R., Cantani, H., Newman, R. G., Zambrano, J., Brunet, A. and Ortiz, A. (2006), ‘Methadonemaintenance in prison: evaluation of a pilot program in Puerto Rico’,Drug and Alcohol Dependence83 (2), pp.122–9.Heimer, R., Kaplan, E. H., Khoshnood, K., Jariwala, B. and Cadman, E. C. (1993), ‘Needle exchange decreasesthe prevalence of HIV-1 proviral DNA in returned syringes in New Haven, Connecticut’,American Journal ofMedicine95 (2), pp. 214–20.Heimer, R., Khoshnood, K., Bigg, D., Guydish, J. and Junge, B. (1998), ‘Syringe use and reuse: effects of syringeexchange programs in four cities’,Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology18(Supplement 1), pp. S37–S44.Heimer, R. , Zambrano, J. A., Brunet, A. et al. (2005), ‘Methadone maintenance treatment in a men’s prison inPuerto Rico: a pilot program’,Journal of Correctional Healthcare11 (3), pp. 295–305.
154
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Heinemann, A. and Gross, U. (2001), ‘Prevention of blood-borne virus infections among drug users in an openprison by syringe vending machines’,Sucht47 (2), pp. 57–65.Hernandez-Aguado, I., Ramos-Rincon, J. M., Avinio, M. J., et al. (2001), ‘Measures to reduce HIV infection havenot been successful to reduce the prevalence of HCV in intravenous drug users’,European Journal of Epidemiology17 (6), pp. 539–44.Hunter, G. M., Donoghoe, M. C., Stimson, G. V., Rhodes, T. and Chalmers, C. P. (1995), ‘Changes in theinjecting risk behaviour of injecting drug users in London, 1990–1993’,AIDS9 (5), pp. 493–501.Huo, D., Bailey, S. L., Garfein, R. S. and Ouellet, L. J. (2005), ‘Changes in the sharing of drug injectionequipment among street-recruited injection drug users in Chicago, Illinois, 1994–1996’,Substance Use and Misuse40 (1), pp. 63–76.Hurley, S. F., Jolley, D. J. and Kaldor, J. M. (1997), ‘Effectiveness of needle-exchange programmes for preventionof HIV infection’,Lancet349 (9068), pp. 1797–800.Hutchinson, S. J., McIntyre, P. G., Molyneaux, P., et al. (2002), ‘Prevalence of hepatitis C among injectors inScotland 1989–2000: declining trends among young injectors halt in the late 1990s’,Epidemiology and Infection128 (3), pp. 473–7.Iguchi, M. Y. (1998), ‘Drug abuse treatment as HIV prevention: changes in social drug use patterns might alsoreduce risk’,Journal of Addictive Diseases17 (4), pp. 9–18.Ingold, F. R. and Ingold, S. (1989), ‘The effects of the liberalization of syringe sales on the behavior ofintravenous drug users in France’,Bulletin on Narcotics41, pp. 67–81.Islam, M. M. and Conigrave, K. M. (2007), ‘Assessing the role of syringe dispensing machines and mobile vanoutlets in reaching hard-to-reach and high-risk groups of injecting drug users (IDUs): a review’,Harm ReductionJournal4 (14), DOI: 10.1186/1477-7517-4-14.Jacob, J. and Stöver, H. (1997), ‘Clean needles for Saxon prisoners’,Prison ReportSpring, pp. 22–3.Jacob, J. and Stöver, H. (2000), ‘Drug use, drug control, and drug services in German prisons: contradictions,insufficiencies and innovative approaches’, in Shewan, D. and Davies, J. (eds),Drug use and prisons: aninternational perspective,Overseas Publishers Association, Amsterdam, pp. 57–87.Jacob, J., Rottman, J. and Stöver, H. (1999),Entstehung und Praxis eines Gesundheitsraumangebotes fürDrogenkonsumierende. Abschlußbericht der einjährigen Evaluation des ‘drop-in Fixpunkt’, Hannover,Bibliotheks undInformationssystem der Universität Oldenburg, Oldenburg.Jones, L., Pickering, L., Sumnall, H., McVeigh, J. and Bellis, M. A. (2008),A review of the effectiveness and cost-effectiveness of needle and syringe programmes for injecting drug users,Centre for Public Health, John MooresUniversity, Liverpool.Käll , K., Hermansson, U., Amundsen, E. J. and Ronnback, S. (2007), ‘The effectiveness of needle exchangeprogrammes for HIV prevention: a critical review’,Journal of Global Drug Policy and Practice1. Available athttp://www.globaldrugpolicy.org/1/3/1.php (accessed 20 October 2009).Keene, J., Stimson, G. V., Jones, S. and Parry-Langdon, N. (1993), ‘Evaluation of syringe-exchange for HIVprevention among injecting drug users in rural and urban areas of Wales’,Addiction88 (8), pp. 1063–70.Kelly, M., Swann, C., Killoran, A., et al. (2002),Methodological problems in constructing the evidence base inpublic health,Health Development Agency, London.Kerr, T., Tyndall, M., Li, K., Montaner, J. and Wood, E. (2005), ‘Safer injection facility use and syringe sharing ininjection drug users’,Lancet366 (9482), pp. 316–18.
155
Harm reduction: evidence, impacts and challenges
Kerr, T., Kimber, J., De Beck, K. and Wood, E. (2007), ‘The role of safer injection facilities in the response to HIV/AIDS among injection drug users’,Current HIV Reports4, pp. 158–64.Kimber, J., Dolan, K., van Beek, I., Hedrich, D. and Zurhold, H. (2003), ‘Drug consumption facilities: an updatesince 2000’,Drug and Alcohol Review22, pp. 227–33.King, V. L., Kidorf, M. S., Stoller, K. B. and Brooner, R. K. (2000), ‘Influence of psychiatric comorbidity on HIVrisk behaviors: changes during drug abuse treatment’,Journal of Addictive Diseases19 (4), pp. 65–83.Klee, H. and Morris, J. (1995), ‘The role of needle exchanges in modifying sharing behaviour: cross-studycomparisons 1989–1993’,Addiction90 (12), pp. 1635–45.Klee, H., Faugier, J., Hayes, C. and Morris, J. (1991), ‘The sharing of injecting equipment among drug usersattending prescribing clinics and those using needle-exchanges’,British Journal of Addiction86, pp. 217–23.Kwiatkowski, C. F. and Booth, R. E. (2001), ‘Methadone maintenance as HIV risk reduction with street-recruitedinjecting drug users’,Journal of Acquired Immune Deficiency Syndromes26 (5), pp. 483–9.Lamden, K. H., Kennedy, N., Beeching, N. J., et al. (1998), ‘Hepatitis B and hepatitis C virus infections: riskfactors among drug users in northwest England’,Journal of Infection37 (3), pp. 260–9.Linssen, L., de Jong, W. and Wolf, J. (2000),Gebruiksruimten: Een systematisch overzicht van de voorziening en deeffecten ervan,Trimbos-Instituut, ontwikkelcentrum Social Verslavingsbeleid, Utrecht.Ljungberg, B., Christensson, B., Tunving, K., et al. (1991), ‘HIV prevention among injecting drug users: three yearsof experience from a syringe exchange program in Sweden’,Journal of Acquired Immune Deficiency Syndromes4(9), pp. 890–5.Longshore, D., Hsieh, S., Danila, B. and Anglin, M. D. (1993), ‘Methadone maintenance and syringe sharing’,International Journal of the Addictions29, pp. 983–96.Longshore, D., Bluthenthal, R. N. and Stein, M. D. (2001), ‘Needle exchange program attendance and injectionrisk in Providence, Rhode Island’,AIDS Education and Prevention13 (1), pp. 78–90.Lott, D., Strain, E. C., Brooner, R., Bigelow, G. and Johnson, R. (2006), ‘HIV risk behaviours duringpharmacologic treatment for opioid dependence: a comparison of levomethadyl acetate hydrochloride,buprenorphine, and methadone’,Journal of Substance Abuse Treatment31 (2), pp. 187–94.Lurie, P. (1997), ‘Invited commentary: le mystere de Montreal’,American Journal of Epidemiology146 (12), pp.1003–6; discussion pp. 1007–10.McAuley, A., Lindsay, G., Woods, M. and Louttit, D. (2009), ‘Responsible management and use of a personaltake-home naloxone supply: a pilot project’,Drugs: Education Prevention and Policy,DOI:10.1080/09687630802530712.MacDonald, M. A., Wodak, A. D., Dolan, K. A., et al. (2000), ‘Hepatitis C virus antibody prevalence amonginjecting drug users at selected needle and syringe programs in Australia, 1995–1997: collaboration ofAustralian NSPs’,Medical Journal of Australia172 (2), pp. 57–61.MacDonald, M., Law, M. G., Kaldor, J. M., Hales, J. and Dore, G. J. (2003), ‘Effectiveness of needle and syringeprogrammes for preventing HIV transmission’,International Journal of Drug Policy14 (5–6), pp. 353–7.McGregor, C., Ali, R., Lokan, R., Christie, P. and Darke, S. (2002), ‘Accidental fatalities among heroin users inSouth Australia, 1994–1997: toxicological findings and circumstances of death’,Addiction Research and Theory,pp. 335–46.
156
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Magura, S., Siddiqui, Q., Shapiro, J., et al. (1991), ‘Outcomes of an AIDS prevention program for methadonepatients’,International Journal of the Addictions26 (6), pp. 629–55.Magura, S., Nwakeze, P. and Demsky, S. (1998), ‘Pre-and in-treatment predictors of retention in methadonetreatment using survival analysis’,Addiction93 (1), pp. 51–60.Maher, L., Jalaludin, B., Chant, K. G., et al. (2006), ‘Incidence and risk factors for hepatitis C seroconversion ininjecting drug users in Australia’,Addiction101 (10), pp. 1499–508.Mansson, A. S., Moestrup, T., Nordenfelt, E. and Widell, A. (2000), ‘Continued transmission of hepatitis B and Cviruses, but no transmission of human immunodeficiency virus among intravenous drug users participating in asyringe/needle exchange program’,Scandinavian Journal of Infectious Diseases32 (3), pp. 253–8.Margolin, A., Avants, S. K., Warburton, L. A., Hawkins, K. A. and Shi, J. (2003), ‘A randomized clinical trial of amanual-guided risk reduction intervention for HIV-positive injection drug users’,Health Psychology22 (2), pp. 223–8.Mark, H. D., Nanda, J., Davis-Vogel, A., et al. (2006), ‘Profiles of self-reported HIV-risk behaviours amonginjection drug users in methadone maintenance treatment, detoxification, and needle exchange programs’,PublicHealth Nursing23 (1), pp. 11–19.Marsch, L. A., Bickel, W. K., Badger, G. J. and Jacobs, E. A. (2005), ‘Buprenorphine treatment for opioiddependence: the relative efficacy of daily, twice and thrice weekly dosing’,Drug and Alcohol Dependence77 (2),pp. 195–204.Mathers, B. M., Degenhardt, L., Wiessing, L., et al. (2008), ‘Global epidemiology of injecting drug use and HIVamong people who inject drugs: a systematic review’,Lancet372 (9651), pp. 1733–45.Maxwell, S., Bigg, D., Stanczykiewicz, K. and Carlberg-Racich, S. (2006), ‘Prescribing naloxone to activelyinjecting heroin users: a program to reduce heroin overdose deaths’,Journal of Addictive Diseases25 (3), pp.89–96.Meandzija, B., O’Connor, P. G., Fitzgerald, B., Rounsaville, B. J. and Kosten, T. R. (1994), ‘HIV infection andcocaine use in methadone maintained and untreated intravenous drug users’,Drug and Alcohol Dependence36(2), pp. 109–13.Meijer, G., de Jong, A., Koeter, M. and Bieleman, B. (2001),Gebruik van de straat: Evaluatie gebruiksruimtebinnenstad-Zuid Groningen,INTRAVAL, Groningen-Rotterdam.Metzger, D. S., Woody, G. E., McLellan, A. T., et al. (1993), ‘Human immunodeficiency virus seroconversionamong intravenous drug users in- and out-of-treatment: an 18-month prospective follow-up’,Journal of AcquiredImmune Deficiency Syndromes6 (9), pp. 1049–56.Meyeno, C., Zulaica, D. and Parras, F. (2000), ‘Prisons: needle exchange programmes in prisons in Spain’,Canadian HIV/AIDS Policy & Law Newsletter5, pp. 20–21.Miller, C. L., Wood, E., Spittal, P. M., et al. (2004), ‘The future face of coinfection: prevalence and incidence ofHIV and hepatitis C virus coinfection among young injection drug users’,Journal of Acquired Immune DeficiencySyndromes36 (2), pp. 743–9.Milloy, M. and Wood, E. (2009), ‘Emerging role of supervised injecting facilities in human immunodeficiencyvirus prevention’,Addiction104 (4), pp. 620–1.Millson, P., Myers, T., Calzavara, L., et al. (2003), ‘Regional variation in HIV prevalence and risk behaviours inOntario injection drug users (IDU)’,Canadian Journal of Public Health94, pp. 431–5.Minder Nejedly, M. and Bürki, C. M. (1996),Monitoring HIV risk behaviours in a street agency with injection roomin Switzerland,Medizinischen Fakultät, Universität Bern, Bern.
157
Harm reduction: evidence, impacts and challenges
Moher, D., Schulz, K., Altman, D. and CONSORT Group (2001), ‘The CONSORT statement: revisedrecommendations for improving the quality of reports of parallel-group randomised trials’,Lancet357 pp. 1191–4.Monterroso, E. R., Hamburger, M. E., Vlahov, D., et al. (2000), ‘Prevention of HIV infection in street-recruitedinjection drug users: the Collaborative Injection Drug User Study (CIDUS)’,Journal of Acquired Immune DeficiencySyndromes25 (1), pp. 63–70.Moss, A. R., Vranizan, K., Gorter, R., et al. (1994), ‘HIV seroconversion in intravenous drug users in SanFrancisco, 1985–1990’,AIDS8 (2), pp. 223–31.MSIC Evaluation Committee (2003),Final report of the evaluation of the Sydney Medically Supervised InjectingCentre,University of New South Wales, Sydney.National Treatment Agency (2009), ‘Life saving kits to be given to families of injecting drug users ingroundbreaking scheme’. Available at http://www.nta.nhs.uk/media/media_releases/2009_media_releases/life_saving_kits_to_be_given_to_families_of_injecting_drug_users.aspx.Nelles, J., Dobler-Mikola, A. and Kaufmann, B. (1997), ‘Provision of syringes and prescription of heroin in prison:the Swiss experience in the prisons of Hindelbank and Oberschongrun,’ in Nelles, J. and Fuhrer, A. (eds),Harmreduction in prison,Peter Lang, Bern, pp. 239–62.Nelson, K. E., Vlahov, D., Cohn, S., et al. (1991), ‘Human immunodeficiency virus infection in diabetic intravenousdrug users’,JAMA266 (16), pp. 2259–61.Novick, D. M., Joseph, H., Croxson, T. S., et al. (1990), ‘Absence of antibody to human immunodeficiency virus inlong-term, socially rehabilitated methadone maintenance patients’,Archives of Internal Medicine150, pp. 97–9.Obadia, Y., Feronia, I., Perrin, V., Vlahov, D., and Moatti, J. P. (1999), ‘Syringe vending machines for injectiondrug users: an experiment in Marseille, France’,American Journal of Public Health89 (12), pp. 1852–4.Oliver, K. J., Maynard, H., Friedman, S. R. and Des Jarlais, D. C. (1994), ‘Behavioral and community impact ofthe Portland Syringe Exchange Program’, paper presented at the Proceedings of a Workshop on NeedleExchange and Bleach Distribution Programs, Washington, DC.Ouellet, L., Huo, D. and Bailey, S. L. (2004), ‘HIV risk practices among needle exchange users and nonusers inChicago’,Journal of Acquired Immune Deficiency Syndromes37 (1), pp. 1187–96.Palmateer, N., Kimber, J., Hickman, M., et al. (2008),Evidence for the effectiveness of harm reduction interventionsin preventing hepatitis C transmission among injecting drug users,Prevention Working Groups of the AdvisoryCouncil on the Misuse of Drugs and the Hepatitis C Action Plan for Scotland, Glasgow.Palmateer, N., Kimber, J., Hickman, M., et al. (2010), ‘Evidence for the effectiveness of sterile injecting equipmentprovision in preventing hepatitis C and HIV transmission among injecting drug users: a review of reviews’,Addiction ,DOI:10.1111/j.1360-0443.2009.02888.x.Paone, D., Des Jarlais, D. C., Caloir, S., et al. (1994), ‘New York City syringe exchange: an overview’, paperpresented at the Proceedings of a Workshop on Needle Exchange and Bleach Distribution Programs,Washington, DC.Parmar, M. (2008), ‘NALoxone InVEstigation (N-ALIVE) pilot randomised controlled trial (RCT)’. Available athttp://www.controlled-trials.com/ISRCTN34044390/.Patrick, D. M., Strathdee, S. A., Archibald, C. P., et al. (1997), ‘Determinants of HIV seroconversion in injection drugusers during a period of rising prevalence in Vancouver’,International Journal of STD & AIDS8 (7), pp. 437–45.Patrick, D. M., Tyndall, M. W., Cornelisse, P. G., et al. (2001), ‘Incidence of hepatitis C virus infection amonginjection drug users during an outbreak of HIV infection’,Canadian Medical Association Journal165 (7), pp. 889–95.
158
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Peak, A., Rana, S., Maharjan, S. H., Jolley, D. and Crofts, N. (1995), ‘Declining risk for HIV among injecting drugusers in Kathmandu, Nepal: the impact of a harm-reduction programme’,AIDS9 (9), pp. 1067–70.Petticrew, M. (2009), ‘Systematic reviews in public health: old chestnuts and new challenges’,Bulletin of the WorldHealth Organization87 (3), pp. 163–163A.Piper, T. M., Stancliff, S., Rudenstine, S., et al. (2008), ‘Evaluation of a naloxone distribution and administrationprogram in New York City’,Substance Use and Misuse43 (7), pp. 858–70.Poschadel, S., Höger, R., Schnitzler, J. and Schreckenberger, D. (2003),Evaluation der Arbeit derDrogenkonsumräume in der Bundesrepublik Deutschland: Endbericht im Auftrag des Bundesministeriums fürGesundheit,Nomos-Verlags-Gesellschaft, Baden-Baden.Poser, W., Koc, J. and Ehrenreich, H. (1995), ‘Methadone maintenance treatment’,British Medical Journal310,pp. 463.Pouget, E. R., Deren, S., Fuller, C. M., et al. (2005), ‘Receptive syringe sharing among injection drug users inHarlem and the Bronx during the New York State Expanded Syringe Access Demonstration Program’,Journal ofAcquired Immune Deficiency Syndromes39 (4), pp. 471–7.Power, R. and Nozhkina, N. (2002), ‘The value of process evaluation in sustaining HIV harm reduction in theRussian Federation’,AIDS16 (2), pp. 303–04.Reitox (2008), ‘National reports to the EMCDDA on new developments, trends and in-depth information onselected issues’, EMCDDA. Available at http://www.emcdda.europa.eu/publications/searchresults?action=list&type=PUBLICATIONS&SERIES_PUB=w203.Reyes Fuentes, V. C. (2003),15 Jahre Fixerraum Bern. Auswirkungen auf soziale und medizinische Aspekte beiDrogenabhängigen,University of Bern, Bern.Rezza, G., Sagliocca, L., Zaccarelli, M., et al. (1996), ‘Incidence rate and risk factors for HCV seroconversionamong injecting drug users in an area with low HIV seroprevalence’,Scandinavian Journal of Infectious Diseases28 (1), pp. 27–9.Rhoades, H., Creson, D., Elk, R., Schmitz, J. and Grabowski, J. (1998), ‘Retention, HIV risk, and illicit drug useduring treatment: methadone dose and visit frequency’,American Journal of Public Health88, pp. 34–9.Richard, A. J., Mosier, V. and Atkinson, J. S. (2002), ‘New syringe acquisition and multi-person use of syringesamong illegal drug users’,Journal of Public Health Policy23 (3), pp. 324–43.Ronco, C., Spuhler, G., Coda, P. and Schopfer, R. (1996), ‘Evaluation der Gassenzimmer I, II und III in Basel’,Sozial und Praventivmedizin41, pp. S58–S68.Roy, E., Alary, M., Morissette, C., et al. (2007), ‘High hepatitis C virus prevalence and incidence amongCanadian intravenous drug users’,International Journal of STD and AIDS18 (1), pp. 23–7.Sackett, D. L., Rosenberg, J., Muir Gray, J. A., Haynes, R. B. and Richardson, W. S. (1996), ‘Evidence basedmedicine: what it is and what it isn’t’,British Medical Journal312, pp. 71–2.Sarkar, K., Mitra, S., Bal, B., Chakraborty, S. and Bhattacharya, S. K. (2003), ‘Rapid spread of hepatitis C andneedle exchange programme in Kolkata, India’,Lancet361 (9365), pp. 1301–2.Saxon, A., Calsyn, D. and Jackson, T. (1994), ‘Longitudinal changes in injection behaviors in a cohort of injectiondrug users’,Addiction89, pp. 191–202.Schechter, M. T., Strathdee, S. A., Cornelisse, P. G., et al. (1999), ‘Do needle exchange programmes increase thespread of HIV among injection drug users? An investigation of the Vancouver outbreak’,AIDS13 (6), pp. F45–51.
159
Harm reduction: evidence, impacts and challenges
Schoenbaum, E. E., Hartel, D. M. and Gourevitch, M. N. (1996), ‘Needle exchange use among a cohort ofinjecting drug users’,AIDS10 (14), pp. 1729–34.Schroeder, J., Epstein, D., Umbricht, A. and Preston, K. (2006), ‘Changes in HIV risk behaviours among patientsreceiving combined pharmacological and behavioral interventions for heroin and cocaine dependence’,Addictive Behaviors31 (5), pp. 868–79.Seal, K. H., Thawley, R., Gee, L., et al. (2005), ‘Naloxone distribution and cardiopulmonary resuscitation trainingfor injection drug users to prevent heroin overdose death: a pilot intervention study’,Journal of Urban Health82(2), pp. 303–11.Sees, K. L., Delucchi, K. L., Masson, C., et al. (2000), ‘Methadone maintenance vs 180-day psychosociallyenriched detoxification for treatment of opioid dependence: a randomized controlled trial’,JAMA283 (10), pp.1303–10.Selvey, L. A., Denton, M. and Plant, A. J. (1997), ‘Incidence and prevalence of hepatitis C among clients of aBrisbane methadone clinic: factors influencing hepatitis C serostatus’,Australian and New Zealand Journal ofPublic Health21 (1), pp. 102–04.Serpelloni, G., Carrieri, M. P., Rezza, G., et al. (1994), ‘Methadone treatment as a determinant of HIV riskreduction among injecting drug users: a nested case-control study’,AIDS Care6 (2), pp. 215–20.Sherman, S. G., Gann, D. S., Tobin, K. E., et al. (2009), ‘“The life they save may be mine”: diffusion of overdoseprevention information from a city sponsored programme’,International Journal of Drug Policy20 (2), pp. 137–42.Shore, R., Marmor, M., Titus, S. and Des Jarlais, D. (1996), ‘Methadone maintenance and other factorsassociated with intraindividual temporal trends in injection drug use’,Journal of Substance Abuse Treatment13,pp. 241–8.Simpson, D. D., Joe, G. W., Rowan-Szal, G. and Greener, J. (1995), ‘Client engagement and change during drugabuse treatment’,Journal of Substance Abuse7 (1), pp. 117–34.Singer, M., Himmelgreen, D., Weeks, M. R., Radda, K. E. and Martinez, R. (1997), ‘Changing the environment ofAIDS risk: findings on syringe exchange and pharmacy sales of syringes in Hartford, CT’,Medical Anthropology18 (1), pp. 107–30.Small, D. (2007), ‘Fools rush in where angels fear to tread: playing God with Vancouver’s supervised injectionfacility in the political borderland’,International Journal of Drug Policy18 (1), pp. 18–26.Smyth, B. P., Keenan, E. and O’Connor, J. J. (1999), ‘Evaluation of the impact of Dublin’s expanded harmreduction programme on prevalence of hepatitis C among short-term injecting drug users’,Journal of Epidemiologyand Community Health53 (7), pp. 434–5.Somaini, B., Wang, J. and Persozo, M. (2000), ‘A continuing concern: HIV and hepatitis testing and prevalenceamong drug users in substitution programmes in Switzerland’,AIDS Care12, pp. 449–60.Sorensen, J. L. and Copeland, A. L. (2000), ‘Drug abuse treatment as an HIV prevention strategy: a review’,Drugand Alcohol Dependence59 (1), pp. 17–31.Sporer, K. A. (2003), ‘Strategies for preventing heroin overdose’,British Medical Journal326 (7386), pp.442–44.Stallwitz, A. and Stöver, H. (2007), ‘The impact of substitution treatment in prisons: a literature review’,International Journal Drug Policy18 (6), pp. 464–74.
160
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Stark, K., Herrmann, U., Ehrhardt, S. and Bienzle, U. (2006), ‘A syringe exchange programme in prison asprevention strategy against HIV infection and hepatitis B and C in Berlin, Germany’,Epidemiology and Infection134 (4), pp. 814–19.Stark, K., Muller, R., Bienzle, U. and Guggenmoos-Holzmann, I. (1996), ‘Methadone maintenance treatment andHIV risk-taking behaviour among injecting drug users in Berlin’,Journal of Epidemiology and Community Health50(5), pp. 534–7.Stevens, A., Stöver, H. and Brentari, C. (2010), ‘Criminal justice approaches to harm reduction in Europe’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Stoltz, J. A., Wood, E., Small, W., et al. (2007), ‘Changes in injecting practices associated with the use of amedically supervised safer injection facility’,Journal of Public Health (Oxford)29 (1), pp. 35–9.Stöver, H. and Nelles, J. (2003), ‘Ten years of experience with needle and syringe exchange programmes inEuropean prisons’,International Journal of Drug Policy14 (5–6), pp. 437–44.Strang, J., Marsden, J., Cummins, M., et al. (2000), ‘Randomized trial of supervised injectable versus oralmethadone maintenance: report of feasibility and 6-month outcome’,Addiction95 (11), pp. 1631–45.Strang, J., Manning, V., Mayet, S., et al. (2008), ‘Overdose training and take-home naloxone for opiate users:prospective cohort study of impact on knowledge and attitudes and subsequent management of overdoses’,Addiction103 (10), pp. 1648–57.Strathdee, S. A., Patrick, D. M., Currie, S. L., et al. (1997), ‘Needle exchange is not enough: lessons from theVancouver injecting drug use study’,AIDS11 (8), pp. F59–65.Taylor, A., Goldberg, D., Hutchinson, S., et al. (2000), ‘Prevalence of hepatitis C virus infection among injectingdrug users in Glasgow 1990–1996: are current harm reduction strategies working?’Journal of Infection40 (2),pp. 176–83.Teeson, M., Ross, J., Darke, S., et al. (2006), ‘One year outcomes for heroin dependence: findings from theAustralian Treatment Outcome Study (ATOS)’,Drug and Alcohol Dependence83 (2), pp. 174–80.Thiede, H., Hagan, H. and Murrill, C. S. (2000), ‘Methadone treatment and HIV and hepatitis B and C riskreduction among injectors in the Seattle area’,Journal of Urban Health77 (3), pp. 331–45.Tilson, H., Aramrattana, A., Bozzette, S., et al. (2007), ‘Preventing HIV infection among injecting drug users inhigh risk countries: an assessment of the evidence’,Institute of Medicine,Washington, DC.Tobin, K. E., Sherman, S., Beilenson, P., Welsh, C. and Latkin, C. A. (2009), ‘Evaluation of the Staying Aliveprogramme: training injection drug users to properly administer naloxone and save lives’,International Journal ofDrug Policy20 (2), pp. 131–6.Valente, T., Foreman, R. K., Junge, B. and Vlahov, D. (2001), ‘Needle-exchange participation effectiveness andpolicy: syringe relay, gender, and the paradox of public health’,Journal of Urban Health78, pp. 340–9.van Ameijden, E. J. and Coutinho, R. A. (1998), ‘Maximum impact of HIV prevention measures targeted atinjecting drug users’,AIDS12 (6), pp. 625–33.van Ameijden, E. J., van den Hoek, J. A., van Haastrecht, H. J. and Coutinho, R. A. (1992), ‘The harm reductionapproach and risk factors for human immunodeficiency virus (HIV) seroconversion in injecting drug users,Amsterdam’,American Journal of Epidemiology136 (2), pp. 236–43.
161
Harm reduction: evidence, impacts and challenges
van Ameijden, E. J., van den Hoek, J. A., Mientjes, G. H. and Coutinho, R. A. (1993), ‘A longitudinal study on theincidence and transmission patterns of HIV, HBV and HCV infection among drug users in Amsterdam’,EuropeanJournal of Epidemiology9 (3), pp. 255–62.van Ameijden, E. J., van den Hoek, A. R. and Coutinho, R. A. (1994), ‘Injecting risk behavior among drug usersin Amsterdam, 1986 to 1992, and its relationship to AIDS prevention programs’,American Journal of Public Health84 (2), pp. 275–81.van Ameijden, E. J., Langendam, M. W. and Coutinho, R. A. (1999), ‘Dose-effect relationship between overdosemortality and prescribed methadone dosage in low-threshold maintenance programs’,Addictive Behaviours24(4), pp. 559–63.van den Berg, C., Smit, C., van Brussel, G., Coutinho, R. A. and Prins, M. (2007), ‘Full participation in harmreduction programmes is associated with decreased risk for human immunodeficiency virus and hepatitis C virus:evidence from the Amsterdam Cohort Studies among drug users’,Addiction102, pp. 1454–62.van den Hoek, J. A., van Haastrecht, H. J. and Coutinho, R. A. (1989), ‘Risk reduction among intravenous drugusers in Amsterdam under the influence of AIDS’,American Journal of Public Health79 (10), pp. 1355–7.van der Poel, A., Barendregt, C. and van de Mheen, D. (2003), ‘Drug consumption rooms in Rotterdam: anexplorative description’,European Addiction Research9, pp. 94–100.Vazirian, M., Nassirimanesh, B., Zamani, S., et al. (2005), ‘Needle and syringe sharing practices of injectingdrug users participating in an outreach HIV prevention program in Tehran, Iran: a cross-sectional study’,HarmReduction Journal2, p. 19.Vertefeuille, J., Marx, M. A., Waimar, T., et al. (2000), ‘Decline in self-reported high-risk injection-relatedbehaviors among HIV-seropositive participants in the Baltimore needle exchange program’,AIDS and Behavior4(4), pp. 381–8.Vickerman, P., Hickman, M., Rhodes, T. and Watts, C. (2006), ‘Model projections on the required coverage ofsyringe distribution to prevent HIV epidemics among injecting drug users’,Journal of Acquired Immune DeficiencySyndromes42 (3), pp. 355–61.Villaneuva, M. G. (2002), ‘Programa de Intercambia de Jeringuillas en el Centre Penitenciario de Pamplona’,RevEsp Sanid Penit4, pp. 18–23.Vlahov, D., Junge, B., Brookmeyer, R., et al. (1997), ‘Reductions in high-risk drug use behaviors amongparticipants in the Baltimore needle exchange program’,Journal of Acquired Immune Deficiency Syndromes andHuman Retrovirology16 (5), pp. 400–06.Wagner, K., Valente, T., Casanova, M., et al. (in press), ‘Evaluation of an overdose prevention and responsetraining programme for injection drug users in the Skid Row area of Los Angeles, CA’,International Journal ofDrug Policy,DOI: 10.1016/j.drugpo.2009.01.003.Ward, J., Mattick, R. P. and Hall, W. (1997),Methadone maintenance treatment and other opioid replacementtherapies,Harwood Academic Press, Amsterdam.Watters, J. (1994), ‘Syringe and needle exchange as HIV/AIDS prevention for injecting drug users’,Journal of theAmerican Medical Association271, pp. 115–20.WHO (World Health Organization) (2007),Guide to starting and managing needle and syringe programmes,World Health Organization, Geneva.WHO, UNAIDS (Joint United Nations Programme on HIV/AIDS) and UNODC (United Nations Office on Drugsand Crime) (2007),Effectiveness of interventions to manage HIV in prisons: opioid substitution therapies and otherdrug dependence treatment,WHO, Geneva.
162
Chapter 5: Harm reduction among injecting drug users — evidence of effectiveness
Williams, A. B., McNelly, E. A., Williams, A. E. and D’Aquila, R. T. (1992), ‘Methadone maintenance treatmentand HIV type 1 seroconversion among injecting drug users’,AIDS Care4 (1), pp. 35–41.Wodak, A. and Cooney, A. (2004),Effectiveness of sterile needle and syringe programming in reducing HIV/AIDSamong injecting drug users,WHO, Geneva.Wodak, A. and Cooney, A. (2006), ‘Do needle syringe programs reduce HIV infection among injecting drugusers? A comprehensive review of the international evidence’,Substance Use and Misuse41 (6–7), pp. 777–813.Wood, E., Tyndall, M. W., Spittal, P. M., et al. (2002), ‘Factors associated with persistent high-risk syringesharing in the presence of an established needle exchange programme’,AIDS16 (6), pp. 941–3.Wood, E., Kerr, T., Spittal, P. M., et al. (2003), ‘An external evaluation of a peer-run “unsanctioned” syringeexchange program’,Journal of Urban Health80 (3), pp. 455–64.Wood, E., Tyndall, M., Stoltz, J., et al. (2005), ‘Factors associated with syringe sharing among users of amedically supervised safer injecting facility’,American Journal of Infectious Diseases1 (1), pp. 50–4.Wood, E., Tyndall, M., Montaner, J., and Kerr, T. (2006), ‘Summary of findings from the evaluation of a pilotmedically supervised safer injecting facility’,Canadian Medical Association Journal175 (11), pp. 1399–404.Wright, N. M. J. and Tompkins, C. N. E. (2006), ‘A review of the evidence for the effectiveness of primaryprevention interventions for hepatitis C among injecting drug users’,Harm Reduction Journal3 (27), DOI:10.1186/1477-7517-3-27.Yancovitz, S., Des Jarlais, D., Peskoe-Peyser, N., et al. (1991), ‘A randomised trial of an interim methadonemaintenance clinic’,American Journal of Public Health81, pp. 1185–91.Zador, D., Sunjic, S. and Darke, S. (1996), ‘Heroin related deaths in New South Wales in 1992: toxicologicalfindings and circumstances’,Medical Journal of Australia164, pp. 204–07.Zurhold, H., Kreuzfeld, N., Degwitz, P. and Verthein, U. (2001),Drogenkonsumräume: Gesundheitsförderung undMinderung öffentlicher Belastungen in europäischen Grossstädten,Lambertus, Freiburg.
163
Chapter 6The effect of epidemiological setting on the impactof harm reduction targeting injecting drug usersPeter Vickerman and Matthew Hickman
AbstractHepatitis C (HCV) and HIV cause substantial morbidity and mortality, and are both easilytransmitted through contaminated syringes. Although reducing the transmission of HCV andHIV through injecting drug use is critical to preventing both infections, there is little evidencethat interventions targeting injecting drug users (IDUs) reduce the transmission of either HIVor HCV.A recent systematic review suggested a strong positive relationship between the prevalenceof HIV and HCV in different IDU populations, but with considerable variability in differentsettings. This analysis uses a dynamic HIV and HCV transmission model to investigate thepossible reasons for these observed trends, and to explore whether HIV and/or HCVprevalence could be used as proxy markers for the relative impact of an IDU intervention indifferent settings. By varying the HIV and HCV transmission probabilities and other non-setting specific HIV/HCV natural history parameters, a dynamic compartmental model of HIVand HCV transmission was fitted, to observe trends in HIV and HCV prevalence fromdifferent settings. Using multivariate linear regression, the output from the ‘best-fitting’simulated epidemics was used to identify factors that determine the type of HIV and HCVepidemic that occurs. These simulated epidemics were then used to project the impact of ageneric intervention that reduced syringe sharing amongst all IDUs or just low- or high-riskIDUs, and to explore whether the impact projections correlated with HIV and/or HCVprevalence.Results showed that the relative HCV to HIV transmission probability was the main factordetermining how well the model agreed with the observed HIV and HCV prevalencetrends. The ‘best-fitting’ model projections suggest that the relative HIV to HCV prevalencein different epidemic scenarios is positively correlated to the relative proportion of andlevel of risk behaviour among the high-risk IDUs. Indeed, the projected impact of thegeneric intervention was also strongly correlated with the baseline HIV and HCVprevalence of the simulated epidemic, with more impact (HIV/HCV infections averted andrelative decrease in HIV/HCV incidence) occurring in higher HCV prevalence settings butless impact occurring, except for HIV infections averted, in higher baseline HIV prevalencesettings. Lastly, a generic intervention among IDUs had less impact on the HCV epidemiccompared to the HIV epidemic in most scenarios. However, when the intervention reachedonly lower-risk IDUs, it had only little impact on the HIV epidemic and greater impact onthe HCV epidemic.165
Harm reduction: evidence, impacts and challenges
We conclude that the trends and variability in HIV and HCV prevalence observed in differentepidemiological settings may be mainly due to differences in the heterogeneity of IDU riskbehaviour. The HIV and HCV prevalence in a setting could be proxy markers for the relativeimpact of an intervention.Keywords:injecting drug use, HIV, hepatitis C, mathematical modelling.
IntroductionHepatitis C (HCV) and HIV cause substantial morbidity and mortality. Worldwide, 40 millionpeople are estimated to be infected with HIV (UNAIDS, 2004a) and 170 million with HCV(WHO, 2000a). HCV and HIV can easily be transmitted through contaminated syringes(Baggaley et al., 2006; De Carli et al., 2003), and, while HIV infection rates vary widely(UNAIDS, 2004b), HCV infection rates are often very high amongst injecting drug users(IDUs) (Health Protection Agency, 2004; Wiessing and Nardone, 2006). Similarly to HIV,HCV infection is an important public health concern in Europe and elsewhere, because themajority of HCV infections do not resolve (Micallef et al., 2006) but become chronic and overtime lead to cirrhosis of the liver, and possibly liver cancer and death (Limburg, 2004).A worldwide systematic ecological analysis by the authors has shown that there is a strongpositive relationship between the prevalence of HIV and that of HCV in different IDUpopulations, with the mean HIV prevalence generally being negligible if HCV prevalence isless than 30 % and thereafter increasing linearly with HCV prevalence (Vickerman et al.,2009a). Although this suggests that HCV prevalence could be used as a proxy indicator forinjection-related HIV risk, there was substantial variability around the relationship when HCVprevalence is greater than 30 %, suggesting that other factors, such as the stage of the HIVepidemic and heterogeneity in IDU risk behaviour, may also play a role. This variability inHIV and HCV prevalence exists in all world regions, with the HIV prevalence in differentEuropean settings varying between 0 % and 70 % (Muga et al., 2007) and the HCVprevalence varying between 2.8 % (Danis et al., 2007) and 98 % (Westh et al., 1993).Overall, HIV prevalence in Europe is low; with high rates of prevalence being found in localstudies. Nonetheless, despite this variability, the systematic review suggests that HCVprevalence could be used as a proxy indicator for injection-related HIV risk — and as atarget or threshold level to minimise the possibility of an HIV outbreak.Modelling health harm and its reductionReducing the transmission of HCV and HIV through injecting drug use is critical to the overallprevention of these infections in most countries. Epidemiological studies have shown thatneedle exchange and opioid substitution therapy (OST) interventions can reduce HIVtransmission (Gibson et al., 1999; Gibson et al., 2001). However, the evidence forinterventions impacting on HCV transmission is modest (Des Jarlais et al., 2005; Goldberg etal., 2001; van den Berg et al., 2007), with only one European study showing that full harmreduction (syringe distribution and OST) can reduce not only HIV incidence by 57 %, but alsoHCV incidence by 64 % (van den Berg et al., 2007). This lack of evidence is partly due to a166
Chapter 6: The effect of epidemiological setting on the impact of harm reduction targeting injecting drug users
relative dearth of epidemiological studies that estimate the impact of IDU interventions onHCV incidence, probably due to their high cost and difficulties in following up ‘chaotic’ IDUs(Craine et al., 2009). Although it is not the gold standard for evaluating interventions,modelling can play an important role in these difficult situations by translating intermediateintervention outcomes (HIV/HCV prevalence trends and/or even decreases in IDU riskbehaviour) into projected decreases in HIV/HCV incidence or number of infections averted.Indeed, modelling can also answer ‘what if’ questions that would otherwise be very difficultto answer with epidemiological studies.Numerous model analyses have provided important insights into the potential impact and cost-effectiveness of different intervention strategies for IDUs in Europe, the United States, EasternEurope, Asia and Australia (Blower et al., 1991; Kaplan and Heimer, 1994; Kretzschmar andWiessing, 1998; Kretzschmar and Wiessing, 2008; Murray et al., 2003; Vickerman et al.,2006b; Vickerman et al., 2007). However, most studies have focused on HIV, with the smallnumber of HCV modelling analyses being hampered by simplified epidemiology of HCV orIDU risk behaviour, or uncertainty surrounding key behavioural or biological parameters(Kretzschmar and Wiessing, 2004; Murray et al., 2003; Pollack, 2001; Vickerman et al., 2007).Despite this, a number of analyses have fit HCV models to epidemiological data from onesetting (Hutchinson et al., 2006; Murray et al., 2003; Vickerman et al., 2007; Vickerman etal., 2009b), mainly to estimate the impact of changes in syringe distribution/sharing.However, this model fitting strategy may not adequately calibrate an HCV transmissionmodel, because one epidemic profile will contain insufficient information to fully understandthe nature of HCV epidemics in other settings. This was emphasised in two studies by the firstauthor of this chapter, which found that very different model parameterisations couldaccurately fit the HCV prevalence data from London, United Kingdom (Vickerman et al.,2007) or Rawalpindi, Pakistan (Vickerman et al., 2009b).Few epidemiological or modelling analyses have considered the impact on the transmissionof both HIV and HCV of an intervention targeting IDUs (Kwon et al., 2009; Murray et al.,2003; Vickerman et al., 2009b), and none have explored how impact could vary by theextent of baseline HIV and HCV epidemic occurring in a setting. In an attempt to fill thisknowledge gap and to reduce the parametric uncertainty around modelling HCV, thisanalysis uses a joint HIV and HCV transmission mathematical model, fitted to the observedtrends between HIV and HCV prevalence, to explore how the impact of a genericintervention (any one that reduces the extent of syringe sharing among IDUs) varies acrossdifferent epidemiological scenarios. The model’s biological parameters are calibrated bydetermining which set of ‘biological parameters’ (HIV and HCV transmission and naturalhistory parameters) most accurately produces the observed relationship between HIV andHCV prevalence when IDU behavioural parameters are widely varied to produce differentepidemics. The simulated epidemics for this ‘biological’ parameter set are then used toexplore how the impact of a generic intervention varies by HIV and HCV prevalence. Morecomplex ‘realistic’ interventions (i.e., combinations of interventions, including treatment) werenot modelled because it was not the main focus of the study, but impact estimates were madeamongst high- and low-frequency syringe sharers in order to understand how targeted IDUinterventions may differentially impact on HIV and HCV.167
Harm reduction: evidence, impacts and challenges
MethodsThere were a number of stages to this analysis, many of which built on the work of previousanalyses. First, the HIV and HCV transmission mathematical model and different ‘biological’parameter sets (includes HIV and HCV transmission probabilities and non-setting specificnatural history parameters — see Table 6.1 for all ‘biological’ parameters) that producedmodel fits in a recent modelling analysis from a specific IDU population (Vickerman et al.,2009b) were used as the basis for this analysis. For each of the biological parameter sets, anextensive uncertainty analysis was undertaken by randomly sampling specific IDU riskbehaviour parameters (see parameters in Table 6.1) to produce 100 different behaviouralparameter sets and so 100 different simulated HCV and HIV epidemics. These 100behavioural parameter sets were chosen so that a wide variety of simulated HIV and HCVepidemics would be produced, and the same behavioural parameter sets were used for eachbiological parameter set. For each parameter set, the simulated epidemic was run until theoverall HCV prevalence among IDUs was stable and the HIV epidemic had run for 30 years.The projected HIV/HCV prevalences were then compared to HIV and HCV prevalence trendsfor different IDU populations from a systematic review to see which biological parameter setproduced the highest proportion of HIV and HCV epidemic projections lying within a definedarea containing the vast majority of the paired HIV and HCV prevalence estimates from thesystematic review. The 100 runs for this ‘best fit’ biological parameter set were used toexplore how the impact of reducing the frequency of syringe sharing by 50 %, eitheramongst all IDUs or just among low-frequency (sharing syringes less often than once a week)or high-frequency (sharing syringes at least once a week) syringe sharers, varies forepidemics with different endemic HIV and HCV prevalence. Intervention impact wasestimated over three years in terms of HIV and HCV infections averted (per 1 000 IDUs) andthe relative decrease in HIV and HCV incidence (defined as the decrease of HIV and,respectively, HCV incidence compared to the baseline incidence).
Table 6.1:Uncertainty ranges used for ‘biological’ (HIV and HCV) and behaviouralmodel parametersModel parameterHIV ‘biological’ model parameterHIV transmission probability per syringesharing eventCofactor increase in HIV transmissionprobability during initial period of highviraemiaPre-AIDS period of high viraemiaDuration of initial period of high viraemiaDuration of pre-AIDS period of highviraemia0.14–1.41 %7.5–15(Baggaley et al., 2006)(Pilcher et al., 2004a; Quinn etal., 2000; Wawer et al., 2005)(Wawer et al., 2005)
Value used
Data source
3–6
1.5–2.5 months (Pilcher et al., 2004b; Wawer etal., 2005)(Wawer et al., 2005)12–24 months
168
Chapter 6: The effect of epidemiological setting on the impact of harm reduction targeting injecting drug users
Table 6.1(continued)Model parameterMedian duration until severe morbidity ordeathHCV ‘biological’ model parameterHCV transmission probability if HIVnegativeHCV transmission probability if HIVpositive relative to if HIV negative1.5–14 %RR of 1.0–3.7(Baggaley et al., 2006; De Carli etal., 2003; Vickerman et al., 2009b)(De Carli et al., 2003;Pappalardo, 2003; Vickerman etal., 2009b; Yazdanpanah et al.,2005)(Cox et al., 2005; Larghi et al.,2002; Vickerman et al., 2007)
Value used75–92 months
Data source(Grover and Shivraj, 2004;Kumarasamy et al., 2003)
Duration of HCV acute phase of infectionProportion of HCV infecteds that resolveinfectionAmongst HIV negativesAmongst HIV positives relative to HIVnegativesProportion of resolved infecteds thatbecome immuneAmongst HIV negatives
3–24 months
26 % (20–50 %) (Micallef et al., 2006)RR of 0.21–0.58(Bonacini et al., 2001; Daar et al.,2001; Grebely et al., 2008;Thomas et al., 2000a)
0–100 %
(Currie et al., 2008; Dalgard,2005; Grebely et al., 2006; Mehtaet al., 2002; Micallef et al., 2007)Little data (Grebely et al., 2006;Mehta et al., 2002)
Amongst HIV positives relative to HIVnegativesEffectiveness of cleaning syringes fordisinfecting against HCV (mainly waterused)Behavioural model parametersDuration inject drugs forProportion do not share syringesFrequency of syringe sharing per monthamongst high-frequency syringe sharersFrequency of syringe sharing per monthamongst low-frequency syringe sharersProportion of IDUs that share with highfrequencyProportion of IDUs that share with lowfrequency
RR of 0.3–0.5
Assumed same Little data (Kapadia et al., 2002).effectiveness asHIV
5–15 years0–40 %4–60<4 (less thanonce per week)5–60 %remainder
NANANANANANA
169
Harm reduction: evidence, impacts and challenges
Model derivationA deterministic compartmental model of HCV and HIV transmission developed for apreviously published analysis was used (Vickerman et al., 2009b). In brief, the modelsimulates the transmission of both HCV and HIV amongst IDUs with different levels of needle/syringe sharing. The model includes three behavioural subgroups of IDUs depending onwhether they do not share needles/syringes (do not inject with a previously used needle/syringe), or share with a low or high frequency. The model simulates the transmission ofHCV/HIV over time and includes two sub-groups for those that are new injectors and thosethat have been injecting for longer. IDUs leave the population if they cease injecting, die orexperience severe HIV-related morbidity.The HCV transmission model assumes that IDUs enter an acute phase of infection onceinfected, and either resolve their infection after a number of months or progress to lifelongchronic infection. A proportion of those that resolve HCV are assumed to become immune,and the remainder become susceptible again (Aitken et al., 2008; Currie et al., 2008;Dalgard, 2005; Grebely et al., 2006; Micallef et al., 2007). All infecteds develop anantibody response during their acute phase.The HIV transmission model assumes that once susceptible individuals are infected theyprogress to a high viraemia phase of infection, following which they progress to a longerstage of low viraemia, a short period of high viraemia pre-AIDS, and then AIDS. Because thefocus of the study was to look at the impact of interventions aiming to reduce injecting risks,the model did not simulate the sexual transmission of HIV.The HCV and HIV models are run in parallel once the HCV transmission model hasreached a stable state without HIV. From that point, the model follows the HIV/HCV co-infection state of each IDU and assumes that being HIV infected exacerbates the effects ofbeing HCV infected, both in terms of the secondary transmission and the natural history ofHCV. Because of evidence that HIV infection increases both the HCV viral load in co-infected IDUs (Bonacini et al., 2001; Daar et al., 2001; Fishbein et al., 2006; Thomas et al.,2000b; Thomas et al., 2001) and the probability of mother-to-child HCV transmission(Pappalardo, 2003), the HCV secondary transmission probability was assumed to beheightened in HIV/HCV co-infected IDUs. In addition, it was assumed that the probabilitythat an HCV infection resolves was reduced in HIV/HCV co-infected individuals (Bonaciniet al., 2001; Daar et al., 2001; Grebely et al., 2007; Mehta et al., 2002; Thomas et al.,2000a), and so was the probability that they develop immunity against HCV (Grebely etal., 2006; Mehta et al., 2002).This HIV/HCV prevalence model also has an additional component that incorporates thepossible effect of a generic intervention. After a certain time the intervention reduces thefrequency of syringe sharing amongst IDUs, regardless of whether they share syringes with alow or high frequency, and affects the epidemiology of HIV and HCV in the modelledpopulation.170
Chapter 6: The effect of epidemiological setting on the impact of harm reduction targeting injecting drug users
Model parameter values used for model fittingThe model was parameterised using different biological parameter sets that producedmodel fits (n=42) to HIV and HCV prevalence data from a specific IDU population(Vickerman et al., 2009b). These parameter sets were obtained during a rigorous fittingprocess that also sampled across the uncertainty ranges for the behavioural parametersfrom that setting. The behavioural parameters were mainly obtained from an in-depthsurvey undertaken in the setting. The 42 biological model parameter sets were from atotal of 400 non-setting specific parameter sets that were randomly sampled fromparameter uncertainty ranges during the model fitting process. The parameter uncertaintyranges for the biological parameters were obtained from the literature, and included suchaspects as the HIV and HCV transmission probabilities, the duration of the HCV acutephase, and proportion of HCV infecteds that resolve infection. See Table 6.1 for thebiological parameters and their uncertainty ranges. All parameters had similar rangesamongst the model fits from the previous analysis, except for the HIV and HCVtransmission probabilities, which had the ranges of 0.34–1.4 % and 1.5–5.0 %,respectively.One hundred behavioural parameter sets were randomly sampled from the behaviouralparameter uncertainty ranges in Table 6.1, and these parameter sets were used toFigure 6.1:Weighted HIV and HCV prevalence data from 310 different IDU populations includingthe defined region for determining whether a model simulation is a model fit or not
100What proportion of endemicmodel projections are withinthis region?
75HIV prevalence (%)
50
25
00255075100
HCV prevalence (%)DataModel fit region
171
Harm reduction: evidence, impacts and challenges
simulate 100 different HIV and HCV epidemics for each biological parameter set. Eachepidemic was run until the HCV prevalence changed by <0.05 % in one year and thenthe HIV epidemic was run for 30 years. The ranges for each behavioural parameterwere set to allow the model to produce a wide range of different HIV and HCVepidemics.For each biological parameter set, the 100 model simulations were compared againstcollated HIV and HCV prevalence data from different IDU cross-sectional surveys foundby our systematic review (Vickerman et. al, 2009a) (see Figure 6.1). This systematic reviewobtained weighted HIV and HCV prevalence estimates for 310 different IDU populationsfrom peer reviewed journal articles, international AIDS conference abstracts between2000–08, the European IDU HIV/HCV database (managed by the European MonitoringCentre for Drugs and Drug Addiction) (EMCDDA, 2008), United Kingdom unlinkedprevalence monitoring programme (managed by the Health Protection Agency) (HealthProtection Agency, 2008), and WHO Multi-City Drug Injection Study Phase II (WHO,2000b). A model simulation was defined as a fit to the collated HIV/HCV prevalence dataif the last time point of the model simulation projected an HIV and HCV prevalence withinthe region surrounded by a bolded triangle shown in Figure 6.1. The percentage of modelruns that were model fits for a particular biological parameter set was used to evaluate itsgoodness of fit. The model projections for the best-fitting biological parameter set werealso validated against available HIV and HCV incidence data from different IDUpopulations (obtained through a non-systematic literature review) to confirm that themodel produced a similar relationship between HIV/HCV incidence and HIV/HCVprevalence.Intervention impact projectionsThe biological parameter set with the best goodness of fit was used to explore how theimpact of a 50 % reduction in the frequency of syringe sharing will vary by endemic HIV andHCV prevalence in different epidemic settings. A 50 % reduction in syringe sharing waschosen for illustrative purposes, but this figure also reflects an upper bound estimate for whatcan be achieved with intensive needle and syringe distribution (Foss et al., 2007; Hutchinsonet al., 2006). The impact of the intervention was estimated in terms of HIV/HCV infectionsaverted (per 1 000 IDUs) and the relative decrease in HIV/HCV incidence over three years.Scatter plots, partial correlation coefficients and linear regression models (with ‘impact’ asthe independent variable and HIV and HCV prevalence as the dependent variables) wereused to assess the relationship between the variables, and the R-squared statistic was used todetermine the strength of the association.
Insights from model fitting processThe percentage of model simulations for each biological parameter set that gave endemicHIV and HCV prevalence projections within the bounded area in Figure 6.1 varied widelyfrom 0 % to 78 %. Interestingly, the goodness of fit was largely dependent on the factor172
Chapter 6: The effect of epidemiological setting on the impact of harm reduction targeting injecting drug users
difference between the HIV and HCV transmission rate (defined asΩ),with a greaterpercentage of simulations lying within the bounded area asΩincreases (Figure 6.2). Thissuggests that the HCV transmission probability must be over three, or potentially even four tofive times greater than the HIV transmission probability. Figure 6.2 also shows that onebiological parameter set had a much better goodness of fit than the others, with 78 % of themodel projections within the bounded area compared to 54 % for the next best-fittingbiological parameter set. This biological parameter set was defined as the ‘best fit’ and wasused in the impact analysis.
Figure 6.2:Relationship between the factor difference in the HCV and HIV transmissionprobabilities and the percentage of model simulations that lie within the bounded areain Figure 6.1
% of endemic HVI/HCV prevalence projectionswithin bounded model fit area
100
75
50
25
0012345Factor difference between HCV and HIV transmission probability /0
A comparison of available HIV/HCV prevalence and incidence data with the modelprojections from the best-fitting biological parameter set is shown in Figures 6.3a and b. Theyshow that the model mimics the data reasonably well, except for settings with high HCVprevalence but low HIV prevalence, that is, a low ratio of HIV prevalence to HCV prevalence.This could be due to the model not incorporating enough heterogeneity in risk behaviour, orHIV being more compartmentalised in specific IDU networks, or just the fact that we onlyincluded the final time point of the model’s projection of HIV and HCV prevalence for eachepidemic in the comparison. Including all the model projections over time for each epidemicresults in many more lower HIV prevalence projections (result not shown), and the existingmodel projections also suggest that decreasing the proportion and/or syringe sharingfrequency of the high-frequency syringe sharers results in a lower HIV prevalence relative toHCV prevalence (Figure 6.4).173
Harm reduction: evidence, impacts and challenges
Figure 6.3:Comparison with data of the HIV/HCV prevalence and incidence projections for the‘best fit’ biological parameter setFigure 6.3a:Comparison with HIV/HCV prevalence data100
HIV prevalence (%)
75
50
25
00255075100
HCV prevalence (%)DataModel fit regionBest fit model projections
Figure 6.3b:Comparison with HIV/HCV incidence data
HIV incidence per 100 person years
100
75
50
25
00255075100
HCV incidence per 100 person yearsDataBest fit model projections
174
Chapter 6: The effect of epidemiological setting on the impact of harm reduction targeting injecting drug users
Figure 6.4a:Relationship between relative HIV to HCV prevalence and the proportion of high-risksyringe-sharing IDUs1.00Ratio of HIV to HCV prevalence
0.75
0.50
0.25
0.00010203040506070
% of IDUs in the high-risk syringe sharing groupFigure 6.4b:Relationship between relative HIV to HCV prevalence and syringe-sharing frequency ofhigh-risk syringe-sharing IDUs1.00Ratio of HIV to HCV prevalence
0.75
0.50
0.25
0.00010203040506070
Frequency of syringe sharing in high-risk syringe sharing group per month
Intervention impact projections: overall projectionsFigure 6.5 shows that the projected HIV and HCV infections averted due to a 50 % reductionin syringe sharing frequency amongst all IDUs is highly variable, although a similar range of175
Harm reduction: evidence, impacts and challenges
impact projections are obtained for each infection. The number of HIV infections averted ispositively correlated with baseline HIV and HCV prevalence and the number of HCVinfections averted is negatively correlated with baseline HIV prevalence, but positivelycorrelated with baseline HCV prevalence. These correlations are maintained when the partialcorrelation coefficients are estimated (see Table 6.2), while controlling for the prevalence ofthe other infection, with the corresponding linear regression models explaining 50–60 %(R2=0.5–0.6) of the variance in the model projections.Figure 6.5a:Scatter plot to show the relationship between HIV infections averted (per 1 000 IDUs)and HIV prevalence200180160HIV infections averted140120100806040200020406080100Baseline HIV prevalence (%)Figure 6.5b:Scatter plot to show the relationship between HIV infections averted (per 1 000 IDUs)and HCV prevalence200180HIV infections averted160140120100806040200020406080100Baseline HCV prevalence (%)
176
Chapter 6: The effect of epidemiological setting on the impact of harm reduction targeting injecting drug users
Figure 6.5c:Relationship between HCV infections averted (per 1 000 IDUs) and HIV prevalence200180HCV infections averted160140120100806040200020406080100
Baseline HIV prevalence (%)
Figure 6.5d:Relationship between HCV infections averted (per 1 000 IDUs) and HCV prevalence
200180HCV infections averted160140120100806040200020406080100
Baseline HCV prevalence (%)
177
Harm reduction: evidence, impacts and challenges
Table 6.2:Partial correlation coefficients and regression parameters for the
relationship between two different measures of intervention impact (HIVand HCV infections averted or relative decrease in HIV and HCVincidence) and baseline HIV and HCV prevalencePartial correlation † withHCVprevalenceHIVprevalence0.35↑–0.74↓–0.73↓–0.93↓
Linear regressioncoefficient † withHCVHIVprevalence prevalence73.0↑235.7↑0.81↑0.98↑77.3↑–222.5↓–1.15↓–1.17↓
R20.500.600.530.87
Infectionsaverted
HIV
0.33↑
HCV 0.76↑
Relative decrease HIV 0.60↑in incidenceHCV 0.91↑Notes:
† all partial correlation coefficients and regression coefficients are significant to p<0.001.↑signifies a positive correlation with that variable and↓signifies a negative correlation with that variable.
Similar associations are seen for the relative decrease in HIV or HCV incidence due to theintervention, with both being positively correlated with baseline HCV prevalence andnegatively correlated with baseline HIV prevalence. However, although the regression modelfor the relative decrease in HIV incidence has a similar R2, the regression model for therelative decrease in HCV incidence is a much better fit, explaining 87 % of the variance. Thebox below explains the implications of these results.
Implications of regression coefficients relating intervention impact projections to baselineHIV and HCV prevalenceFor every 10 % increase in baseline HIV prevalence:• he post-intervention reduction in HIV and HCV incidence decreases by ~12 %;t• he number of HIV infections averted over three years increases by ~8 per 1 000 IDUs treached (which translates to a 10–14 % increase in the number of HIV infections averted ifthe baseline HIV prevalence was 20 %);• he number of HCV infections averted over three years decreases by ~22 per 1 000 IDUs t(which translates to a 33–50 % decrease if the baseline HCV prevalence was 50 %).For every 10 % increase in baseline HCV prevalence:• he post-intervention reduction in HIV incidence increases by 8 % and that of HCV incidence tby 10 %;• he number of HIV infections averted over three years increases by ~7 per 1 000 IDUs treached (which translates to a 10–14 % increase in the number of HIV infections averted ifHIV prevalence was 20 %);• he number of HCV infections averted increases by about ~24 per 1 000 IDUs (which Ttranslates to a 33–50 % increase if the baseline HCV prevalence was 50 %).
178
Chapter 6: The effect of epidemiological setting on the impact of harm reduction targeting injecting drug users
The existence of these associations is due to the relative HIV prevalence (compared toHCV) being a measure of the proportion and syringe sharing frequency of the high-riskIDUs (Figure 6.4). To attain high HIV prevalence, a larger proportion of IDUs whofrequently share syringes is necessary, and so it becomes harder to avert HCV infectionsand reduce the HIV and HCV incidence because IDUs become re-infected frequently. Thiseffect is not observed in the HIV infections averted because the force of infection (therate at which susceptible individuals become infected) for HIV is much lower than that forHCV, with the reduced impact on HIV incidence being offset by the higher baseline HIVincidence.Figure 6.6 suggests that the relative HIV prevalence could be a good predictor of the relativenumber of HIV vs. HCV infections averted by an intervention. For example, if HIV prevalenceis 25 % of HCV prevalence then the model suggests that 40–60 % fewer HIV than HCVinfections will be averted, whereas if HIV prevalence is 75 % of HCV prevalence then >50 %more HIV than HCV infections will be averted.These results occur because the relative HIV to HCV prevalence in a stable epidemic is ameasure of relative proportion and level of risk behaviour of the high-risk IDUs. For a lowrelative HIV prevalence to HCV prevalence, the IDU population must have a smaller and/or‘less risky’ high-risk group with lower HIV incidence, and so fewer HIV cases but more HCVcases are averted because fewer of the HCV incident infections are amongst very high-riskIDUs with a high re-infection rate. For a high relative HIV prevalence, the IDU populationmust have a larger and/or ‘more risky’ high-risk group with higher HIV incidence, and somore HIV cases but fewer HCV cases are averted because more HCV incident infections areamongst the high-risk IDUs that frequently get re-infected.Figure 6.6:The model’s projected relationship between the relative HIV prevalence compared toHCV prevalence and the relative number of HIV infections averted compared to HCVinfections averted250200150100500020406080100Relative HIV prevalence compared to HCV prevalence (%)Below line – more HCV infections averted
Relative HIV infections avertedcompared to HCV infections averted (%)
Above line – more HIV infections averted
179
Harm reduction: evidence, impacts and challenges
Intervention impact projections: effect of targeting IDUsFigure 6.7 shows that the targeting of an intervention among IDUs to only those IDUs thathave a low- or high-frequency of syringe sharing could have substantial implications for theimpact of an intervention. If the intervention just reaches the higher-risk IDUs then a greaterimpact on HIV transmission can be expected, whereas if the intervention just reaches thelower-risk IDUs then a much greater impact on HCV transmission should be expected.Indeed, little to no decrease in HIV incidence should be expected in this latter case becausemost HIV transmission occurs amongst the higher-risk IDUs.Figure 6.7:The model’s projected impact on HIV compared to HCV for an intervention that eitherreaches all IDUs, or just lower- or higher-risk IDUsFigure 6.7a:Impact on HIV and HCV incidenceRelative decrease in HIV or HCV incidence (%)100
75
50
25
0HIV impactHCV impactHIV impactHCV impactHIV impactHCV impact
Reach all IDUs
Reach just higher-riskIDUs
Reach just lower-riskIDUs
Figure 6.7b:Impact on HIV or HCV infections averted160Number of infections averted140120100806040200HIV impactHCV impactHIV impactHCV impactHIV impactHCV impact
Reach all IDUs
Reach just higher-riskIDUs
Reach just lower-riskIDUs
180
Chapter 6: The effect of epidemiological setting on the impact of harm reduction targeting injecting drug users
Figure 6.7c:Relative impact on HIV compared to HCV
350Relative impact on HIV compared to HCV (%)300250200150100500Reach allIDUsReach justhigher-riskIDUsReach justlower-riskIDUsReach allIDUsReach justhigher-riskIDUsReach justlower-riskIDUsBelow line – more impact on HCVAbove line – more impact on HIV
Relative impact on incidence
Relative number of infections averted
DiscussionThis study extensively fit a mathematical model to observed trends between HIV and HCVprevalence in different IDU populations in Europe and beyond. Through fitting the model to awide range of different joint HIV and HCV epidemics, we were able to explore why differentHIV and HCV prevalence trends occur in different settings, project how the impact of anintervention targeting IDUs may vary for different epidemiological settings, and how theimpact of the intervention on HCV transmission may compare to the impact on HIVtransmission. In addition, as a by-product of the fitting process, estimates for the relativetransmissibility of HCV relative to HIV were also produced.This model analysis should be seen as a significant improvement upon previous modellinganalyses because of the effort made to ensure that the model mimics a wide range ofobserved HIV/HCV epidemics. Indeed, through undertaking this novel method of modelfitting, an analysis of the different best-fitting model simulations suggest that heterogeneity inIDU syringe sharing risk behaviour could be a major determinant for the wide range of HIVand HCV epidemics that occur in IDU populations in different settings, including Europe. Ifthis is the case, then the ratio of HIV to HCV prevalence in a stable epidemic setting could beused as a proxy indicator of the heterogeneity in injecting risk behaviour in that IDUpopulation.
181
Harm reduction: evidence, impacts and challenges
Key messages of this research1. Heterogeneity in IDU risk behaviour could be a major determinant for the wide range ofHIV and HCV epidemics that occur in IDU populations in different settings.2. Model projections suggest that greater intervention impact (more infections averted andgreater decrease in incidence) should be expected in higher HCV prevalence settings andless impact in higher HIV prevalence settings, except for the number of HIV infectionsaverted, which increases with HIV prevalence.3. An intervention will generally result in greater impact on an HIV epidemic than on an HCVepidemic, in terms of either infections averted or relative decreases in incidence. However,when the intervention reaches only lower-risk IDUs, it has only little impact on the HIVepidemic and greater impact on the HCV epidemic.4. The ratio of HIV to HCV prevalence in a stable epidemic setting could be used as a proxyindicator of the heterogeneity in injecting risk behaviour in an IDU population, and therelative number of HIV and HCV infections that would be averted by an intervention.
Relative impact of intervention in different epidemiological settingsAs would be expected, our results show that the number of infections averted by a specificintervention will be highly dependent on the characteristics of the epidemic occurring in asetting. However, our results also highlight that the relative reduction in HIV or HCV incidenceattained by an intervention can vary by six fold depending on the type of epidemicoccurring. Importantly, the projections imply that the number of infections averted and theassociated relative decrease in incidence are both strongly related to the HIV and HCVprevalence in a setting. Generally, greater impact (more infections averted and greaterdecrease in incidence) is achieved in higher HCV prevalence settings and less impact isachieved in higher HIV prevalence settings, except for the number of HIV infections averted,which increases with HIV prevalence.These results suggest that the highest impact in terms of reducing HIV/HCV incidence andaverting HCV infections should be expected at very high HCV prevalence (>70 %) but lowHIV prevalence (<10 %), such as has been recorded in some settings in Belgium, Greece,Ireland or Italy. In contrast, the greatest impact in terms of HIV infections averted occurs athigh HIV prevalence (>50 %) as occurs in some settings in Ukraine or Belarus (Vickerman etal., 2006b; Vickerman and Watts, 2002). These results highlight that policymakers should notexpect interventions to result in the same impact on incidence, or in the same number ofinfections averted when initiated in different settings. Indeed, an intervention’s cost-effectiveness ratio will vary widely within and between countries, and different coveragelevels and reductions in syringe sharing will be required to achieve specific reductions indisease incidence in different settings. This analysis can help in producing these targets andin estimating the relative cost-effectiveness of specific interventions in different settings.
182
Chapter 6: The effect of epidemiological setting on the impact of harm reduction targeting injecting drug users
Interestingly, if HIV and HCV infections are considered in a similar light in public healthterms, as could be the case in many European settings, then the projections haveimportant implications for how the impact and cost-effectiveness of an intervention isestimated. For example, although less is achieved in reducing HIV/HCV incidence andfewer HCV infections are averted in high HIV prevalence settings, interventions can stillhave a favourable cost-effectiveness ratio due to many HIV infections being averted.Alternatively, an intervention undertaken in a high HCV but low HIV prevalence setting, asoccurs in many European regions, may not be seen as cost-effective if only the cost perHIV infection averted is considered. However, in these settings many more HCV infectionswill be averted and the intervention is likely to have a large effect on the transmission ofboth infections. To explore this further, quality-adjusted life year (QALY) weights and HIVand HCV health care costs could be incorporated to give relative weights to the benefitsof a HIV or HCV infection averted, so that the cost-effectiveness of different interventionscan be compared in different epidemiological settings depending on the level of careprovided in that country.HIV and HCV impact of targeting low- or high-risk IDUsWhen the HIV and HCV impact projections are compared further, they suggest that anintervention will generally result in greater decreases in HIV incidence than HCV incidence.This is especially true if the intervention mainly reaches higher-risk IDUs, and highlights thatgreater coverage and reductions in risk behaviour will frequently be required by interventionsto achieve a comparable impact on HCV incidence as well as HIV incidence. This trend alsooccurs, and is more pronounced, when we look at the relative decrease in HIV or HCVprevalence (results not shown). This has important implications for harm reductioninterventions because it suggests that much more needs to be done if the objective of theintervention is a decrease in HCV transmission.Limitations of analysisThe analysis was limited in a number of ways. First, it used a limited number of biologicalparameter sets from a previous analysis as the basis for the fitting process. This may havelimited the number of model fits that we found and so there may be more uncertainty aroundour impact projections. The model was only fit against HIV and HCV prevalence trends. Adifferent parameter set may have produced a better fit to other ecological data, such astrends in HIV/HCV co-infection. Behavioural data was not used in the fitting process, and soit was difficult to determine whether the behavioural parameters used would produce similarepidemics in real life. In addition, the transmission of HIV through sexual contact was notincorporated in the model. Although HIV transmission through injecting risk behaviours islikely to dominate in most situations, sexual transmission could play a substantial role insettings where the HIV prevalence is already high but injecting risk behaviours havedecreased in recent years. This could affect the relationship not only between HIV and HCVprevalence, but also, and most likely, between HIV incidence and HIV prevalence or HIVincidence and HCV incidence.183
Harm reduction: evidence, impacts and challenges
Only one intervention was considered in the impact analysis and so it is impossible todetermine how the results would vary for other interventions. The impact analysis also assumedthe HIV and HCV epidemics were in a stable state. Importantly, epidemics in the exponential orearly epidemic stage would have resulted in different impact projections. Lastly, the model wasdeterministic and did not incorporate the effects on transmission of different syringe sharingbehaviours within different risk networks. These more complex syringe sharing structures mayaffect the prevalence of HIV and HCV in different ways, possibly restricting HIV in small IDUsub-networks, and so could explain the reason why the current model structure was not able topredict very low HIV prevalences with high HCV prevalences. The effect of these complexitieson our projections will be explored in future analyses involving more complex models.
Concluding remarksThis analysis used a novel technique to fit a joint HIV/HCV model to HIV and HCV prevalencedata from diverse epidemic types, many of which were from European settings. This enabledthe model to explore the impact of interventions in different epidemic settings, with the resultssuggesting that HIV and HCV prevalence could be used as predictors of intervention impactin different settings, including Europe. However, the study should be seen as preliminarybecause a limited number of ‘biological’ parameter sets (HIV and HCV transmissionprobabilities and natural history parameters) were used in the fitting and the model was onlyfit to HIV/HCV prevalence trends. In addition, the analysis did not explore the impact ofinterventions such as opioid substitution treatment (OST), HCV and/or HIV antiviraltreatments, and/or combined interventions, which may be essential for resulting in largereductions in HIV/HCV incidence in some settings. This has recently been highlighted by astudy looking at the long-term impact of intervention activities in Amsterdam (van den Berg etal., 2007), and will be the focus of future work where sufficient attention can be given tosubtleties such as how increasing the coverage of OST may increase the coverage of syringedistribution to IDUs on and off OST, and how the behaviour of IDUs may revert after leavingOST. In addition, previous analyses have suggested that reducing the number of people thatan IDU shares needles/syringes with and the time that IDUs are initially reached by harmreduction interventions are both important for determining the impact of a harm reductionintervention. These will also be explored further in future analyses.
AcknowledgementsPeter Vickerman designed the study, developed the model, undertook all analyses and wrote thefirst draft of the chapter. Matthew Hickman contributed to the study concept, helped withinterpreting the results, and contributed to writing the manuscript. Tim Rhodes and V. AnnaGyarmathy helped edit the chapter. The views expressed are those of the authors and cannot betaken to reflect the official opinions of the London School of Hygiene and Tropical Medicine.Financial support was provided from a Medical Research Council New Investigators award (heldby P.V.) and the European Monitoring Centre for Drugs and Drug Addiction. Lastly, grateful thanksgoes to Lucas Wiessing and all contributors to the EMCDDA HIV and HCV prevalence database,which was highly useful for providing data for the meta-analysis used in this model analysis.184
Chapter 6: The effect of epidemiological setting on the impact of harm reduction targeting injecting drug users
ReferencesAitken, C. K., Tracy, S. L., Revill, P., et al. (2008), ‘Consecutive infections and clearances of different hepatitis Cvirus genotypes in an injecting drug user’,Journal of Clinical Virology41, pp. 293–6.Baggaley, R. F., Boily, M. C., White, R. G., and Alary, M. (2006), ‘Risk of HIV-1 transmission for parenteralexposure and blood transfusion: a systematic review and meta-analysis’,AIDS20, pp. 805–12.Blower, S. M., Hartel, D., Dowlatabadi, H., Anderson, R. M. and May, R. M. (1991), ‘Drugs, sex and HIV: amathematical model for New York City’,Philosophical Transactions of the Royal Society B: Biological Sciences331,pp. 171–87.Bonacini, M., Lin, H. J. and Hollinger, F. B. (2001), ‘Effect of coexisting HIV-1 infection on the diagnosis andevaluation of hepatitis C virus’,Journal of Acquired Immune Deficiency Syndromes26, pp. 340–4.Cox, A. L., Netski, D. M., Mosbruger, T., et al. (2005), ‘Prospective evaluation of community-acquired acute-phase hepatitis C virus infection’,Clinical Infectious Diseases40, pp. 951–8.Craine, N., Hickman, M., Parry, J. V., et al. (2009), ‘Incidence of hepatitis C in drug injectors: the role ofhomelessness, opiate substitution treatment, equipment sharing, and community size’,Epidemiology and Infection137 (9), pp. 1255–65.Currie, S. L., Ryan, J. C., Tracy, D., et al. (2008), ‘A prospective study to examine persistent HCV reinfection ininjection drug users who have previously cleared the virus’,Drug and Alcohol Dependence93, pp. 148–54.Daar, E. S., Lynn, H., Donfield, S., et al. (2001), ‘Relation between HIV-1 and hepatitis C viral load in patientswith hemophilia’,Journal of Acquired Immune Deficiency Syndromes26, pp. 466–72.Dalgard, O. (2005), ‘Follow-up studies of treatment for hepatitis C virus infection among injection drug users’,Clinical Infectious Diseases40 (Supplement 5), pp. S336–S338.Danis, K., Doherty, L., McCartney, M., McCarrol, J. and Kennedy, H. (2007), ‘Hepatitis and HIV in NorthernIreland prisons: a cross-sectional study’,Eurosurveillance12, pp. 9–12.De Carli, G., Puro, V. and Ippolito, G. (2003), ‘Risk of hepatitis C virus transmission following percutaneousexposure in healthcare workers’,Infection31 (Supplement 2), pp. 22–7.Des Jarlais, D. C., Perlis, T., Arasteh, K., et al. (2005), ‘Reductions in hepatitis C virus and HIV infections amonginjecting drug users in New York City, 1990–2001’,AIDS19 (Supplement 3), pp. S20–S25.EMCDDA (2008),Annual report 2008: the state of the drugs problem in the European Union,European MonitoringCentre for Drugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/publications/annual-report/2008.Fishbein, D. A., Lo, Y., Netski, D., Thomas, D. L. and Klein, R. S. (2006), ‘Predictors of hepatitis C virus RNA levelsin a prospective cohort study of drug users’,Journal of Acquired Immune Deficiency Syndromes41, pp. 471–6.Foss, A. M., Watts, C. H., Vickerman, P., et al. (2007), ‘Could the CARE-SHAKTI intervention for injecting drugusers be maintaining the low HIV prevalence in Dhaka, Bangladesh?’Addiction102, pp. 114–25.Gibson, D. R., Flynn, N. M. and McCarthy, J. J. (1999), ‘Effectiveness of methadone treatment in reducing HIVrisk behavior and HIV seroconversion among injecting drug users’,Aids13, pp. 1807–18.
185
Harm reduction: evidence, impacts and challenges
Gibson, D. R., Flynn, N. and Perales, D. (2001), ‘Effectiveness of syringe exchange programs in reducing HIV riskbehavior and HIV seroconversion among injecting drug users’,AIDS15, pp. 1329–41.Goldberg, D., Burns, S., Taylor, A., et al. (2001), ‘Trends in HCV prevalence among injecting drug users inGlasgow and Edinburgh during the era of needle/syringe exchange’,Scandinavian Journal of Infectious Diseases33, pp. 457–61.Grebely, J., Conway, B., Raffa, J. D., et al. (2006), ‘Hepatitis C virus reinfection in injection drug users’,Hepatology44, pp. 1139–45.Grebely, J., Genoway, K., Khara, M., et al. (2007), ‘Treatment uptake and outcomes among current and formerinjection drug users receiving directly observed therapy within a multidisciplinary group model for the treatmentof hepatitis C virus infection’,International Journal of Drug Policy18, pp. 437–43.Grebely, J., Genoway, K. A., Raffa, J. D., et al. (2008), ‘Barriers associated with the treatment of hepatitis C virusinfection among illicit drug users’,Drug and Alcohol Dependence93, pp. 141–7.Grover, G. and Shivraj, S. O. (2004), ‘Survival pattern of reported HIV infected individuals in the city of Delhi(India)’,Journal of Communicable Diseases36, pp. 83–92.Health Protection Agency (2004),Shooting up: infections among injecting drug users in the United Kingdom 2003,Health Protection Agency, London.Health Protection Agency (2008),Shooting up: infections among injecting drug users in the United Kingdom 2007,Health Protection Agency, London.Hutchinson, S., Bird, S., Taylor, A. and Goldberg, D. (2006), ‘Modelling the spread of hepatitis C virus infectionamong injecting drug users in Glasgow: implications for prevention’,International Journal of Drug Policy17, pp.211–21.Kapadia, F., Vlahov, D., Des Jarlais, D. C., et al. (2002), ‘Does bleach disinfection of syringes protect againsthepatitis C infection among young adult injection drug users?’Epidemiology13, pp. 738–41.Kaplan, E. H. and Heimer, R. (1994), ‘A circulation theory of needle exchange [editorial]’,AIDS8, pp. 567–74.Kretzschmar, M. and Wiessing, L. G. (1998), ‘Modelling the spread of HIV in social networks of injecting drugusers’,AIDS12, pp. 801–11.Kretzschmar, M. and Wiessing, L. (2004), ‘Modelling the transmission of hepatitis C in injecting drug users’, inJager, J. C., Limburg, W., Kretzschmar, M., Postma, M. J. and Wiessing, L. (eds),Hepatitis C and injecting druguse: impact, costs and policy options,European Monitoring Centre for Drugs and Drug Addiction, Lisbon.Kretzschmar, M. and Wiessing, L. (2008), ‘New challenges for mathematical and statistical modeling of HIV andhepatitis C virus in injecting drug users’,Aids22, pp. 1527–37.Kumarasamy, N., Solomon, S., Flanigan, T. P., et al. (2003), ‘Natural history of human immunodeficiency virusdisease in southern India’,Clinical Infectious Diseases36, pp. 79–85.Kwon, J. A., Iversen, J., Maher, L., Law, M. G. and Wilson, D. P. (2009), ‘The impact of needle and syringeprograms on HIV and HCV transmissions in injecting drug users in Australia: a model-based analysis’,Journal ofAcquired Immune Deficiency Syndromes51, pp. 462–9.Larghi, A., Zuin, M., Crosignani, A., et al. (2002), ‘Outcome of an outbreak of acute hepatitis C among healthyvolunteers participating in pharmacokinetics studies’,Hepatology36, pp. 993–1000.
186
Chapter 6: The effect of epidemiological setting on the impact of harm reduction targeting injecting drug users
Limburg, W. (2004),Natural history, treatment and prevention of hepatitis C in injecting drug users: an overview,inJager, J. C., Limburg, W., Kretzschmar, M., Postma, M. J. and Wiessing, L. (eds),Hepatitis C and injecting druguse: impact, costs and policy options,European Monitoring Centre for Drugs and Drug Addiction, Lisbon.Mehta, S. H., Cox, A., Hoover, D. R., et al. (2002), ‘Protection against persistence of hepatitis C’,Lancet359, pp.1478–83.Micallef, J. M., Kaldor, J. and Dore, G. J. (2006), ‘Spontaneous viral clearance following acute hepatitis Cinfection: a systematic review of longitudinal studies’,Journal of Viral Hepatitis13, pp. 34–41.Micallef, J. M., Macdonald, V., Jauncey, M., et al. (2007), ‘High incidence of hepatitis C virus reinfection withina cohort of injecting drug users’,Journal of Viral Hepatitis14, pp. 413–18.Muga, R., Langohr, K., Tor, J., et al. (2007), ‘Survival of HIV-infected injection drug users (IDUs) in the highlyactive antiretroviral therapy era, relative to sex- and age-specific survival of HIV-uninfected IDUs’,ClinicalInfectious Diseases45, pp. 370–6.Murray, J. M., Law, M. G., Gao, Z. and Kaldor, J. M. (2003), ‘The impact of behavioural changes on theprevalence of HIV and hepatitus C among injecting drug users’,International Journal of Epidemiology32, pp.708–14.Pappalardo, B. L. (2003), ‘Influence of maternal human immunodeficiency virus (HIV) co-infection on verticaltransmission of hepatitis C virus (HCV): a meta-analysis’,International Journal of Epidemiology32, pp. 727–34.Pilcher, C. D., Price, M. A., Hoffman, I. F., et al. (2004a), ‘Frequent detection of acute primary HIV infection inmen in Malawi’,AIDS18, pp. 517–24.Pilcher, C. D., Tien, H. C., Eron, J. J., Jr., et al. (2004b), ‘Brief but efficient: acute HIV infection and the sexualtransmission of HIV’,Journal of Infectious Diseases189, pp. 1785–92.Pollack, H. A. (2001), ‘Cost-effectiveness of harm reduction in preventing hepatitis C among injection drug users’,Medical Decision Making21, pp. 357–67.Quinn, T. C., Wawer, M. J., Sewankambo, N., et al. (2000), ‘Viral load and heterosexual transmission of humanimmunodeficiency virus type 1. Rakai Project Study Group’,New England Journal of Medicine342, pp. 921–9.Thomas, D. L., Astemborski, J., Rai, R. M., et al. (2000a), ‘The natural history of hepatitis C virus infection: host,viral, and environmental factors’,Jama284, pp. 450–6.Thomas, D. L., Astemborski, J., Vlahov, D., et al. (2000b), ‘Determinants of the quantity of hepatitis C virus RNA’,Journal of Infectious Diseases181, pp. 844–51.Thomas, D. L., Rich, J. D., Schuman, P., et al. (2001), ‘Multicenter evaluation of hepatitis C RNA levels amongfemale injection drug users’,Journal of Infectious Diseases183, pp. 973–6.UNAIDS (2004a),AIDS epidemic update,UNAIDS, Geneva, pp. 1–21.UNAIDS (2004b),Report on the global HIV/AIDS epidemic,UNAIDS, Geneva, pp. 1–225.van den Berg, C., Smit, C., Van Brussel, G., Coutinho, R. A. and Prins, M. (2007), ‘Full participation in harmreduction programmes is associated with decreased risk for human immunodeficiency virus and hepatitis C virus:evidence from the Amsterdam cohort studies among drug users’,Addiction102, pp. 1454–62.Vickerman, P. and Watts, C. H. (2002), ‘The impact of an HIV prevention intervention for injecting drug users inSvetlogorsk, Belarus: model predictions’,International Journal of Drug Policy13, pp. 149–64.
187
Harm reduction: evidence, impacts and challenges
Vickerman, P., Hickman, M., Rhodes, T. and Watts, C. H. (2006a), ‘Model projections on the required coverageof syringe distribution to prevent HIV epidemics among injecting drug users’,Journal of Acquired ImmuneDeficiency Syndromes42, pp. 355–61.Vickerman, P., Kumaranayake, L., Balakireva, O., et al. (2006b), ‘The cost-effectiveness of expanding harmreduction activities for injecting drug users in Odessa, Ukraine’,Sexually Transmitted Diseases33 (Supplement),pp. S89–S102.Vickerman, P., Hickman, M. and Judd, A. (2007), ‘Modelling the impact of hepatitis C transmission of reducingsyringe sharing: London case study’,International Journal of Epidemiology36, pp. 396–405.Vickerman, P., Hickman, M., May, M., Kretzschmar, M. and Wiessing, L. (2009a), ‘Can HCV prevalence be usedas a measure of injection-related HIV-risk in populations of injecting drug users? An ecological analysis’,Addiction105, pp. 311–18.Vickerman, P., Platt, L. and Hawkes, S. (2009b), ‘Modelling the transmission of HIV and HCV amongst injectingdrug users in Rawalpindi, a low HCV prevalence setting in Pakistan’,Sexually Transmitted Infections85(Supplement 2), pp. ii23–30.Wawer, M. J., Gray, R. H., Sewankambo, N. K., et al. (2005), ‘Rates of HIV-1 transmission per coital act, bystage of HIV-1 infection, in Rakai, Uganda’,Journal of Infectious Diseases191, pp. 1403–09.Westh, H., Worm, A. M., Jensen, B. L., et al. (1993), ‘Hepatitis C virus antibodies in homosexual men andintravenous drug users in Denmark’,Infection21, pp. 115–17.WHO (World Health Organization) (2000a),Hepatitis C fact sheet,WHO, Geneva. Available at http://www.who.int/mediacentre/factsheets/fs164/en/.WHO (2000b),WHO drug injecting study — phase II operations manual version 4,des Jarlais D., Friedman, S.and Perlis, T. (eds), WHO, Geneva, 2000. Available at http://www.who.int/substance_abuse/activities/en/WHODrugInjectionStudyOperationsManual.pdf (accessed 1 October 2008).Wiessing, L. and Nardone, A. (2006), ‘Ongoing HIV and viral hepatitis infections in IDUs across the EU, 2001–2005’,Eurosurveillance11, pp. E061123 2.Yazdanpanah, Y., De Carli, G., Migueres, B., et al. (2005), ‘Risk factors for hepatitis C virus transmission tohealth care workers after occupational exposure: a European case-control study’, Clinical Infectious Diseases 41,pp. 1423–30.
188
Chapter 7The fast and furious — cocaine, amphetamines and harmreductionJean-Paul Grund, Philip Coffin, Marie Jauffret-Roustide, Minke Dijkstra, Dick de Bruin andPeter Blanken‘The role of the state is not to make people happy but to relieve avoidable suffering.’(Sir Karl Popper, 1945)
IntroductionCocaine and amphetamines (‘stimulants’) are distinct central nervous system stimulants withsimilar effects (Pleuvry, 2009; Holman, 1994). Cocaine is a crystalline tropane alkaloidextracted from coca leaves. Amphetamines are a subclass of phenylethylamines withprimarily stimulant effects, including amphetamine, methamphetamine, methcathinone andcathinone and referred to as ‘amphetamines’ in this review (Holman, 1994). MDMA(3,4-methylenedioxy-N-methamphetamine or ecstasy) is a substituted amphetamine knownfor its entactogenic, psychedelic, and stimulant effects (Morgan, 2000). Stimulants canproduce increased wakefulness, focus and confidence, elevated mood, feelings of power,and decreased fatigue and appetite; stimulants also produce nervousness or anxiety and,in some cases, psychosis and suicidal thoughts (Holman, 1994; EMCDDA, 2007f; Hildrey etal., 2009; Pates and Riley, 2009). Although there is little evidence that stimulants causephysical dependence, tolerance may develop upon repetitive use and withdrawal maycause discomfort and depression (EMCDDA, 2007f; Pates and Riley, 2009). Users mayengage in ‘coke or speed binges’ alternated with periods of withdrawal and abstinence(Beek et al., 2001).Epidemiology of stimulant use in the European UnionThe European Monitoring Centre for Drugs and Drug Addiction (EMCDDA, 2009)estimates that at least 3.9 % of the total adult population (15–64 years) in European Union(EU) Member States has used cocaine at least once in their lifetime (lifetime prevalence,LTP), but variations in prevalence and patterns are found between countries, demographicand social groups, and specific settings. Higher levels of cocaine use are found in westernand southern countries, notably Denmark, Spain, Italy, Ireland and the United Kingdom,with relatively low LTP in most other European countries, ranging from 0.1 % to 8.3 %(EMCDDA, 2009). Cocaine use is concentrated among young adults (15–34 years), with anaverage LTP of 5.3 %, and more so among young men, with an LTP over 10 % and lastyear prevalence (LYP) over 5 % in Denmark, Spain, and the United Kingdom (EMCDDA,2007b). LYP for all EU adults is 1.3 %, ranging from 0 % to 3.1 % by country. LYP amongyoung adults is 2.2 %, ranging from 0.1 % to 5.5 %. Last month prevalence (LMP) for alladults range from 0 % to 1.1 %, two-thirds of whom are young adults (EMCDDA, 2007f).191
Harm reduction: evidence, impacts and challenges
Cocaine use appears to have increased among young adults since the 1990s and, whileprevalence is leveling off or decreasing in many countries (EMCDDA, 2007a), Denmarkand Italy report considerable increases as recently as 2005 and Spain, France, Denmark,and the United Kingdom report rapid growth among adults aged 15–24 (EMCDDA,2007d). Those countries with data on problem cocaine use include Spain, with 4.5 to 6problem cocaine users per 1 000 adults in 2002, Italy with 2.9 to 4.1 per 1 000 adults in2005, and England with 5.7 to 6.4 problem crack users per 1 000 adults in 2004/05(EMCDDA, 2007c).Cocaine use is elevated in specific social settings and subpopulations, such as nightlifeparticipants with rates from 10 to 60 % (Cohen and Sas, 1993; Cohen and Sas, 1994;Decorte, 2001; EMCDDA, 2007d; Nabben et al., 2007; Grund et al., 2007b; Haasen et al.,2004), sex workers, homeless people, treatment participants and marginalised young adults(EMCDDA, 2007d; Haasen et al., 2004). Largely employed, socially integrated users mostlysniff cocaine and do so occasionally within rather well-defined leisure settings and periods(Prinzleve et al., 2004; Bellis et al., 2003; Cohen and Sas, 1994; Decorte, 2001), with someexperiencing periods of often short-lived uncontrolled use (Cohen and Sas, 1994; Decorte,2001), a finding consistent with laboratory studies in which experienced cocaine usersregulate their use (Sughondhabirom et al., 2005). Marginalised users, on the other hand,very often smoke cocaine-base (crack) or inject cocaine, use more frequently and chaotically,and more often use heroin, benzodiazepines or alcohol, while also experiencing a widearray of social-economic and medical problems (Prinzleve et al., 2004; Beek, 2001; Hando etal., 1997).LTP of amphetamines among EU adults is 3.3 %, ranging from 0.1 % to 11.9 %, with 0.6 %LYP. As with cocaine, more young adults use amphetamines, with 5 % LTP and 1.3 % LYP(EMCDDA, 2008). Amphetamines are more common in nightlife, in particular in specificdance scenes, such as Hardcore, Tekno or Goa (Nabben et al., 2007; Grund et al.,2007b). In contrast to cocaine, amphetamine use is higher in northern, central and easternparts of the EU, particularly Sweden and Finland, with rising rates among young adults inAustria, Germany, Denmark and southern Italy (Degenhardt et al., 2009). Amphetamineinjecting is a long-established problem in the Czech Republic and increasing in Slovakiaand Hungary (where methamphetamine use and injection is common) (EMCDDA, 2008;Degenhardt et al., 2009; Griffiths et al., 2008) as well as Estonia and countries across theeastern borders, such as Ukraine, Belarus, Russia and Georgia (Degenhardt et al., 2009;Griffiths et al., 2008; Grund et al., 2009; Grund and Merkinaite, 2009) Users in formerSoviet states often produce amphetamine-type stimulants at home (Borodkina et al., 2005;Grund, 2001; Heimer et al., 2007), creating an environment where injecting is commonamong recreational users, in contrast to western EU countries where a division betweenintegrated (party) and marginalised users of amphetamine seems to exist, similar to thatbetween cocaine snorters and smokers or injectors (Grund, 2001; Grund et al., 2009;Degenhard et al., 2009).LTP of ecstasy among EU adults is about 3 %, ranging from 0.3 to 7.3 %, with 0.8 % LYP.Among young adults, LTP is 5.6 % and LYP is 1.8 % (EMCDDA, 2008). The geographic192
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
diffusion of ecstasy is less clear than that of cocaine and amphetamines, but is associatedwith diffusion of the electronic dance music culture (House or Techno parties, raves, etc.).Ecstasy is almost exclusively taken orally, most users are well-integrated and few seektreatment barring other drug or alcohol problems (EMCDDA, 2008). Thus, although thepotential for harm of ecstasy use is not fictional, the reported burden of harm is very low inthe EU compared to those of cocaine and amphetamines. For this reason this review willlargely focus on (problem) use of cocaine and amphetamines. Fletcher and colleagues (2010)provide an overview of newly emerging harm reduction interventions aimed at users ofecstasy, amphetamines and other drugs in recreational settings.In this review we use the term ‘stimulant(s)’ when discussing cocaine and (meth)amphetaminesin general terms. We will use ‘cocaine’ when discussing this substance in either its salt orbase form. ‘Smokable cocaine’ or colloquial terms like ‘crack’ will only be used whenindicated (as in ‘crack pipes’). Note that the term ‘crack’ is associated with stigma amongdrug users and some prefer saying they smoke ‘free-base’, instead of crack. Likewise, we use‘amphetamines’ as a much as possible, when discussing amphetamines in general terms anduse either ‘amphetamine’, ‘methamphetamine’ or ‘(meth)cathinone’ when referring to thosespecific substances.
MethodologyThis review was primarily based on searches in the Medline database for relevant articles.Several search terms were used and generally limited papers to those addressing humansubjects and those published after 1990. The overwhelming majority of articles addresseda small number of harms and standardised search terms were unable to identifynumerous articles known by the authors to be relevant to risk management amongstimulant users. For example, we searched PubMed on 12 October 2008 for clinical trials,metaanalyses, randomised controlled trials, reviews, and practice guidelines involvinghuman subjects with the search terms (cocaine or psychostimulants or amphetamine ormethamphetamine) and (health consequences or overdose or cardiac toxicity or HIV orHCV or pregnancy) published after 1990, resulting in 779 papers. After eliminatingpapers that were not relevant (such as animal studies or medical use of stimulants), therewere 287 articles, of which 49 % referred to pregnancy, 21 % to infectious diseases, 10 %to cardiovascular disease, 5 % to neurologic disease, 5 % to other medical problems, 4 %to overdose. Several searches were replicated in World of Science and through universitysearch engines but with few additional relevant papers identified, nor did including morespecific search terms related to these topics. A number of articles were identified fromauthors’ previous knowledge and included in the review. With regard to infectiousdisease, stimulant use and harm reduction, 196 articles were identified in English andFrench; after examining these articles and selecting a number of other articles, 91references were included. Only a few peer reviewed publications addressed crack useand harm reduction, and most of these were grey. Mental health issues were investigatedin a similar fashion, including a broad search, manual review of the publications, andinclusion of outside sources including published papers, reports, organisational materials,and other grey publications.193
Harm reduction: evidence, impacts and challenges
Adverse (health) consequences associated with use of stimulantsKey findingsScientific literature is overwhelmingly weighted toward the harms of stimulants, with minimalliterature on harm reduction interventions. Among the myriad of ill health effects associated withstimulants, some are mediated by mode of administration (such as infections, overdose, andpulmonary damage) while others are independent thereof (such as neurologic, cardiovascularand mental health problems). But the distinction between the two categories of stimulant-relatedharm is subtle and contingent on the broader risk environment. For example:• roblem stimulant use is associated with poverty, unemployment, homelessness or unstable Phousing, lower socio-economic status, a variety of other social problems, as well as legalproblems and incarceration.• dulterants and use of caustic chemicals in drug preparation are stipulated by market Aconditions beyond the control of individual users.• raditional harm reduction programmes may fail to reach problem stimulant users due to Topiate-centred services and social barriers to young or female users.• nnovative service development paired with critical evaluation is necessary in translating Ithe successes of harm reduction for opiates to stimulants.• here is an important and unmet need for services that enhance the ability of stimulant Tusers to control their intake levels, chaotic behaviour and mental health problems, as wellas limit pulmonary, cardiovascular and neurologic harms.• timulant-related harms are aggravated by external factors, such as selected aspects of Sinternational drug legislation, policing and public policies in a process of ‘contingentcausality’.
The risks associated with stimulants include medical harms, such as infectious, cardiovascular,and neurologic and psychiatric morbidity, as well as risks to pregnancy, pulmonary andrenal toxicity, overdose and other less common sequelae. Problem stimulant use is alsoassociated with poverty, unemployment, homelessness or unstable housing, lower socio-economic status, a variety of other social problems, as well as legal problems andincarceration. Here we focus primarily on medical health consequences while brieflyaddressing mental health and other problems associated with stimulant use.Blood-borne virusesTransmission of blood-borne viruses is consistently associated with stimulant use (Mitchell et al.,2006), due primarily to high-frequency use and to increased risky sexual behaviors. HIV andhepatitis C (HCV) transmission among stimulant injectors has been associated with higherinjecting frequency (Kral et al., 2001; Gibson et al., 2002) and needle sharing (Rotheram-Boruset al., 1999). Frequent cocaine injection is a factor in the failure of selected syringe exchangeprogrammes to prevent HIV transmission (Wood et al., 2002). HCV rates are very high, even194
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
among recent initiates to cocaine injection (Maher et al., 2007). In central and eastern Europe,home-produced stimulants such as methcathinone and cathinone are injected up to 10 timesdaily (Kozlov et al., 2006; Booth et al., 2008; Grund et al., 2009; Chintalova-Dallas et al.,2009) and are associated with increased sexual activity (Kozlov et al., 2006) as well as sharingof equipment in home drug preparation (Grund, 2001; Des Jarlais et al., 2002; Grund andMerkinaite, 2009; Balakireva et al., 2006). In comparison to heroin users, stimulant users aremore likely to have unstable social situations, larger drug-using social networks, riskier injectionpractices (e.g. increased frequency, chaotic drug preparation, injecting in unstable settings) andincreased sexual activity (De et al., 2007; Elkashef et al., 2008; Grund et al., 1991b; Kozlov etal., 2006; Chintalova-Dallas et al., 2009; Booth et al., 2008). HCV is also prevalent amongnon-injection stimulant users, with rates of 2.3–35.3 % among those who sniff or smokestimulants (Scheinmann et al., 2007) and 2.3–81 % among crack smokers (Fischer et al., 2008;Jauffret-Roustide et al., 2008a; Tortu et al., 2001); many are unaware that they are infected(Roy et al., 2001; Kwiatkowski et al., 2002). Hepatitis B (HBV) infection has also been associatedwith injection and non-injection drug use (NIDU), although the availability of a vaccine hasgreatly reduced infection rates (Kottiri et al., 2005). Stimulant use is associated with infrequentcondom use (Edlin et al., 1992), amphetamine use preceding sex (Koblin et al., 2006), riskbehaviours among young gay men (Celentano et al., 2006), and trading sex for drugs ormoney (Serraino et al., 1991; Stevens et al., 1998; Tortu et al., 2000; Tortu et al., 2003).Cocaine smoking is a distinct risk factor for blood-borne virus transmission (Pechansky et al.,2006; Haydon and Fischer, 2005; McCoy et al., 2004; Adimora et al., 2003; Edlin et al.,1994; Chiasson et al., 1991; Haverkos and Steel, 1991), even when adjusted for injectionbehaviour (Wolff et al., 2007; Osher et al., 2003; Nyamathi et al., 2002; Rosenblum et al.,2001; Roy et al., 2001; Jauffret-Roustide et al., 2006), primarily due to an association withrisky sexual behaviour (Hagan et al., 2005; McCoy et al., 2004; Edlin et al., 1994; Lejuez etal., 2005; Campsmith et al., 2000; Gross et al., 2000; Perlman et al., 1999; Word andBowser, 1997; Centers for Disease Control and Prevention, 1996; Seidman et al., 1994; Edlinet al., 1992), with HIV prevalence estimates from 7.5–23.0 % (Jauffret-Roustide et al., 2006;McCoy et al., 2004; Edlin et al., 1994; Kral et al., 1998; Gyarmathy et al., 2002). Sex work ismore frequent among cocaine smokers compared to other drug users (Faruque et al., 1996;Edlin et al., 1994; Campsmith et al., 2000; Fischer et al., 2006; Mehrabadi et al., 2008) andwomen cocaine smokers are particularly vulnerable as they are exposed to multiple risksassociated with both sexual and drug use behaviours, contingent on broader genderrelations (Jauffret-Roustide et al., 2008b; Shannon et al., 2008; Maranda et al., 2004;Cotten-Oldenburg et al., 1999; Heffernan et al., 1996; McCoy and Miles, 1992; Balakireva etal., 2006). While sexual transmission of HIV among cocaine smokers is mainly throughunprotected intercourse (Haverkos and Steel, 1991), other routes include oral sores andcracked lips from hot pipes in the setting of unprotected fellatio (Faruque et al., 1996; Theallet al., 2003). Recent studies of cocaine smoking and HCV transmission have noted thecollective use of glass smoking utensils (‘crack pipes’ or ‘stems’) as a potential risk factor. HCVis present in gingival fluid (Suzuki et al., 2005), nasal secretions (McMahon et al., 2004),saliva (Hermida et al., 2002), and crack pipes (Fischer et al., 2008), the last of which arefrequently made of glass, metal or other materials that can get extremely hot, have jaggededges, and may break between clenching jaws. Oral sores and burns on lips can result fromusing these pipes (Ward et al., 2000; Faruque et al., 1996; Porter and Bonilla, 1993) and195
Harm reduction: evidence, impacts and challenges
small blood droplets deposit on the stem of the pipe, possibly transmitting HCV to others withsimilar sores (Hagan et al., 2005). One study reported that up to 81 % of all cocaine smokershad shared their crack pipes in the previous month (Jauffret-Roustide et al., 2006).Stimulant use may hasten progression of HIV disease, although data are conflicting. Cocaineuse has been associated with poor anti-retroviral initiation and adherence (Brewer et al.,2007), complicated by the interaction of depression, particularly among women (Cook et al.,2007) whose crack use is strongly associated with poor outcomes of HIV disease (Cook et al.,2008). While current or past cocaine use is associated with less favorable laboratoryparameters (T cell and viral load) among patients on HIV treatment, past amphetamine use isassociated with more favorable parameters (Cofrancesco et al., 2008). Studies of HIV-positive and HIV-negative men who have sex with men demonstrate no change in T cellcounts among subjects related to their use of cocaine or amphetamines (Chao et al., 2008),and studies among women showed no difference in CD4 count, viral load, or mortality(Thorpe et al., 2004). References are available to predict possible interactions of HIVmedications with illicit drugs (Wynn et al., 2005), but the clinical implication of theseinteractions remains uncertain (Pal and Mitra, 2006). The hypothesis of a directimmunomodulatory effect of stimulants that could increase vulnerability to HIV and otherinfections remains unproven (Cabral, 2006).Other infectious complicationsStimulants have been associated with increased incidence of many sexually transmitteddiseases including syphilis, gonorrhea, and chancroid (Bauwens et al., 2002; Friedman et al.,2003; Ross et al., 1999; Ross et al., 2002; Sorvillo et al., 1998; Stoner et al., 2000; Thomas etal., 1996; Centers for Disease Control and Prevention, 1991 and 1993; Chirgwin et al., 1991;Finelli et al., 1993; Martin and DiCarlo, 1994; Oxman et al., 1996; Shuter et al., 1998; Williamsand Ekundayo, 2001; Cleghorn et al., 1995), as well as various bacterial infections (Kerr et al.,2005) and tuberculosis (Malakmadze et al., 2005; McElroy et al., 2003). Cocaine use has beenindependently associated with human papillomavirus infection and progression to cervicallesions (Minkoff et al., 2008). Skin and soft tissue infections (SSTIs) affect 10–30 % of injectingdrug users (IDUs) (Binswanger et al., 2000; Murphy et al., 2001; Ciccarone et al., 2001) andare associated with loss of venous access and reliance on intramuscular or subcutaneousinjection (Ciccarone and Bourgeois, 2003; Lloyd-Smith et al., 2008; Binswanger et al., 2000).Injecting crack, vint or boltushka (home-made meth-cathinone) is particularly damaging to veinsdue to the uninformed and unskilled use of chemicals for preparation (Rhodes et al., 2006;Chintalova-Dallas et al., 2009). Jeff or boltushka is injected with large-bore needles that rapidlydamage veins. The United Kingdom has recently seen a rise in groin injection, with anestimated 45 % of IDUs in English cities recently injecting into the femoral vein (Maliphant andScott, 2005; Rhodes et al., 2006). Groin injection has been associated with public use of crackand speedballs and is now common among new initiates and housed IDUs, not just older andhomeless users with no other venous access, suggesting a shift from ‘risk boundary’ to‘acceptable risk’ (Rhodes et al., 2006; Rhodes et al., 2007). Cocaine injectors, includingwomen, those with unstable housing, and those who require help injecting, are independentlymore likely to have SSTIs (Lloyd-Smith et al., 2008).196
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
Shooting Jeff (homemade methcatinone), Pskov, Russia, 1999
Source:J-P. Grund.
Stimulants are also associated with skin lesions resulting from excessive scratching or picking.Most lesions are not due to delusions, apart from ‘Coke Bugs’ or ‘Meth Mites’, which result fromthe sensation that insects are crawling on or under the skin or that the drug is coming out of theskin. These are hallucinations from prolonged stimulant use and resulting sleep deprivation(Frieden, 2006; Beek et al., 2001; Lee, 2008). Known as delusional parasitosis, this behaviour isassociated with MRSA, streptococcal, and polymicrobial SSTIs (Hinkle and Nancy, 2000;Frieden, 2006; Beek et al., 2001; Cohen et al., 2007). Other self-mutilation behavioursobserved by outreach workers in Frankfurt include ‘working on wounds with giant knives’(primarily males), cutting (primarily females), cigarette burns and excessive fingernail-biting(both sexes) (personal email communication, M. Nickolai, 30 September 2009).Neurologic effectsCocaine induces plasticity in the dopaminergic system largely responsible for drugcraving, yet the principal neurologic effects of cocaine are related to its cardiovasculareffects: strokes, hemorrhages and blood clots. Persistent vasoconstriction may lead toreduced brain perfusion and associated cognitive deficits that may or may not resolvewith abstinence (Nnadi et al., 2005). Heavy methamphetamine use also inducesdopaminergic plasticity, as well as reduced dopaminergic activity and neuropsychiatricdeficits in memory, attention, and executive function (Ferris et al., 2008). Alterations in197
Harm reduction: evidence, impacts and challenges
brain structure and chemistry have been convincingly documented in heavy users ofmethamphetamine although the clinical implications of these data remain uncertain(Chang et al., 2007). Numerous studies of long-term prescribed amphetamines havefailed to demonstrate lasting psychiatric or neurologic deficits, although few are of highquality (Vitiello, 2001). In Central and Eastern Europe, chemical residues of homestimulant production (including potassium permanganate, gasoline, toluene ortetrachlorethylene, sodium hydroxide, or hydrochloric acid) (Grund and Merkinaite, 2009)may have toxic effects and local clinicans have reported ‘amphetamine-inducedmovement disorder’ (see e.g. Downes and Whyte, 2005) and declines in cognitivefunction and memory similar to dementia (Volik, 2008; Chintalova-Dallas et al., 2009).Pseudoephedrine restrictions in the region may have resulted in use of more hazardousprecursors such as phenylpropanolamine, associated with hemmorrhagic stroke (Horwitzet al., 2000), in production of cathinone (Chintalova-Dallas et al., 2009). In the setting ofHIV, stimulants have been associated with more rapid progression of cognitive declineand recent data suggest that stimulants may contribute to HIV-related neuron cell death,particularly within the dopaminergic (Ferris et al., 2008) and hippocampal (Venkatesan etal., 2007) systems (Goodkin et al., 1998; Basso and Bornstein, 2000; Nath et al., 2002;Cadet and Krasnova, 2007; Ferris et al., 2008).Cardiovascular effectsCardiovascular toxicities of cocaine are well-established (Vandhuick et al., 2004). Cocaineresults in adrenergic activation through effects on norepinephrine and clot formationthrough activation of platelets, resulting in increased cardiac oxygen demand, coronaryartery spasm, and coronary artery thrombosis. ‘Cocaine chest pain’ is usually not a signof cardiac ischemia, yet cocaine also increases the risk of true myocardial infarction,aortic dissection, coronary artery dissection, cardiomyopathy, and sudden cardiac death(Steinhauer and Caulfield, 2001; McCord et al., 2008). Injection of any drug is associatedwith endocarditis (Guerot et al., 2002). Cocaine-induced tachycardia and hypertensionplay a role in many of these sequelae (Tuncel et al., 2002), accounted for in part by directreduction in vagal tone (Newlin et al., 2000). Injected cocaine causes a dose-dependentprolongation of the QT segment of the cardiac cycle, raising the risk of potentially fatalarrhythmias (Haigney et al., 2006), particularly among those with genetic predispositionsfor QT prolongation (Karch, 2005). Overdose of cocaine can result in fatal monomorphicventricular tachycardia by blocking sodium channels (Bauman and DiDomenico, 2002).Dilated cardiomyopathy may be related to direct toxicity of cocaine through increasedprogrammed death of heart muscle cells (Zhang et al., 1999). Furthermore, prolongedcocaine use accelerates atherosclerosis (Kloner et al., 1992) and accumulation ofmetabolites in cardiac tissue may have further detrimental effects (Schindler et al., 1995).Clinicians are reluctant to use beta blockers, a key agent in heart disease, to managecocaine-related disease due to fear of producing unopposed activation of otheradrenergic receptors with cocaine (Afonso et al., 2007). Use of alcohol and cocainetogether leads to production of cocaethylene, which is believed to increase the cardiotoxiceffects of both drugs (Kertesz et al., 2007), increases the tachycardia produced bycocaine, and may increase the tendency toward violent thoughts and threats (Farre et al.,198
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
1997; Pennings et al., 2002). Amphetamines produce substantial increases in bloodpressure and heart rate, more marked when the drugs are injected and somewhatbuffered among those who also use marijuana (Fleury et al., 2008). Use of ecstasy,amphetamine, and cocaine in a club setting did not result in any excess body temperaturecompared to use of alcohol and/or cannabis alone; those drugs did, however, result in arelative increase in blood pressure (increase of 40mm Hg systolic) and heart rate (increaseof 30 beats/minute) (Mas et al., 1999), perpetuating concerns about possiblecardiovascular toxicities (Cole et al., 2005).
Pulmonary and other health effects
Novel interventions: reinventing the ‘micro’ risk environmentInterventions aimed at reducing harms of cocaine use focus on BBVs and thus on the micro riskenvironment of drug consumption, providing utensils and practical information for safer use.Crack kit programmes offer kits that generally include a Pyrex tube, plastic tips, filters,condoms, lip balm, sterile compresses and chewing gum for salivation (Aidslaw, 2007). Anevaluation of crack kit distribution in Ottawa (Leonard et al., 2006; Leonard et al., 2007)suggested that sharing of crack pipes decreased dramatically, while crack users reducedinjecting and more often smoked cocaine. The Dutch Mainline Foundation offers cocaineinformation in flyers, on the Internet and on the streets, including a van-based ‘health circuit’for cocaine smokers (Boekhout van Solinge, 2001) to check their lung capacity, bloodpressure and heart rate. The van is supervised by a trained nurse, providing participatoryinteraction in which pulmonary and mental health harm reduction and self-regulationstrategies are discussed through motivational interviewing techniques (Wittenberg, 2005).Mainline’s website and flyers emphasise practical information for managing health risks andcontrolling cocaine use, including tips for managing coke bugs, the coke shuffle and the urgeto scratch (e.g. http://www.cocaineinfo.nl/).Crack kits are controversial and rarely funded. In Canada and some US cities, crack kits aredistributed with regional funding (Small and Drucker, 2008), but some have closed after localopposition (Symington, 2007). At the same time, France is improving access to crack kits(Jauffret-Roustide et al., 2008a) with plans for community-based evaluations. Recenttechnological developments such as personal vaporisers, similar to E-cigarettes for tobaccosmokers, might offer additional opportunities to reduce pulmonary and other bodily harm, asvaporisation and filtering could reduce the amount of combustion products inhaled whileoffering an acceptable alternative to crack pipes and perhaps even syringes.Nonetheless, reactive harm reduction measures focused at the micro risk environment ofcocaine use do little to mediate the influences in the drug’s macro risk environment, uponwhich risk behaviour and drug related harms are contingent (Rhodes, 2009). This reviewidentifies an important need to apply harm reduction thinking in proactive policymakingtowards changing the ‘contingent causation’ of problem stimulant use with unhealthy drugand social policies and those that influence the public domain.
199
Harm reduction: evidence, impacts and challenges
The most notable pulmonary complication of smoked cocaine, referred to as ‘crack lung’, isdifficult to differentiate from several other associated and life-threatening restrictive,granulomatous, infectious, and hematologic pulmonary diseases and frequently requiresopen-lung biopsy to diagnose (Terra Filho et al., 2004; Wolff and O’Donnell, 2004). Thevasoconstrictor effect of smoked cocaine can also lead to pulmonary hypertension withchronic use (Glauser and Queen, 2007). Asthma exacerbations and eosinophilic pneumoniasare also described in relation to inhaled stimulants (Mayaud et al., 2001). Intranasal cocaineuse is clearly associated with septal necrosis and perforation (Glauser and Queen, 2007).Use of tobacco is thought to worsen pulmonary outcomes among stimulant smokers orinjectors (Wolff and O’Donnell, 2004).Amphetamine use has been associated with dental disease, although there is dispute as tothe degree of destruction that is related to direct toxicity versus diet and personal hygiene(Chi and Milgrom, 2008; Heng et al., 2008). Renal diseases related to stimulants includeglomerulonephritites, largely believed to be associated with IDU and contaminants, andtubulointerstitial processes resulting from vasoconstrictive properties in the setting of pre-existing mild renal disease (Crowe et al., 2000; Jaffe and Kimmel, 2006). Uncommoncomplications include renal infarction and rhabdomyolisis. Concerns with ecstasy use includehyperthermia and rhabdomyolisis with associated renal failure (Hedetoft and Christensen,1999). Fear of dehydration has led to consumption of large quantities of water that, inindividuals without appropriate regulation of antidiuretic hormone, may lead to dilutionalhyponatremia and, rarely, death (Crowe et al., 2000). Urinary retention due to bladder neckclosure has also been associated with ecstasy use (Crowe et al., 2000). Gastroschesis, orslowed gastric processing of food, has been associated with use of stimulants (Draper et al.,2008), and cocaine use has been associated with intestinal ischemia, likely due to bothvasoconstrictor and pro-thrombogenic effects (Glauser and Queen, 2007).OverdoseOpioids remain the source of most overdose deaths globally, yet in regions such as New YorkCity (Coffin et al., 2003) and Sao Paolo, Brazil (Mesquita et al., 2001), the high prevalence ofcocaine use contributes, often in conjunction with opioids, to the majority of overdose deaths.Among cocaine body-packers, overdose can result from the rupture of a container andrequires immediate laparotomy for chance of survival (Schaper et al., 2007). Extremeoverdose on stimulants can result in profound hyperthermia, with subsequent risks forrhabdomyolisis, seizures, and death (Callaway and Clark, 1994). Overdose on ecstasywithout concomitant use of other drugs is notably rare and difficult to define, but may berelated to seritonin syndrome (see ‘Neurologic effects’) (Schifano, 2004). In a survey of allamphetamine-related deaths in Belgium, cardiopulmonary arrest and trauma were the mostcommon direct causes of death, and drug metabolite levels were notably variable (De Letteret al., 2006). Cocaine use is intimately associated with opioid overdose, with combined useof the two drugs substantially increasing the risk of both nonfatal and fatal overdose (Ochoaet al., 2005; Coffin et al., 2003; Coffin et al., 2007). Furthermore, while overdose on opioidsis far more likely among IDUs, the rates are closer among injection and non-injection cocaineusers (Kaye and Darke, 2004).200
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
Pregnancy and parentingStimulant use during pregnancy and parenting has been a major concern, particularly in theUnited States where fears about a future generation of ‘crack babies’ inspired legislation andprosecutions against women for stimulant use, marijuana use, or any acts that might beconsidered risky during pregnancy (Harris and Paltrow, 2003). Risk factors for bad outcomesamong drug-using pregnant women include lack of prenatal care, prior premature delivery,and active cigarette smoking (Kuczkowski, 2007; Ness et al., 1999). Cocaine use duringpregnancy is more likely than opiates, tobacco, and marijuana to be associated with fetalgrowth decrements (Schempf, 2007), and is associated with abruptio placenta andpremature rupture of membranes; other concerns such as spontaneous abortion, pretermlabour, behavioural or developmental disabilities, feeding disturbances, or withdrawalsyndromes were confounded by other variables and often better attributed to maternalpoverty (Addis et al., 2001). Developmental effects, based on studies utilising vast arrays oftools in an effort to elucidate decrements, remain in doubt by some investigators (Frank et al.,2001), are at most subtle with unclear clinical significance (Lester et al., 2003) and aremediated with educational programmes (Schiller and Allen, 2005). Childhood psychiatriccorrelates are mediated by psychosocial factors and diminish as children age (Williams andRoss, 2007). There is no risk of direct toxicity to a pregnancy at the time of conception frommale cocaine use (Klemmt and Scialli, 2005). A thorough 2005 review of amphetamines andpregnancy found insufficient evidence to evaluate the developmental toxicity of therapeuticamphetamines, with two underpowered cohort studies showing no effect (Golub et al.,2005). Amphetamines have been associated with a 3.5 fold increased risk of fetal growthrestriction, while tobacco use had a twofold increased risk (Smith et al., 2006). Early researchhas demonstrated an association between amphetamine-using mothers and poor perceivedquality of life, increased substance use among family and friends, as well as ongoing legalproblems (Derauf et al., 2007).Mental health and social problemsHigh levels of psychiatric and social comorbidities, in addition to dependence and addiction,are found among chronic stimulant users (Hall et al., 1996; Baker et al., 2004; Darke et al.,2008; Sutcliffe et al., 2009). Chronic amphetamine use is associated with psychosis, usuallytransient during use or withdrawal but occasionally occuring for several years afterdiscontinuation (Scott et al., 2007). Pre-existing psychotic symptoms can be greatly exacerbatedby amphetamine initiation (Hall et al., 1996; Suttcliffe et al., 2009). Stimulant use is alsoassociated with suicide, suicidal ideation, depression, post-traumatic stress disorder, and severalpersonality disorders (Kertesz et al., 2006; Scott et al., 2007). Methamphetamine use has beenassociated with anti-social personality disorder as well as mania and bipolar mood disorder(Chen et al., 2003). Although methamphetamine has been associated with impulsive or violentbehavior, no causal relationship has ever been established (Scott et al., 2007). Compared tococaine, crack use is associated with higher levels of anxiety, depression paranoia, andpsychosis, likely due to intensity of use, physical health, and concurrent social situation ratherthan route of administration per se (Haasen, 2005). There is a strong association betweenamphetamine use and attention-deficit hyperactivity disorder (ADHD), which is treated with201
Harm reduction: evidence, impacts and challenges
amphetamine-type medications, leading some investigators to suspect that indviduals withADHD are drawn to amphetamine use (Jaffe et al., 2005; Scott et al., 2007).Problem use of stimulants is also associated with social and family problems, including poorinterpersonal relationships, child abuse or neglect, job loss, motor vehicle accidents, tradingsex for money or drugs, criminal or violent behaviour and homicide (Daley et al., 2002),although convincing causal relationships have not been established. Problem stimulant usersare more likely to be unemployed and experience poor coping skills, limited social support,and disorganised lifestyles (Scott et al., 2007), which may play a central role in behaviouralproblems. Furthermore, the criminal and stigmatised nature of stimulant use, while possiblydeterring wider use, serves as a barrier for problem users to participate in productive society(Grabowski et al., 2004).
Harm reduction for stimulant usersAre stimulants too fast and too furious for harm reduction? A relatively new focus for harmreduction programmers, stimulants require rethinking many traditional strategies. Here wediscuss the evidence for, and emerging interventions in, harm reduction for stimulant users. Westart with a brief review of behavioural and pharmacologic treatment interventions for stimulantdependence and then focus on the stimulant-specific harms discussed in the previous section.Behavioural and pharmacologic interventions for stimulant users
Challenges for harm reduction for stimulant usersHarm reduction for problem stimulant users is both crucial and feasible, but requiresconsideration of the unique characteristics of stimulant use. There are many obstacles,including:• requent cocaine injection is a factor in the failure of selected syringe exchange programmes Fto prevent HIV transmission and in low treatment success and retention.• ocal studies among IDUs in English cities show show that up to 45 % report recent injecting Linto the femoral vein.• ocaine smoking is a growing risk factor for blood-borne virus transmission, due to Cassociations with risky sex and collective use of smoking utensils.• emale users are exposed to multiple risks associated with both sexual and drug use Fbehaviours, which are contingent on broader gender relations.• espite shifts toward smoking drugs in many EU countries, public health efforts remain Dalmost exclusively focused on IDUs.Independent of mode of administration, stimulant and other drug users must enjoy thefundamental human right to health protection, as stipulated by Article 25 of the UniversalDeclaration of Human Rights.
202
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
Generally, the primary goal of treatment is viewed as inducing abstinence and preventingrelapse (‘cure’). If abstinence is not (yet) feasible, treatment should aim at reducing or atleast stabilising substance use and its consequences (‘care’). The ultimate stage oftreatment should be lenitive and aim at alleviating suffering (‘palliation’). At all stages,crisis intervention, treatment of intoxication and withdrawal, and improving health,psychological and social functioning are self-evident (Health Council of the Netherlands,2002).The first line of treatment for problem stimulant use is outpatient psychosocial intervention(American Psychiatric Association, 2007), most notably cognitive behaviour therapy (CBT),contingency management (CM) (Dutra et al., 2008), and motivational interviewing (MI)(Shearer, 2007; EMCDDA, 2007e). In CM a well-described target behaviour (e.g.,medication compliance, clinic attendance, stimulant use abstinence, or any other verifiablebehaviour) is rewarded whenever the behaviour is demonstrated (Dutra et al., 2008). CMis most effective when cash (as opposed to vouchers) and higher-value incentives areused, and although the effects diminish after the intervention is discontinued, effects ofincentives have been demonstrated for up to 12 months thereafter (Lussier et al., 2006;Prendergast et al., 2006).There is no proven effective pharmacological treatment for cocaine and stimulant use, inspite of the large number of studies on a broad array of pharmaceuticals (for reviews, see:De Lima et al., 2002; EMCDDA, 2007e; Pirona and Hedrich, 2009). More recently, theCocaine Rapid Efficacy Screening Trial (CREST) tested 19 medications, of which threepotentially effective compounds (cabergoline, reserpine and tiagabine) were movedforward to be tested in larger, confirmatory trials (Leiderman, 2005; Kampman et al.,2005). However, in recent larger trials neither tiagabine (Winhusen et al., 2007a) norreserpine (Winhusen et al., 2007b) were effective in reducing cocaine use compared toplacebo. Another approach is to develop a vaccine to prevent cocaine from crossing theblood–brain barrier; the current vaccine needs improvement (Martell et al., 2009) andthere are many ethical issues to be addressed even once a vaccine has shown to beeffective (see e.g. Hall and Carter, 2004).More recently, there is growing interest in shifting the focus from abstinence to ‘substitutiontreatment’, based on the effectiveness of replacement therapy for nicotine and opiatedependence (Moeller et al., 2008; Shearer, 2008). The rationale for substitution treatment isto replace harmful stimulant drug use ‘with safer, licit pharmaceutical drugs, avoidingcontaminants and risks associated with hazardous routes of administration, such as injecting(blood-borne viral infections, overdose)’ (Shearer, 2008, pp. 302–03). Ultimately, substitutiontreatment should result in a stabilisation of illicit drug use, thereby enabling the stimulant druguser to benefit from additional psychosocial interventions. Although the evidence to date forsubstitution treatment of stimulant use is scant (De Lima et al., 2002; Castells et al., 2007),dexamphetamine (SR) and modafinil seem promising candidates for further study. Llosa(1994) and Hurtado-Gumucio (2000) have also documented in non-controlled studies thatcoca tea, coca leaves and cocaine tablets could be effective in terms of craving, cocaine useand social functioning.203
Harm reduction: evidence, impacts and challenges
Interventions aimed at reducing adverse (health) consequences associatedwith stimulant useBlood-borne virusesHarm reduction for stimulant injectors relies heavily on the evidence for HIV prevention amongheroin injectors (see e.g. Kimber et al., 2010), but demands consideration of the unique settingof stimulant injection. In particular, stimulant injection involves more frequent injection, increasedsexual risk behaviours, chaotic injecting behaviour, home production, younger ages and morefrequent treatment utilisation. Stimulant injectors should have easy access to large volumes ofsterile injection equipment and means of sexual protection, requiring liberal exchange anddistribution policies, extended opening hours and, where needed, outreach activities in injectingand sexual risk environments (Beek et al., 2001; Des Jarlais et al., 2009). Proper injection kitsshould include a range of materials based on local assessment of drug use patterns and thesocial situation of injectors. One-for-one syringe exchange policies, still in place in variousneedle and syringe programmes (NSPs) in the EU and Eastern Europe, should be avoided dueto the high frequency of stimulant injection.Harm reduction materials
Collage: Jean-Paul Grund. Source images: Exchange Supplies.Harm reduction kits for injecting drug users may include needles and syringes, disinfectants, alcohol pads, ascorbic orcitric acid, filters, single-use cookers, plasters and antibiotic ointments, as well as educational materials. Sometimes otherspecific (e.g. for home preparation in CEE) or generic (such as vitamins or food) items are included as well.
204
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
Longer opening hours for NSPs and liberal exchange policies, political activism and publicfunding are associated with higher coverage of IDU populations and lower rates of riskbehaviour (Templaski et al., 2008; Bluthenthal et al., 2007a; Bluthenthal et al., 2007b).Increased coverage was followed by substantial reductions in HIV prevalence and incidenceamong IDUs in the United States (Santibanez et al., 2006). Exchange Supplies in the UnitedKingdom offers syringes with coloured plungers and ‘syringe-IDs’ (a little colour- and pattern-marked clip for the back of the plunger), developed to allow stimulant injectors in particularto distinguish their personal syringe when injecting collectively (see illustration above).In response to home-made stimulants, some NSPs in Eastern Europe offer syringes both forinjecting and for preparing drugs (Grund and Merkinaite, 2009). Harm reduction networks inGeorgia, Russia and Ukraine are developing interventions and information materials for home-made stimulant users. Distributing litmus paper to home-made stimulant users to allowproduction of less acidic drugs has been proposed but not yet implemented (Agafonova, 2008).Traditional harm reduction programmes may fail to reach problem stimulant users due toopiate-centered services and social barriers to young or female users (see e.g. Grund andMerkinaite, 2009). Outreach, secondary exchange, or peer-driven strategies are neededto reach those not attending established service programmes (Needle et al., 2005; Coyle etal., 1998; Des Jarlais et al., 2009; Wood et al., 2003; Grund et al., 1992a; Broadhead etal., 1998). An unsanctioned peer-based and all-night NSP, located on the street inVancouver’s open drug scene, was able to reach and deliver harm reduction services tothe city’s most at risk cocaine injectors (Wood et al., 2003). Syringe dispensing machines(SDMs) and mobile NSPs provide confidential access to sterile equipment at times andplaces where coverage is poor (Islam and Conigrave, 2007), to younger users (Moatti etal., 2001; Obadia et al., 1999) with shorter injection histories than NSP or pharmacy users,less drug dependence, less access to established services (Stark et al., 1994; Leicht, 1993),less licit income, and lower socioeconomic status (Moatti et al., 2001). Patrons of mobileoutlets are likely to be younger, indigenous and female, inject more frequently and do somore often on the street, be engaged in sex work and not be in drug treatment (Miller etal., 2002; Riley et al., 2000; Islam and Conigrave, 2007). SDMs are not advised as stand-alone interventions as there is little chance for health education, but they can serve asstrategic adjuncts to conventional NSPs and pharmacy distribution (Islam and Conigrave,2007; Agnoletto et al., 1993; Cox et al., 2000).Despite shifts towards smoking drugs in many EU countries, public health efforts remainalmost exclusively focused on IDU (Jauffret-Roustide, 2004; Jauffret-Roustide et al., 2008a;Haydon and Fischer, 2005; Cheung, 2000). Canada and several US programmes haveimplemented specific programmes for cocaine smokers (Boyd et al., 2008; Leonard et al.,2006; Leonard et al., 2007), such as the distribution of so-called ‘crack kits’, containingsupplies to prevent oral or respiratory lesions from smoking (Porter and Bonilla, 1993;Malchy et al., 2008; Collins et al., 2005). Studies of the out-of-treatment cocaine and heroinusers suggest that the principles and evidence base of needle exchange (Wodak andCooney, 2005; Hunt et al., 2003; Hunt et al., 2005; WHO, 2005; WHO et al. and UNODC,2004) may apply to crack kits or other drug use utensils as well (Grund, 1991a; Grund,1993; Pizzey and Hunt, 2008).205
Harm reduction: evidence, impacts and challenges
Although many supervised drug consumption facilities prohibit injected or smoked cocainedue to the chaotic and frenetic nature of use, several supervised injection facilities (SIFs) in theEU now include rooms for smoking cocaine and other drugs (Hunt, 2006), a trend that mayextend to Vancouver’s SIF (Shannon et al., 2006). Managing a smoking room has provensimilar to an injection room; SIFs that do allow cocaine use have not reported majorproblems (Poschadel et al., 2002; Verthein et al., 2001; Zurhold et al., 2001; Zurhold et al.,2003; Vogt and Zeissler, 2005; Broadhead et al., 2002; Poel, et al., 2003; Hedrich, 2004;IWGDCR, 2006). Programmes targeting smokers should emphasise women through gender-sensitive programmes that have been developed, although few of these have been evaluated(Boyd et al., 2008; Wechsberg et al., 2004; Butters and Erickson, 2003). Programming forwomen may work better when biological, behavioural, psychological and socialcharacteristics of women are considered and individual and community support measurescombined (Latka, 2003), supporting increased autonomy of women over their drug use andsexuality to minimise exposure to BBVs (Jauffret-Roustide et al., 2008b; Gollub, 2008).Sexually transmitted diseases, bacterial infections and other complicationsAmple supply of injection and sexual protection supplies may also contribute to reducingsexually transmitted diseases (STDs) and bacterial infections (Beek et al., 2001; Kerr et al.,2005). Proper injection techniques, antibacterial creams and ointments and rotation ofinjection sites may help reduce vein loss and effectively treat minor SSTIs (Stern, 1992). Basichygiene (hand washing, short nails) and vein care as well as simple wound care and trainingin safer injection may prevent infections in cocaine injectors (Beek et al., 2001; Kerr et al.,2005; Rhodes et al., 2007). Wound and abscess services within NSPs may increase patient–clinician interactions, providing opportunities for referrals to services such as HIV counselingand testing, medical care, and drug treatment at an estimated cost of $5 per patient (Grau etal., 2002). There is no consensus on whether groin injection should be actively discouragedor safer techniques provided (as in the United Kingdom; Maliphant and Scott, 2005; Zador,2007; Strang et al., 2008), although investigators agree that transitions to groin injection orcrack injection should be discouraged (Rhodes et al., 2007).Neurologic effectsEfforts to reduce the neurologic sequelae of stimulants are primarily related to the use of ‘clubdrugs’. Reducing frequency of use is the most common strategy for reducing the delayed‘comedown’ of stimulants, depression, and concerns about neurologic damage (Allott andRedman, 2006). ‘Pre-loading’ or ‘post-loading’ with a variety of substances is anotherapproach, involving vitamins, foods, antidepressant medications, sleeping tablets, or aminoacids. While there are no data evaluating the effect of these common methods (Kelly, 2009),a combination of amphetamines and most anti-depressant medications poses the risk of alife-threatening reaction known as serotonin syndrome (Copeland et al., 2006). A Dutchwebsite (http://www.cocaineinfo.nl/) provides neurological explanations for the ‘CokeShuffle’, advising temporary cessation of use, massage, a warm environment or a visit to thesauna, as this might help to reduce cramps. Sometimes benzodiazepines are prescribed toproblem cocaine users, mostly for sleep, but these may also alleviate joint and muscle pains.206
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
Cardiovascular effectsRoutine cardiovascular care, involving diet and exercise, management of high blood pressureand cholesterol, as well as reducing other risk factors such as tobacco use, are likely to bethe most powerful harm reduction strategies, as they are for the general population.Reducing dosage and frequency of all stimulant use may reduce cardiovascular toxicities, asmay reducing concomitant alcohol consumption. Although no controlled studies or specificinterventions have been conducted, patients maintained on amphetamines (Vitiello, 2008)and Andean users of low-potency coca products (Knuepfer, 2003) are believed to be at onlymild to moderately increased risk of cardiovascular toxicities. As cocaine is directly toxic toheart muscle cells while amphetamines exert toxicity primarily through blood pressureelevation, reducing or discontinuing use with onset of the cardiovascular disease that comeswith age is paramount to reducing the harm of these drugs.Pulmonary and other health effectsWhile marijuana can be filtered for some reduction in exposure to particulate matter(McPartland and Pruitt, 1997), filtering stimulant drugs is less likely to reduce the impact of thesedrugs on pulmonary tissue. Nonetheless, providing filters may reduce oropharyngeal exposureto hot embers, thus reducing burns to the mouth and throat. Harm reduction providers inCanada, and the United States offer ‘crack kits’ that include Pyrex pipes or rubber mouthpieces(Leonard et al., 2006; Leonard et al., 2007; Aidslaw, 2007), which may reduce lacerations tothe lips. Mainline in Amsterdam offered street cocaine smokers lung, blood and heartmeasurements, safer smoking advice and self-regulation training (Boekhout van Solinge, 2001),but roll-out of the methodology in mainstream drug services proved challenging (Bruin et al.,2008). Other strategies to reduce pulmonary damage could include vaporisation and othermeans to filter out talc and other particles. Sufficient hydration contributes to lip, skin and otherorgan health. The frequency of pneumonia might be mitigated by pneumococcal vaccinationand tuberculosis prevention, diagnosis and treatment.The American Dental Association has developed a patient folder on ‘meth mouth,’ that includesdrug treatment locators, a guide for parents and ‘a calculator to figure out how much it costs tosupport a drug habit’ (American Dental Association, 2005), but provides no advice on oralhygiene. Drug users in Amsterdam can get dental care at a special clinic and referrals toregular dentists. In Frankfurt in the 1990s, the Integrative Drogenhilfe was reportedly successfulin finding IDUs dentists in the community using case management and advocacy strategies, aspart of a ‘Vermittlung in die Normalität’ philosophy towards all their clients’ health, social andlegal problems (personal communication Marion Nickolai, 15 August 2009).OverdoseCocaine overdose is frequently cardiovascular (i.e. heart attack, fatal arrhythmia, or stroke)and demands rapid and sophisticated medical management. Concomitant use of opioids,alcohol or other depressant drugs is closely associated with cocaine overdose (Kaye andDarke, 2004), suggesting that limiting other drug use while using cocaine may reduce the risk207
Harm reduction: evidence, impacts and challenges
of overdose. Cardiopulmonary resuscitation delivered by bystanders has been demonstratedto improve outcomes in opioid overdose (Dietze et al., 2002) and may translate to stimulantoverdoses. Naloxone will not reverse a stimulant overdose, therefore ensuring rapid access tononjudgmental medical care without police intervention is essential to reducing fatalities.Mental health problemsMany mental health problems associated with stimulant use are dose, frequency and mode ofadministration related, and might be mitigated by specific harm reduction measures. Careproviders should use a sensitive, respectful approach toward stimulant users, even when chaotic,and treat people with signs of drug toxicity, such as cocaine-induced psychosis (Beek et al.,2001). Brief interventions among recreational amphetamine users should include informationabout potential mental health problems arising from regular use (Baker et al., 2004) and morethan weekly use or injection should be discouraged (Hall et al., 1996). A randomised-controlledtrial of Assertive Community Treatment for chronic crack users in Rotterdam found goodprogramme compliance and improvements in physical and mental health (Henskens, 2004).Cessation of cocaine injecting or smoking may be necessary for recovery from cocaine-relatedmental health morbidity (Beek et al., 2001), but self-regulation to control use may also provehelpful (Prinzleve et al., 2002; Haasen et al., 2005; Cramer and Schippers, 1994/1996).Stimulant users often self-medicate with heroin or other downers to control side-effects ofanxiety and irritability (Grund, 1993; Decorte, 2001). Acupuncture, while of little use asmonotherapy, may reduce cocaine craving when provided as an adjunct treatment (Gates etal., 2006; Kim et al., 2005) and the service may retain users in care (NTA, 2002). In New York,the Lower East Side Harm Reduction Center offers acupuncture, Reiki and other alternativetreatments to cocaine users (personal communication Raquel Algarin, 23 November 2009).Other practical suggestions for dealing with the behavioural peculiarities include immediateand flexible walk-in services (Haasen et al., 2003, Beek et al., 2001) and offering a calming,tranquil environment (Stöver, 2002), similar to ‘chill-out’ rooms at dance parties.‘Tagesruheräume’, or daytime rest rooms, for cocaine injectors and crack smokers have beenestablished in Frankfurt am Main and integrated within a low-threshold drug help centre,which offers counselling, medical and psychiatric care, a consumption room and a shelter inHamburg (Vogt et al., 2000; Stöver, 2001; Verthein et al., 2001). Organisations such as HITin Liverpool, Lifeline in Manchester and Mainline in Amsterdam have developed severalexplicit flyers for cocaine users with tips for managing mental health risks and controlling useof cocaine. While a focus of many programmes, approaches developed for stimulant usersare rarely published in the scientific literature.Pregnancy and parentingAn ethnographic evaluation of drug-using pregnant women demonstrated numerous self-employed harm reduction strategies, such as use of less dangerous substances (e.g.marijuana), reduced dose and frequency, and improved diet and self-care, as well as lesshelpful strategies like avoiding medical care for fear of stigma or prosecution (Kearney et al.,208
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
1995; Murphy and Rosenbaum, 1999). Long-term outcome data on early interventionprogrammes for cocaine-exposed children suggest that the impact of poverty farovershadows that of cocaine, and that early intervention can improve developmentaloutcomes (Kilbride et al., 2000). Furthermore, among cocaine-exposed children who do notreceive early interventions, remaining with their birth mothers may result in improved socialinteractions (Kilbride et al., 2006). Substantial harm reduction efforts around stimulants andpregnancy in North America have been legal defense and policy reform to reduce thecriminalisation of women’s behaviour during pregnancy (Lester et al., 2004).
DiscussionAppraisal of the quality of evidence reviewed and limitations of the studyResearch has established the rationale for many harm reduction interventions for stimulantusers (Wodak and Cooney, 2005; Farrell et al., 2005; Hunt et al., 2003; Hunt et al., 2005;WHO et al., 2004). Nonetheless, scientific literature is overwhelmingly weighted towardthe harms of stimulants, with minimal literature on harm reduction interventions.Investigations frequently consider stimulants users a subset, rather than the targetpopulation of a study. Several interventions for stimulant users, such as providing materialsfor safer crack smoking or safer groin injection training, remain controversial or illegal andthus systematic evaluations are lacking. Funding mechanisms for evaluating newinterventions are also limited, partly due to the reliance of most investigators on HIVfunding streams.Potential harms addressed by harm reduction interventionsThe effectiveness of pharmacological and psychosocial interventions for stimulant users islimited (De Lima et al., 2002; EMCDDA, 2007e; Pirona and Hedrich, 2009), thusinterventions to stabilise and minimise the negative consequences of ongoing stimulant useare of paramount importance. The evidence suggests that there are no fundamentalchallenges in adjusting regular harm reduction interventions, such as NSPs and SIFs, towardsBBV prevention among problem stimulant users. However, a wide range of health and socialproblems associated with stimulant use are largely unaddressed by current services (e.g.specific harm reduction approaches to SSTIs have been developed but are not widelyimplemented (Grau et al., 2002; Kerr et al., 2005)).Prevention of SSTIs, overdose or pulmonary, neurologic, or cardiovascular damage is arelatively new focus in harm reduction and there is much ground to be gained in preventionand early treatment of these conditions. ‘Crack kits’ may prove useful in preventing certaininfections. Widely available SSTI, and cardiac primary care services, may lessen the burdenof disease. The rapidly expanding literature on overdose prevention programming (Sporerand Kral, 2007; Maxwell et al., 2006; Coffin et al., 2007; Coffin, 2008) suggests a need toextend the harm reduction philosophy even further. Innovative service development pairedwith critical evaluation is necessary in translating the successes of harm reduction towardsheroin to stimulant use.209
Harm reduction: evidence, impacts and challenges
Community-based research, programme evaluations and best practice examples underscorethe need for services that enhance the ability of stimulant users to manage their intake levels,chaotic behaviour and mental health problems. Several harm reduction programmesinformally aid stimulant users in money management, at times even holding clients’ benefitcheques until after a binge. At hundreds, if not thousands, of blogs and Internet discussionlists, users discuss stimulant and other drug use openly and in detail, including many of theharms discussed in this review, dietary advice and ‘street pharmacology’ approaches to self-regulation (e.g. ‘Harm Reduction for Stimulants’, http://www.drugs-forum.com/forum/archive/index.php/t-24802.html).Rhodes and colleagues reported what could be termed an epidemic of groin injecting.When groin injection becomes an ‘acceptable risk’ (Rhodes et al., 2006), one wonderswhat other risks have pushed the normalisation of this hazardous behaviour down theinjector’s ‘hierarchy of risk’ (Connors, 1992). Rhodes and colleagues not only pointtowards increasing crack/speedball injection in their explanation, they also emphasise thechanging ‘risk environment’ of drug injecting (Rhodes, 2002). Groin injection is reportedlyviewed as ‘reliable, speedy, and discreet’. As one of their respondents explained, ‘you cando it under a camera’ (Rhodes et al., 2006). The omnipresence of camera and humansurveillance, zero tolerance towards deviance in the public space and the resulting lack ofspaces where homeless IDUs could withdraw to inject in British (and other) cities can thusbe seen to engender a risk environment in which ‘macro risk factors’ synergise the risks ofcrack injection towards aggravating injecting-related harm (Rhodes, 2002; Rhodes et al.,2006; Rhodes, 2009). Such environmental factors are mostly beyond the scope of harmreduction interventions, which focus primarily on the substance and its users. Nonetheless,in the early 1980s, when cocaine landed in the urban heroin scenes of the Netherlandsand injecting was still the dominant mode of drug administration, IDUs did not turn ‘enmasse’ towards groin injecting (Grund et al., 1991b). Instead, smoking cocaine at ‘houseaddresses’ became the norm (Grund et al., 1991a; Grund and Blanken, 1993; Blanken etal., 1997).The harms associated with problem stimulant use interact at multiple levels in the riskenvironment (Rhodes, 2002; Zinberg, 1984). Not only can specific harms influence oneanother, but they are also aggravated by external factors, such as international druglegislation, policing and other public policies in a process of ‘contingent causality’ (Rhodes,2009). Developing proper and timely responses to such policy-related harms is a crucialchallenge to harm reduction. Not because the proper harm reduction tools are absent orcannot be imagined, but because the larger risk environment might make such efforts nulland void (Grund et al., 1992b; Rhodes et al., 2006; Gostin, 1998). Policymakers shouldtherefore find ways to reduce the harms from counter-effective drug policies, harsh socialpolicies and policies affecting our public space and private behaviours, and strengthen theability of drug consumers and society to learn from past experience.History is full of examples of the acculturation of ‘new’ psychoactive drugs across variouscultures. As part of the mainstream social fabric, most drinking is restrained by explicit andimplicit social rules passed from generation to generation. Unfortunately, the collectiveknowledge on cocaine and amphetamines is accumulated through peer-based learning and210
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
not necessarily passed on automatically to new generations of users. The potential to respondin a rational and healthy fashion to ‘new’ illicit drugs is — among users and policymakersalike — hampered by what Lloyd Johnston termed ‘generational forgetting’ (Johnston et al.,2004). Yet, this learning is crucial to peacefully controlling problem drug use, a role recentlyadopted by harm reduction providers in many countries.Implications for future intervention development, research and policyThere is a strong base of needle exchange programming in many, but not all, EU MemberStates, but their coverage of the IDU population may vary and stimulant users are poorlyreached. Developing sufficient coverage for NSP and other interventions is a clear butcomplex issue (Des Jarlais et al., 2009) (see Kimber et al., 2010). Therefore, internal andexternal regulatory barriers, such as one-for-one exchange policies and laws that impedeharm reduction programmes from distributing other safer use supplies (e.g. crack pipes andsmoking foil) should be reconsidered. While returning used injecting equipment should beencouraged, the strict combination of distribution and collection is an unsavoury choice as ithinders access to ample quantities of injecting equipment at places and times when these aremost needed. Therefore, independent distribution and collection schemes should bedeveloped (Des Jarlais et al., 2009; Wood et al., 2003; Grund et al., 1992a).The volume of injection equipment or condoms provided to clients should be determinedbased on a thorough assessment of clients’ needs and network characteristics (Braine et al.,2008; Friedman et al., 2007; Rothenberg, 2007). All this requires a paradigm shift in serviceprovision — from institutional provider–client relationships to facilitation of peer prevention inuser networks (Broadhead et al., 1998) through peer-based outreach and secondaryexchange. Syringe vending machines and mobile programmes can be useful adjuncts to‘reaching the unreached’ but should be firmly based in flexible, attractive and human-delivered services.Safer injecting and smoking education and interventions supporting transition to lessharmful routes of drug administration, as well as overdose prevention and medical care ofvein, skin and other infections should become standard features of SIFs and NSPs, andmoved into the mainstream of harm reduction. NSPs and SIFs should not only create ahealthy atmosphere, but also a setting that allows for the pleasurable effects of stimulantswhile minimising negative experiences, possibly by emphasising more controlled and lessfrenetic use. Relaxation techniques and alternative therapies may help stimulant users toameliorate some of the mental health effects of heavy or frequent stimulant use, as well asphysical complaints such as musculoskeletal pain. Offering sleep and day rest facilitiesmay help to reduce sleep deprivation, which may alleviate the mental health strain ofstimulant use. Involving participants in service provision and other activities may furtherhelp reduce the frequency and amounts of stimulant use, potentially leading toimprovements in mental health and social functioning. Collaborations between variousmedical specialties, drug users, service providers and researchers in designing harmreduction strategies towards the pulmonary, cardiovascular and neurologic effects ofstimulant use are equally important.211
Harm reduction: evidence, impacts and challenges
The reviewed studies suggest that problem stimulant use requires innovative, integratedand multidisciplinary medical and social services, but also drug and social policies thatdo not exacerbate the already considerable potential for harm of stimulants. The recentattention being paid to the unintended consequences of drug policy at UNODC isencouraging, but needs to be translated into effective action. At present, internationaldrug and other public policies emphasise maximising harm to reduce casual drug use.Stimulant and other drug users must enjoy the fundamental human right to healthprotection, as stipulated by Article 25 of the Universal Declaration of Human Rights(General Assembly of the United Nations, 1948). In 1945, at the brink of war and peace,Sir Karl Popper published his influentialThe open society and its enemies,in which hewrote ‘The role of the state is not to make people happy but to relieve avoidablesuffering.’ For the state and its agents to live up to these calls is amongst the principalchallenges of harm reduction.
AcknowledgementsThe authors would like to gratefully acknowledge Gaelle Guibert and Marc Rondy forconducting parts of the crack literature review for this paper. We thank David Otiashvili andSimona Merkinaite for support with Russian-language literature and Floor van Bakkum, MikaMikkonen, Shona Shoning and Allan Clear for their help with finding information on variousspecific topics. We thank Mariette Baas and Lila Oudaya for their assistance in preparingthis manuscript.
Further readingBeek, I. van, Dwyer, R. and Malcom, A. (2001), ‘Cocaine injecting: the sharp end of drug related harm’,Drugand Alcohol Review20, 333–42.Bertol, E., Trignano, C., Di Milia, M. G., Di Padua, M. and Mari, F. (2008), ‘Cocaine-related deaths: an enigmastill under investigation’,Forensic Science International7 Apr, 176 (2–3), pp. 121–3.Darke, S., Kaye, S., McKetin, R. and Duflou, J. (2008), ‘Major physical and psychological harms ofmethamphetamine use’,Drug and Alcohol Review27, pp. 253–62.EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2007),Treatment of problem cocaine use:a review of the literature,EMCDDA, Lisbon.EMCDDA (2008),Treatment of problem cocaine use: a short update,EMCDDA, Lisbon.Karch, S. B. (2005), ‘Cocaine cardiovascular toxicity’,Southern Medical JournalAugust, 98 (8), pp. 794–9.Leonard, L., DeRubeis, E., Pelude, L., et al. (2007), ‘“I inject less as I have easier access to pipes”: injecting, andsharing of crack-smoking materials, decline as safer crack-smoking resources are distributed’,International Journalof Drug Policy19 (3), pp. 1–10.Pates, R. and Riley, D. (2009),Interventions for amphetamine misuse,Wiley-Blackwell, Oxford.Scheinmann, R., Hagan, H., Lelutiu-Weinberger, C., et al. (2007), ‘Non-injection drug use and hepatitis C virus: asystematic review’,Drug and Alcohol Dependence89, pp. 1–12.
212
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
ReferencesAddis, A., Moretti, M. E., Ahmed Syed, F., Einarson, T. R. and Koren, G. (2001), ‘Fetal effects of cocaine: anupdated meta-analysis’,Reproductive Toxicology15 (4), pp. 341–69.Adimora, A. A., Schoenbach, V. J., Martinson, F. E., et al. (2003), ‘Concurrent partnerships among rural AfricanAmericans with recently reported heterosexually transmitted HIV infection’,Journal of Acquired Immune DeficiencySyndromes34, pp. 423–9.Afonso, L., Mohammad, T. and Thatai, D. (2007), ‘Crack whips the heart: a review of the cardiovascular toxicityof cocaine’,American Journal of Cardiology100 (6), pp. 1040–3.Agafonova, A. (2008), ‘Report from the consultation meeting “Psychostimulants: harm reduction approaches”’,Russian Harm Reduction Network, Moscow.Agnoletto, V., Tradati, C., Ceserani, N., et al. (1998),Street work and needle exchange machines ascomplementary strategies of HIV harm reduction among active drug users: an Italian model(Abstract no. WS-D09-4),Int Conf AIDS,Berlin, Germany.Aidslaw (2007),Abolition du programme de trousses pour l’usage plus sûr du crack: un geste irresponsable et decourte visé’e, du Conseil municipal d’Ottawa(news release). Available at http://www.aidslaw.ca/publications/interfaces/downloadDocumentFile.php?ref=731 (accessed on 23 January 2010).Alcabes, P. (2009),Dread: how fear and fantasy have fueled epidemics from the Black Death to avian flu,PublicAffairs Books, New York.Allott, K. and Redman, J. (2006), ‘Patterns of use and harm reduction practices of ecstasy users in Australia’,Drugand Alcohol Dependence82 (2), pp. 168–76.American Dental Association (2005), ‘For the dental patient: methamphetamine use and oral health’. Available athttp://www.ada.org/prof/resources/pubs/jada/patient/patient_55.pdf (accessed on 30 September 2009).American Dental Association (2009), ‘Methamphetamine use (meth mouth)’. Available at http://www.ada.org/prof/resources/topics/methmouth.asp (accessed on 30 September 2009).American Psychiatric Association (2007), ‘Practice guideline for the treatment of patients with substance usedisorders’ (2nd edition),American Journal of Psychiatry164 (4) (Supplement), pp. 1–124.Baker, A., Lee, N. K., Claire, M., et al. (2004), ‘Drug use patterns and mental health of regular amphetamineusers during a reported “heroin drought”’,Addiction99, pp. 875–84.Balakireva, O. M., Grund, J. P. C., Barendregt, C., et al. (2006),Risk and protective factors in the initiation ofinjecting drug use: analytical report on a respondent driven sampling study and strategy paper preventing theinitiation of injecting drug use among vulnerable adolescents and young people: final report,UNICEF/UISR,Kiev.Basso, M. R. and Bornstein, R. A. (2000), ‘Neurobehavioural consequences of substance abuse and HIVinfection’,Journal of Psychopharmacology14 (3), pp. 228–37.Bauman, J. L. and DiDomenico, R. J. (2002), ‘Cocaine-induced channelopathies: emerging evidence on themultiple mechanisms of sudden death’,Journal of Cardiovascular Pharmacology and Therapeutics7 (3), pp.195–202.Bauwens, J. E., Orlander, H., Gomez, M. P., et al. (2002), ‘Epidemic Lymphogranuloma venereum duringepidemics of crack cocaine use and HIV infection in the Bahamas’,Sexually Transmitted Diseases29, pp. 253–9.
213
Harm reduction: evidence, impacts and challenges
Beek, I. van, Dwyer, R., and Malcom, A. (2001), ‘Cocaine injecting: the sharp end of drug related harm’,Drugand Alcohol Review20, 333–42.Bellis, M., Hughes, K., Bennett, A. and Thomson, R. (2003), ‘The role of an international nightlife resort in theproliferation of recreational drugs’,Addiction98, pp. 1713–21.Binswanger, I. A., Kral, A. H., Bluthenthal, R. N., Rybold, D. J. and Edlin, B. R. (2000), ‘High prevalence ofabscesses and cellulitis among community-recruited injection drug users in San Francisco’,Clinical InfectiousDiseases30, pp. 579–81.Blanken, P., Barendregt, C., and Hendriks, V. (1997),Op is op. Niets is voor altijd. Een onderzoek naar het rokenvan cocaïne-base en zelf-controle mechanismen (IVO-reeks nr. 14),IVO, Rotterdam.Bluthenthal, R., Anderson, R., Flynn, N. and Kral, A. (2007a), ‘Higher syringe coverage is associated with lowerodds of HIV risk and does not increase unsafe syringe disposal among syringe exchange program clients’,Drugand Alcohol Dependence89, pp. 214–22.Bluthenthal, R., Ridgeway, G., Schell, T., et al. (2007b), ‘Examination of the association between syringeexchange program (SEP) dispensation policy and SEP client-level syringe coverage among injection drug users’,Addiction102, pp. 638–46.Boekhout van Solinge, T. (2001),Op de pof,Rozenberg, Amsterdam.Booth, R., Lehman, W., Kwiatkowski, C., et al. (2008), ‘Stimulant injectors in Ukraine: the next wave of theepidemic?’AIDS and Behaviour,12 (4), pp. 652–61.Borodkina, O. I., Baranova, M. V., Girchenko, P. V., et al. (2005), ‘The correlation between the type of drug useand HIV prevalence of IDU in different Russian cities’,Russian Journal of HIV/AIDS and Related Problems9 (3), pp.74–5.Boyd, S., Johnson, J. L. and Moffat, B. (2008), ‘Opportunities to learn and barriers to change: crack cocaine usein the Downtown Eastside of Vancouver’,Harm Reduction Journal5, p. 34.Braine, N., Acker, C., Goldblatt, C., Yi, H., Friedman, S. R., and Des Jarlais, D. C. (2008), ‘Neighborhoodhistory as a factor shaping syringe distribution networks among drug users at a U.S. syringe exchange’,Soc Netw30 (3), pp. 235–46.Brewer, T. H., Zhao, W., Pereyra, M., et al. (2007), ‘Initiating HIV care: attitudes and perceptions of HIV positivecrack cocaine users’,AIDS and Behavior11 (6), pp. 897–904.Broadhead, R. S., Heckathorn, D. D., Weakliem,D. L., et al. (1998), ‘Harnessing peer networks as an instrumentfor AIDS prevention: results from a peer-driven intervention’, in Needle, R. H., Coyle, S. and Cesari, H. (eds), ‘HIVprevention with drug-using populations: current status and future prospects’,Public Health Reports113 (Supplement1), pp. 42–57.Broadhead, R. S., Altice, F. L., Kerr, T. H. and Grund, J-P. C. (2002), ‘Safer injection facilities in North America:their place in public policy and health initiatives’,Journal of Drug Issues32 (7), pp. 327–54.Bruin, D. de, Ossebaard, H., Bakker, I., Aalderen, H. van and Wildschut, J. (2008), ‘Hoezo onbereikbaar?Passende hulp voor basecokegebruikers: knelpunten en kansen’,Verslaving, Tijdschrift over Verslavingsproblematiek4, no. 1.§.Butters, J. and Erickson, P. G. (2003), ‘Meeting the health care needs of female crack users: a Canadianexample’,Women and Health37, pp. 1–17.Cabral, G. A. (2006), ‘Drugs of abuse, immune modulation, and AIDS’,Journal of Neuroimmune Pharmacology1(3), pp. 280–95.
214
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
Cadet, J. L. and Krasnova, I. N. (2007), ‘Interactions of HIV and methamphetamine: cellular and molecularmechanisms of toxicity potentiation’,Neurotoxicity Research12 (3), pp. 181–204.Callaway, C. W. and Clark, R. F. (1994), ‘Hyperthermia in psychostimulant overdose’,Annals of EmergencyMedicine24 (1), pp. 68–76.Camilleri, A. M. and Caldicott, D. (2005), ‘Underground pill testing, down under’,Forensic Science International151 (1), pp. 53–8.Campsmith, M. L., Nakashima, A. K. and Jones, J. L. (2000), ‘Association between crack cocaine use and high-risk sexual behaviours after HIV diagnosis’,Journal of Acquired Immune Deficiency Syndromes25, pp. 192–8.Castells, X., Casas, M., Vidal, X. et al. (2007), ‘Efficacy of central nervous stimulant treatment for cocainedependence: a systematic review and meta-analysis of randomized controlled clinical trials’,Addiction102 (12),pp. 1871–87.Celentano, D. D., Valleroy, L. A., Sifakis, F., et al. (2006), ‘Associations between substance use and sexual riskamong very young men who have sex with men’,Sexually Transmitted Diseases33 (4), pp. 265–71.Centers for Disease Control and Prevention (1991), ‘Alternative case-finding methods in a crack-related syphilisepidemic: Philadelphia’,Morbidity and Mortality Weekly Report40, pp. 77–80.Centers for Disease Control and Prevention (1993), ‘Selective screening to augment syphilis case-finding —Dallas, 1991’,Morbidity and Mortality Weekly Report42, pp. 424–7.Centers for Disease Control and Prevention (1996), ‘Continued sexual risk behaviour among HIV-seropositive,drug-using men — Atlanta, Washington, D.C., and San Juan, Puerto Rico, 1993’,Morbidity and Mortality WeeklyReport45, pp. 151–2.Chang, L., Alicata, D., Ernst, T. and Volkow, N. (2007), ‘Structural and metabolic brain changes in the striatumassociated with methamphetamine abuse’,Addiction102 (Supplement 1), pp. 16–32.Chao, C., Jacobson, L. P., Tashkin, D., et al. (2008), ‘Recreational drug use and T lymphocyte subpopulations inHIV-uninfected and HIV-infected men’,Drug and Alcohol Dependence94 (1–3), pp. 165–71.Chen, C. K., Lin, S. K., Sham, P. C., et al. (2003), ‘Pre-morbid characteristics and co-morbidity ofmethamphetamine users with and without psychosis’,Psychological Medicine33 (8), pp. 1407–14.Cheung, Y. W. (2000), ‘Substance abuse and developments in harm reduction’,Canadian Medical AssociationJournal162, pp. 1697–700.Chi, D. and Milgrom, P. (2008), ‘The oral health of homeless adolescents and young adults and determinants oforal health: preliminary findings’,Special Care Dentistry28 (6), pp. 237–42.Chiasson, M. A., Stoneburner, R. L., Hildebrandt, D. S., et al. (1991), ‘Heterosexual transmission of HIV-1associated with the use of smokable freebase cocaine (crack)’,AIDS5, pp. 1121–6.Chintalova-Dallas, R., Case, P., Kitsenko, N. and Lazzarini, Z. (2009), ‘Boltushka: a homemade amphetamine-type stimulant and HIV risk in Odessa, Ukraine’,International Journal of Drug Policy20, pp. 347–51.Chirgwin, K., DeHovitz, J. A., Dillon, S. and McCormack, W. M. (1991), ‘HIV infection, genital ulcer disease, andcrack cocaine use among patients attending a clinic for sexually transmitted diseases’,American Journal of PublicHealth81, pp. 1576–9.Ciccarone, D. and Bourgois, P. (2003), ‘Explaining the geographical variation of HIV among injection drug usersin the United States’,Substance Use and Misuse38, pp. 2049–63.
215
Harm reduction: evidence, impacts and challenges
Ciccarone, D., Bamberger, J., Kral, A., et al. (2001), ‘Soft tissue infections among injection drug users: SanFrancisco, California, 1996–2000’,Morbidity and Mortality Weekly Report50 (19), pp. 381–84.Cleghorn, F.R., Jack, N., Murphy, J.R. et al. (1995), ‘HIV-1 prevalence and risk factors among sexually transmitteddisease clinic attenders in Trinidad’,AIDS9, pp. 389–94.Coffin, P. (2008),Overdose: a major cause of preventable death in central and eastern Europe and central Asia,Eurasian Harm Reduction Network, Vilnius.Coffin, P. O., Galea, S., Ahern, J., et al. (2003), ‘Opiates, cocaine and alcohol combinations in accidental drugoverdose deaths in New York City, 1990–98’,Addiction98 (6), pp. 739–47.Coffin, P. O., Tracy, M., Bucciarelli, A., et al. (2007), ‘Identifying injection drug users at risk of nonfataloverdose’,Academic Emergency Medicine14 (7), pp. 616–23.Cofrancesco, J. Jr., Scherzer, R., Tien, P. C., et al. (2008), ‘Illicit drug use and HIV treatment outcomes in a UScohort’,Aids22 (3), pp. 357–65.Cohen, A. L., Shuler, C., McAllister, S., et al. (2007), ‘Methamphetamine use and methicillin-resistantstaphylococcus aureus skin infections’,Emerging Infectious Diseases13 (11), pp. 1707–13.Cohen, P. and Sas, A. (1993),Ten years of cocaine: a follow-up study of 64 cocaine users in Amsterdam,Department of Human Geography, Universiteit van Amsterdam, Amsterdam, pp. 1–126.Cohen, P. and Sas, A. (1994), ‘Cocaine use in Amsterdam in non deviant subcultures’,Addiction Research2 (1),pp. 71–94.Cole, J. C., Sumnall, H. R., Smith, G. W. and Rostami-Hodjegan, A. (2005), ‘Preliminary evidence of thecardiovascular effects of polysubstance misuse in nightclubs’,Journal of Psychopharmacology19 (1), pp. 67–70.Collins, C. L., Kerr, T., Tyndall, M. W. S., et al. (2005), ‘Rationale to evaluate medically supervised safer smokingfacilities for non-injection illicit drug users’,Canadian Journal of Public Health96, pp. 344–7.Connors, M. M. (1992), ‘Risk perception, risk taking and risk management among intravenous drug users:implications for AIDS prevention’,Social Science and Medicine34 (6), pp. 591–601.Cook, J. A., Burke-Miller, J. K., Cohen, M. H., et al. (2008), ‘Crack cocaine, disease progression, and mortalityin a multicenter cohort of HIV-1 positive women’,Aids22 (11), pp. 1355–63.Cook, J. A., Grey, D. D., Burke-Miller, J. K., et al. (2007), ‘Illicit drug use, depression and their association withhighly active antiretroviral therapy in HIV-positive women’,Drug and Alcohol Dependence89 (1), pp. 74–81.Copeland, J., Dillon, P. and Gascoigne, M. (2006), ‘Ecstasy and the concomitant use of pharmaceuticals’,Addictive Behaviours31 (2), pp. 367–70.Cotten-Oldenburg, N. U., Jordan, B. K., Martin, S. L. and Kupper, L. (1999), ‘Women inmates’ risky sex and drugbehaviours: are they related?’American Journal of Drug and Alcohol Abuse25, pp. 129–49.Cox, G., Lawless, M., Cassin, S. P. and Geoghegan, T. W. (2000), ‘Syringe exchanges: a public health responseto problem drug use’,Irish Medical Journal93 (5), pp. 143–6.Coyle, S. L., Needle, R. H. and Normand, J. (1998), ‘Outreach based HIV prevention for injecting drug users: areview of published outcome data’, in Needle, R. H., Coyle, S. and Cesari, H. (eds),HIV prevention with drug-using populations: current status and future prospects,Public Health Reports, 113 (Supplement 1), pp. 19–30.Cramer, E. A. S. M. and Schippers, G. M. (1994/1996),Zelfcontrole en ontwenning van harddrugs, Eindrapportvan een onderzoek naar de ontwikkeling en evaluatie van een zelfcontrole programma voor druggebruikers,Nijmegen: UNRAB.
216
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
Crowe, A. V., Howse, M., Bell, G. M. and Henry, J. A. (2000), ‘Substance abuse and the kidney’,QJM93 (3),pp. 147–52.Daley, D. C., Mercer, D. and Carpenter, G. (2002),Drug counseling for cocaine addiction: the collaborativecocaine treatment study model,National Institute on Drug Abuse, Bethesda, Maryland.Darke, S., Kaye, S., McKetin, R. and Duflou, J. (2008), ‘Major physical and psychological harms ofmethamphetamine use’,Drug and Alcohol Review,pp. 253–62.De, P., Cox, J., Boivin, J. F., Platt, R. W. and Jolly, A. M. (2007), ‘Rethinking approaches to risk reduction forinjection drug users: differences in drug type affect risk for HIV and hepatitis C virus infection through drug-injecting networks’,Journal of Acquired Immune Deficiency Syndromes46 (3), pp. 355–61.De Lima, M. S., De Oliviera Soares, B. G., Reisser, A., et al. (2002), ‘Pharmacological treatment of cocainedependence: a systematic review’,Addiction97 (8), pp. 931–49.De Letter, E. A., Piette, M. H., Lambert, W. E. and Cordonnier, J. A. (2006), ‘Amphetamines as potential inducersof fatalities: a review in the district of Ghent from 1976–2004’,Medicine, Science and the Law46 (1), pp. 37–65.Decorte, T. (2001),The taming of cocaine: cocaine use in European and American cities,VUB University Press,Brussel.Degenhardt, L., Mathers, B., Guarinieri, M. , Panda, S., Phillips, B., Strathdee, S. A., Tyndall, M., Wiessing, L.,Wodak, A., Howard, J., on behalf of the Reference Group to the United Nations on HIV and injecting drug use(2010), ‘Meth/amphetamine use and associated HIV: Implications for global policy and public health’, (correctedproof, 01 February 2010),International Journal of Drug Policy,21, DOI: 10.1016/j.drugpo.2009.11.007.Derauf, C., Lagasse, L. L., Smith, L. M., et al. (2007), ‘Demographic and psychosocial characteristics of mothersusing methamphetamine during pregnancy: preliminary results of the infant development, environment, andlifestyle study (IDEAL)’,American Journal of Drug and Alcohol Abuse33 (2), pp. 281–9.Des Jarlais, D. C., Grund J-P. C., Zadoretzky, C., et al. (2002), ‘HIV risk behaviour among participants of syringeexchange programmes in central/eastern Europe and Russia’,International Journal of Drug Policy13, pp. 165–74.Des Jarlais, D. C., McKnight, C., Goldblatt, C. and Purchase, D. (2009), ‘Doing harm reduction better: syringeexchange in the United States’,Addiction,104 (9), pp. 1441–6.Dietze, P., Cantwell, K. and Burgess, S. (2002), ‘Bystander resuscitation attempts at heroin overdose: does itimprove outcomes?’,Drug and Alcohol Dependence67 (2), pp. 213–18.Downes, M. A. and Whyte, I. M. (2005), ‘Amphetamine-induced movement disorder’,Emergency MedicineAustralia17, pp. 277–80.Draper, E. S., Rankin, J. and Tonks, A. M., et al. (2008), ‘Recreational drug use: a major risk factor forgastroschisis?’,American Journal of Epidemiology167 (4), pp. 485–91.Dutra, L., Stathopoulou, G., Basden, S. L., et al. (2008), ‘A meta-analytic review of psychosocial interventions forsubstance use disorders’,American Journal of Psychiatry165 (2), pp. 179–87.Edlin, B. R., Irwin, K. L., Ludwig, D. D., et al. (1992), ‘High-risk sex behaviour among young street-recruited crackcocaine smokers in three American cities: an interim report’, The Multicenter Crack Cocaine and HIV InfectionStudy Team,Journal of Psychoactive Drugs24, pp. 363–71.Edlin, B. R., Irwin, K. L., Faruque, S., et al.(1994), ‘Intersecting epidemics: crack cocaine use and HIV infectionamong inner-city young adults’, Multicenter Crack Cocaine and HIV Infection Study Team,New England Journal ofMedicine331, pp. 1422–7.
217
Harm reduction: evidence, impacts and challenges
Elkashef, A., Vocci, F., Hanson, G., et al. (2008), ‘Pharmacotherapy of methamphetamine addiction: an update’,Substance Abuse29 (3), pp. 31–49.EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2007a),Annual report 2007: highlights,Figure 7. Available at http://www.emcdda.europa.eu/html.cfm/index42367EN.html (accessed on 19 July 2009).EMCDDA (2007b), Statistical bulletin, Figure GPS-13. Available at http://www.emcdda.europa.eu/stats09/gpsfig13 (accessed on 19 July 2009).EMCDDA (2007c), Statistical bulletin, Table PDU-2. Available at http://www.emcdda.europa.eu/stats07/pdutab02b (accessed on 19 July 2009).EMCDDA (2007d), Statistical bulletin 2007. Available at http://www.emcdda.europa.eu/stats07/GPS (accessedon 19 July 2009).EMCDDA (2007e),Treatment of problem cocaine use: a review of the literature,EMCDDA, Lisbon. Available athttp://www.emcdda.europa.eu/html.cfm/index40152EN.html (accessed on 17 December 2009).EMCDDA (2007f),Cocaine and crack cocaine: a growing public health issue,EMCDDA, Lisbon. Available athttp://www.emcdda.europa.eu/html.cfm/index44746EN.html (accessed on 23 January 2010).EMCDDA (2008),Annual report.Available at http://www.emcdda.europa.eu/publications/annual-report/2008(accessed on 19 July 2009).EMCDDA (2009), Statistical bulletin 2009. Available at http://www.emcdda.europa.eu/stats09/gps (accessedon 19 July 2009).Farre, M., De La Torre, R., Gonzalez, M. L., et al. (1997), ‘Cocaine and alcohol interactions in humans:neuroendocrine effects and cocaethylene metabolism’,Journal of Pharmacology and Experimental Therapeutics283 (1), pp. 164–76.Farrell, M., Marsden, J., Ling, L., Ali, R. and Gowing, L. (2005),Effectiveness of drug dependence treatment inpreventing HIV among injecting drug users: evidence for action technical paper,World Health Organization,Geneva.Faruque, S., Edlin, B. R., McCoy, C. B., et al. (1996), ‘Crack cocaine smoking and oral sores in three inner-cityneighborhoods’,Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology13, pp. 87–92.Ferris, M. J., Mactutus, C. F. and Booze, R. M. (2008), ‘Neurotoxic profiles of HIV, psychostimulant drugs ofabuse, and their concerted effect on the brain: current status of dopamine system vulnerability in NeuroAIDS’,Neuroscience and Behavioural Reviews32 (5), pp. 883–909.Finelli, L., Budd, J. and Spitalny, K.C. (1993), ‘Early syphilis: relationship to sex, drugs, and changes in high-riskbehaviour from 1987–1990’,Sexually Transmitted Diseases20, pp. 89–95.Fischer, B., Rehm, J., Patra, J., et al. (2006), ‘Crack across Canada: comparing crack users and crack non-users ina Canadian multi-city cohort of illicit opioid users’,Addiction101, pp. 1760–70.Fischer, B., Powis, J., Firestone, C. M., Rudzinski, K. and Rehm, J. (2008), ‘Hepatitis C virus transmission amongoral crack users: viral detection on crack paraphernalia’,European Journal of Gastroenterology & Hepatology20,pp. 29–32.Fletcher, A., Calafat, A., Pirona, A. and Olszewski, D. (2010), ‘Young people, recreational drug use and harmreduction’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence,impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, PublicationsOffice of the European Union, Luxembourg.
218
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
Fleury, G., De La Garza, R., Mahoney, J. J., Evans, S. E. and Newton, T. F. (2008), ‘Predictors of cardiovascularresponse to methamphetamine administration in methamphetamine-dependent individuals’,American Journal onAddictions17 (2), pp. 103–10.Frank, D. A., Augustyn, M., Knight, W. G., Pell, T. and Zuckerman, B. (2001), ‘Growth, development, andbehavior in early childhood following prenatal cocaine exposure: a systematic review’,JAMA285 (12), pp.1613–25.Frieden, J. (2006), ‘Skin manifestations may signal crystal meth use: think “meth mites” when patients are pickingat their skin and think they have insects crawling on them’, Skin disorders,Family Practice News.Available athttp://www.accessmylibrary.com/coms2/summary_0286-12689367_ITM (accessed on 19 July 2009).Friedman, S. R., Flom, P. L., Kottiri, R., et al. (2003), ‘Drug use patterns and infection with sexually transmissibleagents among young adults in a high-risk neighbourhood in New York City’,Addiction98, pp. 159–69.Friedman, S. R., Bolyard, M. and Mateu-Gelabert, P. (2007), ‘Some data-driven reflections on priorities in AIDSnetwork research’,AIDS and Behaviour11 (5), pp. 641–51.Gates, S., Smith, L. A. and Foxcroft, D. R. (2006), ‘Auricular acupuncture for cocaine dependence’,CochraneDatabase of Systematic Reviews1, CD005192.General Assembly of the United Nations (1948),The Universal Declaration of Human Rights.Available at http://www.un.org/en/documents/udhr/.Gibson, D. R., Leamon, M. H. and Flynn, N. (2002), ‘Epidemiology and public health consequences ofmethamphetamine use in California’s Central Valley’,Journal of Psychoactive Drugs34, pp. 313–19.Glauser, J. and Queen, J. R. (2007), ‘An overview of non-cardiac cocaine toxicity’,Journal of Emergency Medicine32 (2), pp. 181–6.Gollub, E. L. (2008), ‘A neglected population: drug-using women and women’s methods of HIV/STI prevention’,AIDS Education and Prevention20, pp. 107–20.Golub, M., Costa, L., Crofton, K., et al. (2005), ‘NTP-CERHR Expert Panel Report on the reproductive anddevelopmental toxicity of amphetamine and methamphetamine’,Birth Defects Research Part B: Developmental andReproductive Toxicology74 (6), pp. 471–584.Goodkin, K., Shapshak, P., Metsch, L. R., et al. (1998), ‘Cocaine abuse and HIV-1 infection: epidemiology andneuropathogenesis’,Journal of Neuroimmune Pharmacology83 (1–2), pp. 88–101.Gostin, L. O. (1998), ‘The legal environment impeding access to sterile syringes and needles: the conflict betweenlaw enforcement and public health’,Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology18(Supplement 1), pp. S60–S70.Grabowski, J., Rhoades, H., Stotts, A., et al. (2004), ‘Agonist-like or antagonist-like treatment for cocainedependence with methadone for heroin dependence: two double-blind randomized clinical trials’,Neuropsychopharmacology29 (5), pp. 969–81.Grau, L.E., Arevalo, S., Catchpool, C., Heimer, R. for the Diffusion of Benefit through Syringe Exchange StudyTeam (2002), ‘Expanding harm reduction services through a wound and abscess clinic’,American Journal ofPublic Health92, pp. 1915–17.Griffiths, P., Mravcik, V., Lopez, D. and Klempova, D. (2008), ‘Quite a lot of smoke but very limited fire: the use ofmethamphetamine in Europe’,Drug and Alcohol Review27 (3), pp. 236–42.
219
Harm reduction: evidence, impacts and challenges
Gross, M., Holte, S. E., Marmor, M., et al. (2000), ‘Anal sex among HIV-seronegative women at high risk of HIVexposure’, The HIVNET Vaccine Preparedness Study 2 Protocol Team,Journal of Acquired Immune DeficiencySyndromes24, pp. 393–8.Grund, J-P. C. (1993),Drug use as a social ritual: functionality, symbolism and determinants of self-regulation,Addiction Research Institute (IVO), Rotterdam. Available at http://www.drugtext.org/library/books/grund01/grundcon.html.Grund, J-P. C. (2001), ‘A candle lit from both sides: the epidemic of HIV infection in central and eastern Europe’,in McElrath, K. (ed.),HIV and AIDS: a global view,Greenwood Press, Westport, CT.Grund, J-P. C. and Blanken, P. (1993),From ‘Chasing the dragon’ to ‘Chinezen’: the diffusion of heroin smoking in theNetherlands,Addiction Research Institute (IVO), Rotterdam. Available at http://www.drugtext.org/library/books/grund/CHASDRAG.html.Grund, J-P. C. and Merkinaite, S. (2009),Young people and injecting drug use in selected countries of Central andEastern Europe,Young IDUs Working Group, EHRN, Vilnius.Grund, J-P.C., Adriaans, N.F.P. and Kaplan, C.D. (1991a), ‘Changing cocaine smoking rituals in the Dutch heroinaddict population’,British Journal of Addiction86, pp. 439–48.Grund, J-P. C., Kaplan, C. D. and Adriaans, N. F. P. (1991b), ‘Needle sharing in the Netherlands: anethnographic analysis’,American Journal of Public Health81, pp. 1602–07.Grund, J-P. C., Blanken, P., Adriaans, N. F. P., et al. (1992a), ‘Reaching the unreached: targeting hidden IDUpopulations with clean needles via known users’,Journal of Psychoactive Drugs24 (1), pp. 41–7.Grund, J-P. C., Stern, L. S., Kaplan, C. D., Adriaans, N. F. P. and Drucker, E. (1992b), ‘Drug use contexts andHIV-consequences: the effect of drug policy on patterns of everyday drug use in Rotterdam and the Bronx’,BritishJournal of Addiction87, pp. 381–92.Grund, J-P. C., Öfner, P. J. and Verbraeck, H. T. (2007a),Marel o Del, kas kamel, le Romes duvar (God hits whomhe chooses, the Rom gets hit twice): an exploration of drug use and HIV risks among the Roma of central and easternEurope,L’Harmattan, Budapest.Grund, J-P. C., Reinerie, P., Smits, M. and Albert, G. (2007b), ‘Uitgaan en genotmiddelengebruik in Den Haag:gegevens over 2006–2007 uit de panelstudie’,Epidemiologisch Bulletin42 (4), pp. 2–10. Available at http://www.denhaag.nl/Docs/ocw/GGD/Epibul/Epi%20nr%204%202007.pdf.Grund, J-P.C., Zabransky, T., Irwin, K. and Heimer R. (2009), ‘Stimulant use in central and eastern Europe: howrecent social history shaped current drug consumption patterns’, in Pates, R. and Riley, D. (eds),Interventions foramphetamine misuse,Wiley Blackwell, Oxford.Guerot, E., Sanchez, O., Diehl, J. L. and Fagon, J. Y. (2002), ‘Acute complications in cocaine users’,Ann MedInterne(Paris) 153 (3 Supplement), pp. 1S27–31.Gyarmathy, V. A., Neaigus, A., Miller. M., Friedman, S. R. and Des, J. (2002), ‘Risk correlates of prevalent HIV,hepatitis B virus, and hepatitis C virus infections among noninjecting heroin users’,Journal of Acquired ImmuneDeficiency Syndromes30, pp. 448–56.Haasen, C., Prinzleve, M., Zurhold, H., et al. (2003),Support needs for cocaine and crack users in Europe,Zentrum für Interdisziplinäre Suchtforschung, Hamburg.Haasen, C., Prinzleve, M., Zurhold, H., et al. (2004), ‘Cocaine use in Europe: a multi-centre study’,EuropeanAddiction Research,10 (4), pp. 139–46.
220
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
Haasen, C., Prinzleve, M., Gossop, M., et al. (2005), ‘Relationship between cocaine use and mental healthproblems in a sample of European cocaine powder or crack users,’World Psychiatry4, pp. 173–6.Hagan, H., Thiede, H. and Des Jarlais, D. C. (2005), ‘HIV/hepatitis C virus co-infection in drug users: riskbehaviour and prevention’,AIDS19 (Supplement 3), pp. S199–S207.Haigney, M. C., Alam, S., Tebo, S., et al. (2006), ‘Intravenous cocaine and QT variability’,Journal ofCardiovascular Electrophysiology17 (6), pp. 610–16.Hall, W. and Carter, L. (2004), ‘Ethical issues in using a cocaine vaccine to treat and prevent cocaine abuse anddependence’,Journal of Medical Ethics30 (4), pp. 337–40.Hall, W., Hando, J., Darke, S. and Ross, J. (1996), ‘Psychological morbidity and route of administration amongamphetamine users in Sydney, Australia’,Addiction91, pp. 81–7.Hando, J., Flaherty, B. and Rutter, S. (1991), ‘An Australian profile on the use of cocaine’,Addiction92, pp. 173–82.Harris, L. H. and Paltrow, L. (2003), ‘Msjama: the status of pregnant women and fetuses in US criminal law’,JAMA289 (13), pp. 1697–9.Haverkos, H. W. and Steel, E. (1991), ‘Crack cocaine, fellatio, and the transmission of HIV’,American Journal ofPublic Health81, pp. 1078–9.Haydon, E., and Fischer, B. (2005), ‘Crack use as a public health problem in Canada: call for an evaluation of“safer crack use kits”’,Canadian Journal of Public Health96, pp. 185–8.Health Council of the Netherlands (2002),Pharmacotherapeutic interventions in drug addiction,Health Council ofthe Netherlands, The Hague, publication no. 2002/10.Hedetoft, C. and Christensen, H. R. (1999), ‘Amphetamine, ecstasy and cocaine: clinical aspects of acutepoisoning’,Ugeskr Laeger161 (50), pp. 6907–11.Hedrich, D. (2004),European report on drug consumption rooms,European Monitoring Centre for Drugs and DrugAddiction (EMCDDA), Portugal.Heffernan, R., Chiasson, M. A. and Sackoff, J. E. (1996), ‘HIV risk behaviours among adolescents at a sexuallytransmitted disease clinic in New York City’,Journal of Adolescent Health18, pp. 429–34.Heimer, R., Booth, R. E., Irwin, K. S. and Merson, M. H. (2007), ‘HIV and drug use in Eurasia’, in Twigg, J. L.(ed.),HIV/AIDS in Russia and Eurasia,Palgrave Macmillan, Basingstoke.Heng, C. K., Badner, V. M. and Schiop, L. A. (2008), ‘Meth mouth’,New York State Dental Journal74 (5), pp.50–1.Henskens, R. (2004), ‘Grab and hold: randomized controlled trial of the effectiveness of an outreach treatmentprogram for chronic high-risk crack abusers’ (dissertatie), GGD Rotterdam, Universiteit van Tilburg.Hermida, M., Ferreiro, M. C., Barral, S., Laredo, R., Castro, A. and Diz, D. P. (2002), ‘Detection of HCV RNA insaliva of patients with hepatitis C virus infection by using a highly sensitive test’,Journal of Virological Methods101, pp. 29–35.Hildrey, Z., Thomas, S. E. and Smith A. (2009), ‘The physical effects of amphetamine use’, in Pates, R. and Riley,D. (eds),Interventions for amphetamine misuse,Wiley-Blackwell, Oxford, pp. 173–204.Hinkle, Nancy C. (2000), ‘Delusory parasitosis’,American Entomologist46 (1), pp. 17–25.Holman, R. B. (1994), ‘Biological effects of central nervous system stimulants’,Addiction89 (11), pp. 1435–41.
221
Harm reduction: evidence, impacts and challenges
Horwitz, R. I., Hines, H. H., Brass, L. M., Kernan, W. N. and Viscoli, C. M. (2000),Phenylpropanolamine and riskof hemorrhagic stroke: final report of the hemorrhagic stroke project,Yale University School of Medicine. Availableat http://www.fda.gov/ohrms/dockets/ac/00/backgrd/3647b1_tab19.doc.Hunt, N. (2006),Paper C. An overview of models of delivery of drug consumption rooms, supporting evidence to TheReport of the Independent Working Group on Drug Consumption Rooms,Joseph Rowntree Foundation, York.Hunt, N., Ashton, M., Lenton, S., et al. (2003),A review of the evidence-base for harm reduction approaches todrug use,Forward Thinking on Drugs, London.Hunt, N., Trace, M. and Bewley-Taylor, D. (2005),Reducing drug-related harms to health: a global overview of theevidence,Beckley Foundation, London.Hurtado-Gumucio, J. (2000), ‘Coca leaf chewing as therapy for cocaine maintenance’,Annales de MédicineInterne151 (Supplement B), pp. 44–8.Islam, M. M. and Conigrave, K. M. (2007), ‘Assessing the role of syringe dispensing machines and mobile vanoutlets in reaching hard-to-reach and high-risk groups of injecting drug users (IDUs): a review’,Harm ReductionJournal,4: 14 (DOI: 10.1186/1477-7517-4-14).IWGDCR (Independent Working Group on Drug Consumption Room) (2006),The report of the IndependentWorking Group on Drug Consumption Rooms,Joseph Rowntree Foundation, York.Jaffe, C., Bush, K. R., Straits-Troster, K., et al. (2005), ‘A comparison of methamphetamine-dependent inpatientschildhood attention deficit hyperactivity disorder symptomatology’,Journal of Addictive Diseases24 (3), pp. 133–52.Jaffe, J. A. and Kimmel, P. L. (2006), ‘Chronic nephropathies of cocaine and heroin abuse: a critical review’,Clinical Journal of the American Society of Nephrology1 (4), pp. 655–67.Jauffret-Roustide, M. (2004),Les drogues: approche sociologique, économique et politique,La DocumentationFran§aise ed., Paris.Jauffret-Roustide, M., Couturier, E., Le Strat, Y., et al. (2006), ‘Estimation de la séroprévalence du VIH et du VHCet profils des usagers de drogues en France, étude InVS-ANRS Coquelicot, 2004’,Bull Epidemiol Hebd33, pp.244–7.Jauffret-Roustide, M., Rondy, M., Oudaya, L., Pequart, C., Semaille, C. and Desenclos, J. C. (2008a), ‘Evaluationd’un outil de réduction des risques visant à limiter la transmission du VIH et des hépatites chez les consommateursde crack’,Rev Epidemiol Sante Publique,56, p. 376.Jauffret-Roustide, M., Oudaya, L., Rondy, M., et al. (2008b), ‘Life trajectory and risk-taking among women drugusers’,Med Sci (Paris)24 (Spec No. 2), pp. 111–21.Jauffret-Roustide, M., Le Strat, Y. , Couturier, E., et al. (2009), ‘A national cross-sectional study among drug-users:estimates of HCV prevalence and highlight on practical and statistical aspects in the design’,BMC InfectiousDiseases9, pp. 113–25.Johnston, L. D., O’Malley, P. M., Bachman, J. G. and Schulenberg, J. E. (2004),Monitoring the future nationalresults on adolescent drug use: overview of key findings, 2003,National Institute on Drug Abuse, Bethesda, MD.Kampman, K. M., Leiderman, D., Holmes, T., et al. (2005), ‘Cocaine Rapid Efficacy Screening Trials (CREST):lessons learned’,Addiction100 (S1), pp. 102–10.Karch, S. B. (2005), ‘Cocaine cardiovascular toxicity’,Southern Medical Journal98 (8), pp. 794–9.
222
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
Kaye, S. and Darke, S. (2004), ‘Non-fatal cocaine overdose among injecting and non-injecting cocaine users inSydney, Australia’,Addiction99 (10), pp. 1315–22.Kearney, M. H., Murphy, S. and Rosenbaum, M. (1994), ‘Mothering on crack cocaine: a grounded theoryanalysis’,Social Science & Medicine38 (2), pp. 351–61.Kearney, M. H., Murphy, S., Irwin, K. and Rosenbaum, M. (1995), ‘Salvaging self: a grounded theory ofpregnancy on crack cocaine’,Nursing Research44 (4), pp. 208–13.Kelly, B. C. (2009), ‘Mediating MDMA-related harm: preloading and post-loading among ecstasy-using youth’,Journal of Psychoactive Drugs41 (1), pp. 19–26.Kerr, T., Wood, E. Grafstein, E., et al. (2005), ‘High rates of primary care and emergency department use amonginjection drug users’,Vancouver Journal of Public Health27 (1), pp. 62–66 (Doi:10.1093/Pubmed/Fdh189).Kertesz, S. G., Madan, A., Wallace, D., Schumacher, J. E. and Milby, J. B. (2006), ‘Substance abuse treatmentand psychiatric comorbidity: do benefits spill over? Analysis of data from a prospective trial among cocaine-dependent homeless persons’,Substance Abuse Treatment, Prevention, and Policy1, p. 27.Kertesz, S. G., Pletcher, M. J., Safford, M., et al. (2007), ‘Illicit drug use in young adults and subsequent declinein general health: the coronary artery risk development in young adults (cardia) study’,Drug and AlcoholDependence88 (2–3), pp. 224–33.Kilbride, H., Castor, C., Hoffman, E. and Fuger, K. L. (2000), ‘Thirty-six-month outcome of prenatal cocaineexposure for term or near-term infants: impact of early case management’,Journal of Developmental & BehavioralPediatrics21 (1), pp. 19–26.Kilbride, H. W., Castor, C. A. and Fuger, K. L. (2006), ‘School-age outcome of children with prenatal cocaineexposure following early case management’,Journal of Developmental & Behavioral Pediatrics27 (3), pp. 181–7.Kim, Y. H., Schiff, E., Waalen, J. and Hovell, M. (2005), ‘Efficacy of acupuncture for treating cocaine addiction:a review paper,’Journal of Addictive Diseases24, pp. 115–32.Kimber, J., Palmateer, N., Hutchinson, S., et al. (2010), ‘Harm reduction among injecting drug users: evidence ofeffectiveness’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction:evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10,Publications Office of the European Union, Luxembourg.Klemmt, L. and Scialli, A. R. (2005), ‘The transport of chemicals in semen’,Birth Defects Research Part B:Developmental and Reproductive Toxicology74 (2), pp. 119–31.Kloner, R. A., Hale, S., Alker, K. and Rezkalla, S. (1992), ‘The effects of acute and chronic cocaine use on theheart’,Circulation85 (2), pp. 407–19.Knox, E. G. (1989), ‘Detection of clusters’, in Elliott, P. (ed.),Methodology of enquiries into disease clustering,SmallArea Health Statistics Unit, London, pp. 17–20.Knuepfer, M. M. (2003), ‘Cardiovascular disorders associated with cocaine use: myths and truths’,Pharmacologyand Therapeutics97 (3), pp. 181–222.Koblin, B. A., Husnik, M. J., Colfax, G., et al. (2006), ‘Risk factors for HIV infection among men who have sexwith men’,Aids20 (5), pp. 731–9.Kottiri, B. J., Friedman, S. R., Euler, G. L., et al. (2005), ‘A community-based study of hepatitis B infection andimmunization among young adults in a high-drug-use neighborhood in New York City’,Journal of Urban Health82, pp. 479–87.
223
Harm reduction: evidence, impacts and challenges
Kozlov, A. P., Shaboltas, A. V., Toussova, O. V., et al. (2006), ‘HIV incidence and factors associated with HIVacquisition among injection drug users in St Petersburg, Russia’,AIDS20 (6), pp. 901–06.Kral, A. H., Bluthenthal, R. N., Booth, R. E. and Watters, J. K. (1998), ‘HIV seroprevalence among street-recruitedinjection drug and crack cocaine users in 16 US municipalities’,American Journal of Public Health88, pp. 108–13.Kral, A. H., Bluthenthal, R. N., Lorvick, J., et al. (2001), ‘Sexual transmission of HIV-1 among injection drug usersin San Francisco, USA: risk factor analysis’,Lancet357, pp. 1397–401.Kuczkowski, K. M. (2007), ‘The effects of drug abuse on pregnancy’,Current Opinion in Obstetrics andGynecology19 (6), pp. 578–85.Kwiatkowski, C. F., Fortuin, C. K. and Booth, R. E. (2002), ‘The association between knowledge of hepatitis Cvirus status and risk behaviours in injection drug users’,Addiction97, pp. 1289–94.Latka, M. (2003), ‘Drug-using women need comprehensive sexual risk reduction interventions’,Clinical InfectiousDiseases37 (Supplement 5), pp. S445–S450.Lee, C. S. (2008), ‘Delusions of parasitosis’,Dermatologic Therapy21 (1), pp. 2–7 (US: http://dx.doi.org/10.1111/j.1529-8019.2008.00163.x).Leicht, A., (1993),Characteristics and HIV-infection of users of syringe vending-machines and exchanging programsin Berlin/Germany,Berlin.Leiderman, D. B. (2005), ‘Cocaine Rapid Efficacy Screening Trial (CREST): a paradigm for the controlledevaluation of candidate medications for cocaine dependence’,Addiction100 (Supplement 1), pp. 1–11.Lejuez, C. W., Bornovalova, M. A., Daughters, S. B. and Curtin, J. J. (2005), ‘Differences in impulsivity andsexual risk behaviour among inner-city crack/cocaine users and heroin users’,Drug and Alcohol Dependence77,pp. 169–75.Leonard, L., Meadows, E., Pelude, L., et al. (2006),Results of the evaluation of the City of Ottawa’s Public HealthDepartment’s Safer Crack Use initiative: a harm reduction success,Ontario HIV Treatment Network ResearchConference, Toronto, 27–28 November.Leonard, L., De Rubeis, E., Pelude, L., et al. (2007), ‘I inject less as I have easier access to pipes: injecting, andsharing of crack-smoking materials, decline as safer crack-smocking resources are distributed’,InternationalJournal of Drug Policy,pp. 1–10.Lester, B. M., Lagasse, L., Seifer, R., et al. (2003), ‘The Maternal Lifestyle Study (MLS): effects of prenatal cocaineand/or opiate exposure on auditory brain response at one month’,Journal of Pediatrics142 (3), pp. 279–85.Lester, B. M., Andreozzi, L. and Appiah, L. (2004), ‘Substance use during pregnancy: time for policy to catch upwith research’,Harm Reduction Journal1 (1), p. 5.Llosa, T. (1994), ‘The standard low dose of oral cocaine: used for treatment of cocaine dependence’,SubstanceAbuse15 (4), pp. 215–20.Lloyd-Smith, E., Wood, E., Zhang, R., et al. (2008), ‘Risk factors for developing a cutaneous injection-relatedinfection among injection drug users: a cohort study’,BMC Public Health8, p. 405.Lussier, J. P., Heil, S. H., Mongeon, J. A. et al. (2006), ‘A meta-analysis of voucher-based reinforcement therapyfor substance use disorders’,Addiction101 (2), pp. 192–203.Maher, L., Li, J., Jalaludin, B., Chant, K. G. and Kaldor, J. M. (2007), ‘High hepatitis C incidence in new injectingdrug users: a policy failure?’Australian and New Zealand Journal of Public Health31 (1), pp. 30–5.
224
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
Malakmadze, N., Gonzalez, I. M., Oemig, T., et al. (2005), ‘Unsuspected recent transmission of tuberculosisamong high-risk groups: implications of universal tuberculosis genotyping in its detection’,Clinical InfectiousDiseases40, pp. 366–73.Malchy, L., Bungay, V. and Johnson, J. (2008), ‘Documenting practices and perceptions of “safer” crack use: aCanadian pilot study’,International Journal of Drug Policy19, pp. 339–41.Maliphant, J. and Scott, J. (2005), ‘Use of the femoral vein (“groin injecting”) by a sample of needle exchangeclients in Bristol, UK’,Harm Reduction Journal,2, p. 6 (DOI:10.1186/1477-7517-2-6).Maranda, M. J., Han, C. and Rainone, G. A. (2004), ‘Crack cocaine and sex’,Journal of Psychoactive Drugs36,pp. 315–22.Martell, B. A., Orson, F. M., Poling, J., et al. (2009), ‘Cocaine vaccine for the treatment of cocaine dependencein methadone-maintained patients’,Archives of General Psychiatry66 (10), pp. 1116–23.Martin, D. H. and DiCarlo, R. P. (1994), ‘Recent changes in the epidemiology of genital ulcer disease in theUnited States: the crack cocaine connection’,Sexually Transmitted Diseases21, pp. S76–S80.Mas, M., Farre, M., De La Torre, R., et al. (1999), ‘Cardiovascular and neuroendocrine effects andpharmacokinetics of 3, 4-Methylenedioxymethamphetamine in humans’,Journal of Pharmacology andExperimental Therapeutics290 (1), pp. 136–45.Maxwell, S., Bigg, D., Stanczykiewicz, K. and Carlberg-Racich, S. (2006), ‘Prescribing naloxone to activelyinjecting heroin users: a program to reduce heroin overdose deaths’,Journal of Addictive Diseases25 (3), pp.89–96.Mayaud, C., Boussaud, V., Saidi, F. and Parrot, A. (2001), ‘Bronchopulmonary disease in drug abusers’,Revue depneumologie Clinique57 (4), pp. 259–69.McCord, J., Jneid, H., Hollander, J. E., et al. (2008), ‘Management of cocaine-associated chest pain andmyocardial infarction: a scientific statement from the American Heart Association Acute Cardiac Care Committeeof the Council on Clinical Cardiology’,Circulation117 (14), pp. 1897–907.McCoy, C. B., Lai, S., Metsch, L. R., Messiah, S. E. and Zhao, W. (2004), ‘Injection drug use and crack cocainesmoking: independent and dual risk behaviours for HIV infection’,Annals of Epidemiology14, pp. 535–42.McCoy, H. V. and Miles C. A. (1992), ‘Gender comparison of health status among users of crack cocaine’,Journal of Psychoactive Drugs24, pp. 389–97.McElroy, P. D., Rothenberg, R. B., Varghese, R. et al. (2003), ‘A network-informed approach to investigating atuberculosis outbreak: implications for enhancing contact investigations’,International Journal of Tuberculosis andLung Disease7, pp. S486–S493.McMahon, J. M., Simm, M., Milano, D. and Clatts, M. (2004), ‘Detection of hepatitis C virus in the nasalsecretions of an intranasal drug-user’,Annals of Clinical Microbiology and Antimicrobials,3 (6). Available athttp://www.ann-clinmicrob.com/content/pdf/1476-0711-3-6.pdf (accessed on 23 January 2010).McPartland, J. M. and Pruitt, P. L. (1997), ‘Medical marijuana and its use by the immunocompromised’,AlternativeTherapies in Health and Medicine3 (3), pp. 39–45.Mehrabadi, A., Craib, K. J., Patterson, K., et al. (2008), ‘The Cedar Project: a comparison of HIV-relatedvulnerabilities amongst young Aboriginal women surviving drug use and sex work in two Canadian cities’,International Journal of Drug Policy19, pp. 159–68.Mesquita, F., Kral, A., Reingold, A., et al. (2001), ‘Overdoses among cocaine users in Brazil’,Addiction96 (12),pp. 1809–13.
225
Harm reduction: evidence, impacts and challenges
Miller, C. L., Tyndall, M., Spittal, P., et al. (2002), ‘Risk-taking behaviors among injecting drug users who obtainsyringes from pharmacies, fixed sites and mobile van needle exchanges’,Journal of Urban Health79 (2), pp.257–65.Milloy, M. J., Kerr, T., Tyndall, M., Montaner, J. and Wood, E. (2008), ‘Estimated drug overdose deaths avertedby North America’s first medically-supervised safer injection facility’,PloS ONE3 (10), p. E3351.Minkoff, H., Zhong, Y., Strickler, H. D., et al. (2008), ‘The relationship between cocaine use and humanpapillomavirus infections in HIV-seropositive and HIV-seronegative women’,Infectious Diseases in Obstetrics andGynecology,Article ID 587082, 7 pages (DOI: 10.1155/2008/587082).Mitchell, S. J., Morris, S. R., Kent, C. K., Stansell, J. and Klausner, J. D. (2006), ‘Methamphetamine use andsexual activity among HIV-infected patients in care — San Francisco’,AIDS Patient Care and STDs20 (7), pp.502–10.Moatti, J. P., Vlahov, D., Feroni, I., Perrin, V. and Obadia, Y. (2001), ‘Multiple access to sterile syringes forinjection drug users: vending machines, needle exchange programs and legal pharmacy sales in Marseille,France’,European Addiction Research7, pp. 40–5.Moeller, F. G., Barrat, E. S., Dougherty, D. M., et al. (2008), ‘Use of stimulants to treat cocaine andmethamphetamine abuse’,Current Psychiatry Reports10 (5), pp. 385–91.Morgan, M. J. (2000), ‘Ecstasy (MDMA): a review of its possible persistent psychological effects’,Psychopharmacology152, pp. 230–48.Murphy, E. L., DeVita, D., Liu, H., et al. (2001), ‘Risk factors for skin and soft-tissue abscesses among injectiondrug users: a case-control study’,Clinical Infectious Diseases33, pp. 35–40.Murphy, S. and Rosenbaum, M. (1999),Pregnant women on drugs: combating stereotypes and stigma,RutgersUniversity Press, New Jersey.Nabben, T., Benschop, A. and Korf, D. J. (2007),Antenna 2006. Trends in alcohol, tabak en drugs bij jongeAmsterdammers,Rozenberg Publishers, Amsterdam.Nath, A., Hauser, K. F., Wojna, V., et al. (2002), ‘Molecular basis for interactions of HIV and drugs of abuse’,Journal of Acquired Immune Deficiency Syndromes31 (Supplement 2), pp. S62–S69.Neaigus, A., Gyarmathy, V. A., Zhao, M., et al. (2007), ‘Sexual and other noninjection risks for HBV and HCVseroconversions among noninjecting heroin users’,Journal of Infectious Diseases195, pp. 1052–61.Needle, R. H., Burrows, D., Friedman, S. R., et al. (2005), ‘Effectiveness of community-based outreach inpreventing HIV/AIDS among injecting drug users’,International Journal of Drug Policy16 (Supplement 1), pp. 45–57. (Also at:Evidence for Action on HIV prevention among Injecting Drug Users,World Health Organization,Department of HIV/AIDS, Geneva, 2004.) Available at http://www.who.int/hiv/pub/prev_care/en/evidenceforactionalcommunityfinal.pdf (accessed on 23 January 2010).Ness, R. B., Grisso, J. A., Hirschinger, N., et al. (1999), ‘Cocaine and tobacco use and the risk of spontaneousabortion’,New England Journal of Medicine340 (5), pp. 333–9.Newlin, D. B., Wong, C. J., Stapleton, J. M. and London, E. D. (2000), ‘Intravenous cocaine decreases cardiacvagal tone, vagal index (derived in lorenz space), and heart period complexity (approximate entropy) in cocaineabusers’,Neuropsychopharmacology23 (5), pp. 560–8.Nnadi, C. U., Mimiko, O. A., Mccurtis, H. L. and Cadet, J. L. (2005), ‘Neuropsychiatric effects of cocaine usedisorders’,Journal of the National Medical Association97 (11),pp. 1504–15.
226
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
NTA (2002), ‘Treating cocaine/crack dependence’,Research Into Practice: 1a Drug Services Briefing, Drug andAlcohol Findings,National Treatment Agency for Substance Misuse, London.Nyamathi, A. M., Dixon, E. L., Robbins, W., et al. (2002), ‘Risk factors for hepatitis C virus infection amonghomeless adults’,The Journal of General Internal Medicine17, pp. 134–43.Obadia, Y., Feroni, I., Perrin, V., Vlahov, D. and Moatti, J. P. (1999), ‘Syringe vending machines for injecting drugusers: an experiment in Marseille, France’,American Journal of Public Health89 (12), pp. 1582–84.Ochoa, K. C., Davidson, P. J., Evans, J. L., et al. (2005), ‘Heroin overdose among young injection drug users inSan Francisco’,Drug and Alcohol Dependence80 (3), pp. 297–302.Osher, F. C., Goldberg, R. W., McNary, S. W., et al. (2003), ‘Substance abuse and the transmission of hepatitisC among persons with severe mental illness’,Psychiatric Services54, pp. 842–7.Oxman, G. L., Smolkowski, K. and Noell, J. (1996), ‘Mathematical modeling of epidemic syphilis transmission:implications for syphilis control programs’,Sexually Transmitted Diseases23, pp. 30–9.Pal, D., Mitra, A. K. (2006), ‘MDR- and CYP3A4-mediated drug-drug interactions’,Journal of NeuroimmunePharmacology1 (3), pp. 323–39.Pates, R. and Riley, D. (2009), ‘The psychological and psychiatric effects of amphetamine use’, in Pates, R. andRiley, D. (eds),Interventions for amphetamine misuse,Wiley-Blackwell, Oxford, pp. 173–204.Pechansky, F., Woody, G., Inciardi, J., et al. (2006), ‘HIV seroprevalence among drug users: an analysis ofselected variables based on 10 years of data collection in Porto Alegre, Brazil’,Drug and Alcohol Dependence82(Supplement 1), pp. S109–S113.Pennings, E. J., Leccese, A. P. and Wolff, F. A. (2002), ‘Effects of concurrent use of alcohol and cocaine’,Addiction97 (7), pp. 773–83.Perlman, D. C., Henman, A. R., Kochems, L., et al. (1999), ‘Doing a shotgun: a drug use practice and itsrelationship to sexual behaviours and infection risk’,Social Science & Medicine48, pp. 1441–8.Pirona, A. and Hedrich, D. (2009),Treatment of problem cocaine use: a short update(Version 1), EMCDDA,Lisbon. Available at http://www.emcdda.europa.eu/attachements.cfm/att_76877_EN_EMCDDA-cocaine%20treatment-update.pdf (accessed on 29 November 2009).Pizzey, R. and Hunt, N. (2008), ‘Distributing foil from needle and syringe programmes (NSPs) to promotetransitions from heroin injecting to chasing: an evaluation’,Harm Reduction Journal5, p. 24.Pleuvry, N. J. (2009), ‘Central nervous system stimulants: basic pharmacology and relevance to anaesthesia’,Anaesthesia and Intensive Care Medicine10 (7), pp. 344–7.Poel, A. van der, Barendregt, C. and Mheen, D. van de (2003), ‘Drug consumption rooms in Rotterdam: anexplorative description’,European Addiction Research9 (2), pp. 94–100.Popper, K. (1945),The open society and its enemies(Vols 1 and 2), George Routledge and Sons, London.Porter, J. and Bonilla, L. (1993), ‘Crack users’ cracked lips: an additional HIV risk factor’,American Journal ofPublic Health83, pp. 1490–1.Poschadel, S., Höger, R., Schnitzler, J. and Schreckenberg, D. (2002), ‘Evaluation der Arbeit derDrogenkonsumräume in der Bundesrepublik Deutschland. Endbericht im Auftrag des Bundesministeriums fürGesundheit’, ZEUS, Bochum.Prendergast, M., Podus, D., Finney, J., et al. (2006), ‘Contingency management for treatment of substance usedisorders: a meta-analysis’,Addiction101 (11), pp. 1546–60.
227
Harm reduction: evidence, impacts and challenges
Prinzleve, M., Verthein, U. and Degkwitz, P. (2002), ‘Ambulante Suchtakupunktur als Begleittherapie in derSubstitutionsbehandlung’,Suchttherapie3, pp. 197–204.Prinzleve, M., Haasen, C., Zurhold, H., et al. (2004), ‘Cocaine use in Europe — a multi-centre study: patterns ofuse in different groups’,European Addiction Research10 (4), pp. 147–55.Rhodes, T. (2002), ‘The “risk environment”: a framework for understanding and reducing drug-related harm’,International Journal of Drug Policy13 (2), pp. 85–94.Rhodes, T. (2009), ‘Risk environments and drug harms: a social science for harm reduction approach’,International Journal of Drug Policy20 (3), pp. 193–201.Rhodes, T., Stoneman, A., Hope, V., Hunt, N. and Judd, A. (2006), ‘Groin injecting in the context of crackcocaine and homelessness: from “risk boundary” to “acceptable risk”?’,International Journal of Drug Policy17, pp.164–70.Rhodes, T., Briggs, D., Kimber, J., Jones, S. and Holloway, G. (2007), ‘Crack-heroin speedball injection and itsimplications for vein care: qualitative study’,Addiction102, pp. 1782–90.Riley, E. D., Safaeian, M., Strathdee, S. et al. (2000), ‘Comparing new participants of a mobile versus apharmacy-based needle exchange program’,Journal of Acquired Immune Deficiency Syndromes24 (1), pp. 57–61.Rosenblum, A., Nuttbrock, L., McQuistion, H. L., Magura, S. and Joseph, H. (2001), ‘Hepatitis C and substanceuse in a sample of homeless people in New York City’,Journal of Addictive Diseases20, pp. 15–25.Ross, M. W., Hwang, L. Y., Leonard, L., Teng, M. and Duncan, L. (1999), ‘Sexual behaviour, STDs and drug usein a crack house population’,International Journal of STD & AIDS10, pp. 224–30.Ross, M. W., Hwang, L. Y., Zack, C., Bull, L. and Williams, M. L. (2002), ‘Sexual risk behaviours and STIs in drugabuse treatment populations whose drug of choice is crack cocaine’,International Journal of STD & AIDS13, pp.769–74.Rothenberg, R. (2007), ‘Maintenance of endemicity in urban environments: a hypothesis linking risk, networkstructure and geography’,Sexually Transmitted Infections83, pp. 10–15 (DOI:10.1136/sti. 2006.017269).Rotheram-Borus, M. J., Mann, T. and Chabon, B. (1999), ‘Amphetamine use and its correlates among youthsliving with HIV’,AIDS Education and Prevention11 (3), pp. 232–42.Roy, E., Haley, N., Leclerc, P., Boivin, J. F., Cedras, L. and Vincelette, J. (2001), ‘Risk factors for hepatitis C virusinfection among street youths’,Canadian Medical Association Journal165, pp. 557–60.Santibanez, S., Garfein, R., Swartzendruber, A., et al. (2006), ‘Update and overview of practical epidemiologicaspects of HIV/AIDS among injection drug users in the United States’,Journal of Urban Health83, pp. 86–100.Schaper, A., Hofmann, R., Bargain, P., Desel, H., Ebbecke, M. and Langer, C. (2007), ‘Surgical treatment incocaine body packers and body pushers’,International Journal of Colorectal Disease22 (12), pp. 1531–5.Scheinmann, R., Hagan, H., Lelutiu-Weinberger, C., et al. (2007), ‘Non-injection drug use and hepatitis C virus: asystematic review’,Drug and Alcohol Dependence89, pp. 1–12.Schempf, A. H. (2007), ‘Illicit drug use and neonatal outcomes: a critical review’,Obstetrical & GynecologicalSurvey62 (11), pp. 749–57.Schifano, F. (2004), ‘A bitter pill: overview of ecstasy (MDMA, MDA) related fatalities’,Psychopharmacology(Berl) 173 (3–4), pp. 242–8.Schiller, C. and Allen, P. J. (2005), ‘Follow-up of infants prenatally exposed to cocaine’,Pediatric Nursing31 (5),pp. 427–36.
228
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
Schindler, C. W., Tella, S. R., Erzouki, H. K. and Goldberg, S. R. (1995), ‘Pharmacological mechanisms incocaine’s cardiovascular effects’,Drug and Alcohol Dependence37 (3), pp. 183–91.Scott, J. C., Woods, S. P. and Matt, G. E., et al. (2007), ‘Neurocognitive effects of methamphetamine: a criticalreview and meta-analysis’,Neuropsychology Review17 (3), pp. 275–97.Seidman, S. N., Sterk-Elifson, C. and Aral, S. O. (1994), ‘High-risk sexual behaviour among drug-using men’,Sexually Transmitted Diseases21, pp. 173–80.Serraino, D., Franceschi, S., Vaccher, E., et al. (1991), ‘Risk factors for human immunodeficiency virus infection in581 intravenous drug users, northeast Italy, 1984–1988’,International Journal of Epidemiology20 (1), pp. 264–70.Shannon, K., Ishida, T., Morgan, R., et al. (2006), ‘Potential community and public health impacts of medicallysupervised safer smoking facilities for crack cocaine users’,Harm Reduction Journal3 (1) (DOI: 10.1186/1477-7517-3-1).Shannon, K., Rusch, M., Morgan, R., et al. (2008), ‘HIV and HCV prevalence and gender-specific risk profiles ofcrack cocaine smokers and dual users of injection drugs’,Substance Use and Misuse43, pp. 521–34.Shearer, J. (2007), ‘Psychosocial approaches to psychostimulant dependence: a systematic review’,Journal ofSubstance Abuse Treatment32 (1), pp. 41–52.Shearer, J. (2008), ‘The principles of agonist pharmacotherapy for psychostimulant dependence’,Drug andAlcohol Review27 (3), pp. 301–08.Shuter, J., Bell, D., Graham, D., Holbrook, K. A. and Bellin, E. Y. (1998), ‘Rates of and risk factors fortrichomoniasis among pregnant inmates in New York City’,Sexually Transmitted Diseases25, pp. 303–07.Small, D. and Drucker, E. (2008), ‘Return to galileo? The inquisition of the international narcotic control board’,Harm Reduction Journal5 (16) (DOI: 10.1186/1477-7517-5-16).Smith, L. M., Lagasse, L. L., Derauf, C., et al. (2006), ‘The infant development, environment, and lifestyle study:effects of prenatal methamphetamine exposure, polydrug exposure, and poverty on intrauterine growth’,Pediatrics118 (3), pp. 1149–56.Sorvillo, F., Kovacs, A., Kerndt, P., et al. (1998), ‘Risk factors for trichomoniasis among women with humanimmunodeficiency virus (HIV) infection at a public clinic in Los Angeles County, California: implications for HIVprevention’,American Journal of Tropical Medicine and Hygiene58, pp. 495–500.Sporer, K. A. and Kral, A. H. (2007), ‘Prescription naloxone: a novel approach to heroin overdose prevention’,Annals of Emergency Medicine49 (2), pp. 172–7.Stark, K., Leicht, A. and Müller, R. (1994), ‘Characteristics of users of syringe vending machines in Berlin’,Sozialund Praventivmedizin39 (4), pp. 209–16.Steinhauer, J. R. And Caulfield, J. B. (2001), ‘Spontaneous coronary artery dissection associated with cocaineuse: a case report and brief review’,Cardiovascular Pathology10 (3), pp. 141–5.Stern, L. S. (1992), ‘Self-injection education for street level sex workers’, in O’Hare, P., Newcombe, R., Matthews,A., Buning, E. and Drucker, E. (eds),The reduction of drug related harm,Routledge, London.Stevens, S. J., Estrada, A. L. and Estrada, B. D. (1998), ‘HIV sex and drug risk behavior and behavior change ina national sample of injection drug and crack cocaine using women’,Women Health27 (1–2), pp. 25–48.Stoner, B. P., Whittington, W. L., Hughes, J. P., Aral, S. O. and Holmes, K. K. (2000), ‘Comparative epidemiologyof heterosexual gonococcal and chlamydial networks: implications for transmission patterns’,Sexually TransmittedDiseases27, pp. 215–23.
229
Harm reduction: evidence, impacts and challenges
Stöver, H. (2001),Bestandsaufnahme „Crack-Konsum“ in Deutschland: Verbreitung, Konsummuster, Risiken undHilfeangebote,BISDRO, Bremen.Stöver, H. (2002), ‘Crack cocaine in Germany: current state of affairs’,Journal of Drug Issues32, pp. 413–22.Strang, J., Zador, D., Lintzeris, N., et al. (2008), ‘The fine line between harm reduction and harm production:development of a clinical policy on femoral (groin) injecting’,European Addiction Research14 (4), pp. 213–18.Sughondhabirom, A., Jain, D., Gueorguieva, R. et al. (2005), ‘A paradigm to investigate the self-regulation ofcocaine administration in humans’,Psychopharmacology180 (3), pp. 436–46.Sutcliffe, C. G., German, D., Sirirojn, B., et al. (2009), ‘Patterns of methamphetamine use and symptoms ofdepression among young adults in northern Thailand’,Drug and Alcohol Dependence101, pp. 146–51.Suzuki, T., Omata, K., Satoh, T., et al. (2005), ‘Quantitative detection of hepatitis C virus (HCV) RNA in salivaand gingival crevicular fluid of HCV-infected patients’,Journal of Clinical Microbiology43, pp. 4413–7.Symington, A. (2007), ‘Ottawa: crack pipe program cancelled by city council’,HIV/AIDS Policy & Law Review12,pp. 29–30.Templaski, B., Cooper, H., Friedman, S. R., et al. (2008), ‘Correlates of syringe coverage for heroin injection in35 large metropolitan areas in the US in which heroin is the dominant injected drug’,International Journal of DrugPolicy19, pp. S47–S58.Terra Filho, M., Yen, C. C., Santos Ude, P. and Munoz, D. R. (2004), ‘Pulmonary alterations in cocaine users’,Sao Paulo Medical Journal 122 (1), pp. 26–31.Theall, K. P., Sterk, C. E., Elifson, K. W. and Kidder, D. (2003), ‘Factors associated with positive HIV serostatusamong women who use drugs: continued evidence for expanding factors of influence’,Public Health Reports118,pp. 415–24.Thomas, J. C., Schoenbach, V. J., Weiner, D. H., Parker, E. A. and Earp, J. A. (1996), ‘Rural gonorrhea in thesoutheastern United States: a neglected epidemic?’,American Journal of Epidemiology143, pp. 269–77.Thorpe, L. E., Ouellet, L. J., Levy, J. R., Williams, I. T. and Monterroso, E. R. (2000), ‘Hepatitis C virus infection:prevalence, risk factors, and prevention opportunities among young injection drug users in Chicago, 1997–1999’,Journal of Infectious Diseases182, pp. 1588–94.Thorpe, L. E., Frederick, M., Pitt, J., et al. (2004), ‘Effect of hard-drug use on CD4 cell percentage, HIV RNA level,and progression to AIDS-defining class C events among HIV-infected women’,Journal of Acquired ImmuneDeficiency Syndromes37 (3), pp. 1423–30.Tortu, S., Beardsley, M., Deren, S., et al. (2000), ‘HIV infection and patterns of risk among women drug injectorsand crack users in low and high sero-prevalence sites’,AIDS Care12 (1), pp. 65–76.Tortu, S., Neaigus, A., McMahon, J. and Hagen, D. (2001), ‘Hepatitis C among noninjecting drug users: areport’,Substance Use and Misuse36, pp. 523–34.Tortu, S., Mcmahon, J. M., Hamid, R. and Neaigus, A. (2003), ‘Women’s drug injection practices in East Harlem:an event analysis in a high-risk community’,AIDS and Behavior7 (3), pp. 317–28.Tortu, S., McMahon, J. M., Pouget, E. R. and Hamid, R. (2004), ‘Sharing of noninjection drug-use implements asa risk factor for hepatitis C’,Substance Use and Misuse39, pp. 211–24.Tuncel, M., Wang, Z., Arbique, D., et al. (2002), ‘Mechanism of the blood pressure-raising effect of cocaine inhumans’,Circulation105 (9), pp. 1054–9.
230
Chapter 7: The fast and furious — cocaine, amphetamines and harm reduction
Vandhuick, O., Pistorius, M. A., Jousse, S., et al. (2004), ‘Drug addiction and cardiovascular pathologies’,J MalVasc29 (5), pp. 243–8.Venkatesan, A., Nath, A., Ming, G. L. and Song, H. (2007), ‘Adult hippocampal neurogenesis: regulation by HIVand drugs of abuse’,Cellular and Molecular Life Sciences64 (16), pp. 2120–32.Verthein, U., Haasen, C., Prinzleve, M. et al. (2001), ‘Cocaine use and the utilisation of drug help services byconsumers of the open drug scene in Hamburg,’European Addiction Research7, pp. 176–83.Vitiello, B. (2001), ‘Long-term effects of stimulant medications on the brain: possible relevance to the treatment ofattention deficit hyperactivity disorder’,Journal of Child and Adolescent Psychopharmacology11 (1), pp. 25–34.Vitiello, B. (2008), ‘Understanding the risk of using medications for attention deficit hyperactivity disorder withrespect to physical growth and cardiovascular function’,Child and Adolescent Psychiatric Clinics of North America17 (2), pp. 459–74.Vogt, I. and Zeissler, E. (2005),Abschlussbericht der Evaluation des Projektes Rauchraum im DrogennotdienstFrankfurt des Vereins Jugendberatung und Jugendhilfe e.V.,ISFF, Frankfurt.Vogt, I., Schmid, M. and Roth, M. (2000), ‘Crack-Konsum in der Drogenszene in Frankfurt am Main: Ergebnisseempirischer Studien,’Wiener Zeitschrift für Suchtforschung23, pp. 5–13.Volik, A. (2008), ‘Admixtures in home-made injecting drugs: components of harm and prevention of harmfulconsequences’,Public Health,Poltava, Ukraine. [Волик A., Примести в кустарных инъекционных наркотиках:
составляющие вреда и профилактика вредных последствий, БФ «Общественное здоровье», Полтава,Украина, 2008 г.].Ward, H., Pallecaros, A., Green, A. and Day, S. (2000), ‘Health issues associated with increasing use of “crack”cocaine among female sex workers in London’,Sexually Transmitted Infections76, pp. 292–3.Wechsberg, W. M., Lam, W. K., Zule, W. A. and Bobashev, G. (2004), ‘Efficacy of a woman-focusedintervention to reduce HIV risk and increase self-sufficiency among African American crack abusers’,AmericanJournal of Public Health94, pp. 1165–73.Williams, J. H. and Ross, L. (2007), ‘Consequences of prenatal toxin exposure for mental health in children andadolescents: a systematic review’,European Child & Adolescent Psychiatry16 (4), pp. 243–53.Williams, P. B. and Ekundayo, O. (2001), ’Study of distribution and factors affecting syphilis epidemic amonginner-city minorities of Baltimore’,Public Health115, pp. 387–93.Winhusen, T., Somoza, E. Ciraulo, D. A., et al. (2007a), ‘A double-blind, placebo-controlled trial of tiagabine forthe treatment of cocaine dependence’,Drug and Alcohol Dependence91 (2–3), pp. 141–8.Winhusen, T., Somoza, E. Ciraulo, D. A., et al. (2007b), ‘A double-blind, placebo-controlled trial of reserpine forthe treatment of cocaine dependence’,Drug and Alcohol Dependence91 (2–3), pp. 205–12.Wittenberg, S. (2005),Niet uit het veld te slaan - bereiken van basecokegebruikers op straat,Amsterdam, StichtingMainline.Wodak, A. and Cooney A. (2005), ‘Effectiveness of sterile needle and syringe programmes’,International Journalof Drug Policy,16S, pp. S31–S44.Wolff, A. J. and O’Donnell, A. E. (2004), ‘Pulmonary effects of illicit drug use’,Clinics in Chest Medicine25 (1),pp. 203–16.Wolff, F. H., Fuchs, S. C., Barcellos, N. T., et al. (2007), ‘Risk factors for hepatitis C virus infection in individualsinfected with the HIV’,Digestive and Liver Disease40 (6), pp. 460–7.
231
Harm reduction: evidence, impacts and challenges
Wood, E., Tyndall, M. W., Spittal, P. M., et al. (2002), ‘Factors associated with persistent high-risk syringesharing in the presence of an established needle exchange programme’,AIDS16 (6), pp. 941–3.Wood, E., Kerr, T., Spittal, P. M., et al. (2003), ‘An external evaluation of a peer-run “unsanctioned” syringeexchange program’,Journal of Urban Health,Bulletin of the New York Academy of Medicine, 80, pp. 455–64.Word, C. O. and Bowser, B. (1997), ‘Background to crack cocaine addiction and HIV high-risk behaviour: thenext epidemic’,American Journal of Drug and Alcohol Abuse23, pp. 67–77.WHO (World Health Organization) (2005),Policy and programming guide for HIV/AIDS prevention and careamong injecting drug users,Department of HIV/AIDS, Geneva.WHO, UNAIDS (Joint United Nations Programme on HIV/AIDS) and UNODC (United Nations Office on Drugsand Crime) (2004),Policy brief: provision of sterile injecting equipment to reduce HIV transmission,GeneralAssembly of the United Nations, Universal Declaration of Human Rights, New York, 10 December, 1948.WHO, UNODC and UNAIDS (2004),Substitution maintenance therapy in the management of opioid dependenceand HIV/AIDS prevention, Position paper,WHO, Geneva.Wynn, G. H., Cozza, K. L., Zapor, M. J., Wortmann, G. W. and Armstrong, S. C. (2005), ‘Med-psych drug-druginteractions update — antiretrovirals, part III: antiretrovirals and drugs of abuse’,Psychosomatics46 (1), pp. 79–87.Zador, D. A. (2007), ‘Facilitating groin injecting behaviour: harm reduction or harm production? (commentary)’,Addiction102, pp. 1791–2.Zhang, L., Xiao, Y. and He, J. (1999), ‘Cocaine and apoptosis in myocardial cells’,Anatomical Record,257 (6),pp. 208–16.Zinberg, N. E. (1984),Drug, set, and setting: the basis for controlled intoxicant use,Yale University Press, NewHaven.Zurhold, H., Kreutzfeld, N., Degkwitz, P. and Verthein, U. (2001),Drogenkonsumräume. Gesundheitsförderung undMinderung öffentlicher Belastungen in europäischen Großstädten,Lambertus, Freiburg i. Br.Zurhold, H., Degkwitz, P., Verthein, U. and Haasen, C. (2003), ‘Drug consumption rooms in Hamburg, Germany:evaluation of the effects on harm reduction and the reduction of public nuisance’,Journal of Drug Issues33 (3),pp. 663–88.
232
Chapter 8Harm reduction policies for cannabisWayne Hall and Benedikt Fischer
AbstractThis chapter reviews the limited evidence on strategies for reducing the harms arising fromcannabis use and from criminal penalties to control its use. It summarises evidence on theharms arising from cannabis use, namely, increased risks of: car crashes among users whodrive while intoxicated; the development of cannabis dependence among regular users;psychosis and poorer adolescent psychosocial outcomes; and increased risks of respiratorydisease from smoking. Strategies for reducing these risks to users are described, such as,roadside drug testing to deter cannabis-intoxicated driving, and education of users aboutpatterns of use that increase risks of dependence, poor mental health and respiratoryproblems. The chapter also briefly discusses depenalisation and decriminalisation ofcannabis use as strategies to reduce harms arising from cannabis prohibition. It concludeswith suggestions for research priorities in how to reduce harms arising from cannabis useand the policies adopted to reduce such use.Keywords:cannabis-impaired driving, cannabis dependence, respiratory risks, cannabisdecriminalisation.
IntroductionCannabis is the most widely used illicit drug globally, and its use has increased over the pastdecade. In 2005, around 160 million adults (4 % of the global adult population) were estimatedto have used cannabis in the previous year, 10 % more than in the mid 1990s (UNODC, 2007).In the recent World Mental Health Surveys, the lifetime use of cannabis was higher in theUnited States and New Zealand than in Europe, which, in turn, reported higher rates of usethan the Middle East and Africa or Asia (Degenhardt et al., 2008). Because of their largerpopulations, Asia, Africa and the Americas account for an estimated 31 %, 24 % and 24 % ofglobal cannabis use compared to 19 % in Europe and 2 % in Oceania (UNODC, 2007).In the United States in 2005, 40 % of the adult population reported using cannabis at sometime in their lives and 13 % of adolescents reported use in the past year (SAMHSA, 2006).Cannabis use in most countries begins in the mid to late teens and is most common amongpeople in their early 20s (Degenhardt et al., 2008). Most use is intermittent and time-limited(Bachman et al., 1997), with about 10 % of those who ever use cannabis becoming dailyusers, and another 20 % to 30 % using weekly (Hall and Pacula, 2003). Cannabis usedeclines from the early and mid 20s to the early 30s, reflecting major role transitions in earlyadulthood (e.g. entering tertiary education or full-time employment, marrying, and havingchildren) (Anthony, 2006; Bachman et al., 1997).235
Harm reduction: evidence, impacts and challenges
Cannabis use in EuropeCannabis is the most widely used illicit drug among European adolescents and its use is socommon that it has been described as an ‘illegal everyday drug’ (Essau, 2006). In the late1990s and early 2000s, the median rate of lifetime cannabis use among European adultsaged between 18 and 64 years was 15 %, with a range between 31 % in the Czech Republicand 2 % in Romania (EMCDDA, 2006). Rates of lifetime use were higher among youngeradults (aged between 15 and 34 years), with a median rate of 21 %, and a range between3 % in Romania and 45 % in Denmark (EMCDDA, 2006).Smart and Ogborne (2000) have summarised data on illicit drug use among high schoolstudents in 36 European countries during the mid-1990s (circa 1995). The highest prevalenceof lifetime cannabis use was found in Scotland (53 %), which was higher than the overallprevalence in the United Kingdom (41 %), followed by the Netherlands (22 %). These ratesincreased during the 1990s in those countries that have undertaken a series of surveys overthat time, namely, the Netherlands, Switzerland, and Norway (Harkin et al., 1997). Thesetrends mirror those in Australia, Canada and the United States (Room et al., 2008).More recent survey data collected by EMCDDA suggests that cannabis use rates haveincreased throughout Europe since then, and have recently begun to stabilise. Out of a totalpopulation of almost 500 million, 74 million Europeans aged 16 to 64 years have hadlifetime experience with cannabis, 23 million in the past year, and 12 million in the pastmonth (see the General Population Survey Tables in EMCDDA, 2009). Highest rates of usewere in young adults aged 15–34 years (31 % lifetime, 13 % past year). These rates varybetween countries (ranges 3 %–50 % and 1 %–21 % respectively). Average European rateswere lower than in the United States (49 % and 21 %), Canada (58 % and 28 %) andAustralia (48 % and 20 %) in the mid 2000s.
The probable harms of cannabis useAs argued in more detail elsewhere (Hall and Pacula, 2003; Room et al., 2008), there isreasonable evidence that cannabis use can harm some users. In this chapter we summarisethe evidence on those adverse effects most commonly attributed to cannabis use and bestsupported by epidemiological evidence. We then describe strategies that could be used toreduce these harms arising from cannabis use. We also briefly discuss alternative policyapproaches that aim to reduce harms arising from current criminal control policies towardscannabis use.Cannabis and motor vehicle crashesCannabis intoxication produces dose-related impairments in cognitive and behavioural skillsthat may affect driving (Mannet al., 2008; Ramaekers et al., 2004; Solowij, 1998). Olderstudies that measured inactive metabolites of tetrahydrocannabinol (THC) could not assesswhether drivers were impaired at the time of accidents (Ramaekers et al., 2004). Recent236
Chapter 8: Harm reduction policies for cannabis
studies measuring THC in blood suggest that cannabis-affected drivers are at a higher risk ofbeing involved in crashes (e.g. Drummer et al., 2004; Gerberich et al., 2003; Mura et al.,2003). Cannabis use appears to increase the risk of motor vehicle crashes by two to threetimes (Ramaekers et al., 2004) compared with 6 to 15 times for alcohol. It has beenestimated that cannabis-affected driving accounted for 2.5 % of fatal accidents in France,compared to 29 % for alcohol (Laumon et al., 2005).
Cannabis dependenceA cannabis dependence syndrome develops in some daily or near-daily users of cannabis(Budney, 2006; Roffman and Stephens, 2006). Cannabis dependence is characterised bymarked distress resulting from impaired control over cannabis use and difficulty in ceasinguse despite harms caused by it. After tobacco and alcohol, cannabis was the most commonform of drug dependence in the US in the 1990s and early 2000s (Anthony, 2006) and inAustralia in the late 1990s (Hall et al., 1999). The risk of developing cannabis dependence inthe United States is similar to that for alcohol but lower than that for nicotine and the opioids(Anthony et al., 1994). Around 10 % of those who ever use cannabis meet criteria fordependence (Anthony, 2006). This rises to 16 % in persons who initiate in early adolescence(Anthony, 2006).Over the past two decades, increasing numbers of people have sought professional help fortheir cannabis use in the United States, Europe and Australia (Hall and Pacula, 2003). InEurope in 2006 there were 390,000 requests for treatment for cannabis dependence(EMCDDA, 2008). This was 21 % of all cases requesting assistance for illicit drugs andsecond only to opioids (EMCDDA, 2008). Some of this increase may be explained byincreased diversion of cannabis users apprehended by the police into treatment programmes,but not all, because increases have also occurred in the Netherlands where cannabispossession has been decriminalised de facto (Dutch National Alcohol and Drug InformationSystem, 2004).
Cannabis and schizophreniaA 15-year prospective study of 50 465 Swedish conscripts (Andréasson et al., 1987) foundthat the risk of schizophrenia increased with the number of times cannabis had been used byage 18. A 27-year follow-up of the same cohort (Zammit et al., 2002) also found a dose-response relationship between frequency of cannabis use at baseline and risk ofschizophrenia during the follow-up. These relationships persisted after controlling for otherdrug use and other confounding factors. These findings have been supported by longitudinalstudies in the Netherlands (van Os et al., 2002) and Germany (Henquet et al., 2004) and bytwo small New Zealand cohort studies (Arseneault et al., 2002; Fergusson et al., 2003). Themost plausible explanation appears to be that regular cannabis use acts with a variety ofother unknown risk factors to precipitate psychoses in vulnerable individuals (Degenhardtand Hall, 2006; Moore et al., 2007).237
Harm reduction: evidence, impacts and challenges
The respiratory risks of cannabis smokingRegular smokers of cannabis who do not smoke tobacco have more symptoms of chronicbronchitis and poorer lung function than people who do not smoke either cannabis ortobacco (see Tashkin, 1999). People who smoke cannabis with or without tobacco also seemto be more susceptible to respiratory infections (Tashkin, 1999).Cannabis smoke is carcinogenic (Marselos and Karamanakos, 1999), making cannabissmoking a potential cause of cancers of the lung and mouth, tongue, and oesophagus (Halland MacPhee, 2002). Epidemiological studies of head and neck cancer have producedconflicting results: one case control study found an association (Zhang et al., 1999) but alongitudinal study (Sidney et al., 1997) and two other case control studies failed to do so(Llewellyn et al., 2004; Rosenblatt et al., 2004). Case control studies of cannabis smoking andlung cancer have found associations but they have not been able to separate the effects ofcannabis from tobacco smoking because most cannabis users in these studies were also dailycigarette smokers (Mehra et al., 2006).
Potential harm reduction strategies for cannabisThe following sections outline some potential harm reduction strategies for cannabis. Someare based on adaptations of similar policies that have been used to reduce harm from otherdrugs, such as alcohol. In other cases we outline the type of advice that could be given tousers to avoid patterns or practices of use that increase the risk of experiencing adversehealth outcomes (Swift et al., 2000). With few exceptions, there is little evidence on theireffectiveness. Research into the effectiveness of these proposals should be a priority for harmreduction policies for cannabis.Motor vehicle accidentsIt is obvious that cannabis users can avoid cannabis-related vehicle crashes by not drivingwhile intoxicated, but it is uncertain whether cannabis users have responded to educationcampaigns that urge them not to drive after using. Australia, Norway and Sweden haveadopted random roadside drug testing in an effort to discourage cannabis-impaired driving.In Australia, the Victorian state government introduced random roadside saliva testing forcannabis and other drugs in December 2004; other Australian states and territories havesince followed (Butler, 2007). Australian legislators have assumed that this policy willsubstantially reduce cannabis-related road crashes in the same way that random breathtesting reduced alcohol related crashes in Australia (Henstridge et al., 1997). Other Europeancountries have adopted the more focused policy of testing for cannabis in saliva or urine onsuspicion of use or evidence of impaired driving (Mann et al., 2008).The illegality of cannabis use has prompted the adoption of a ‘zero tolerance’ approach inAustralia, Norway and Sweden, with the presence of any detectable amount of THC definedas an offence (Butler, 2007). Any road safety benefits of this policy are a by-product of thedeterrent effect of enforcing prohibitive drug laws. Proponents of drug testing argue that it238
Chapter 8: Harm reduction policies for cannabis
will save lives (Jones et al., 2008) but so far there is no evidence that it has done so. Thispolicy needs to be properly evaluated to see if it reduces cannabis-impaired driving at anacceptable social and economic cost (Hall and Homel, 2007). Other approaches that focuson harm reduction would include: developing measures of cannabis-impaired driving, asadvocated by Grotenhermen et al. (2007), and encouraging cannabis users to adopt‘designated driver’ programmes like those advocated for alcohol users.Cannabis dependenceAn essential first step in reducing the risk of cannabis dependence is informing users of therisk. This can be done by explaining that the risk increases with regular use and is greatestwhen cannabis is used daily for weeks or months, as is true for alcohol and tobaccodependence. Priorities for research include assessing whether users will accept this advice orwhat the most persuasive way of delivering it would be.Screening and brief advice for excessive alcohol consumption in general practice, hospital oreven non-medical settings reduces consumption and the problems caused by alcohol (e.g.Shand et al., 2003). The same approach could be adopted for cannabis use disorders inprimary care settings, for example among young adults with respiratory problems orsymptoms of anxiety and depression, all of which are common among cannabis-dependentindividuals who seek help from family physicians (Degenhardt et al., 2001).Similarly, brief interventions for frequent cannabis users could be targeted at populations and/orsettings where cannabis use is known to be high, for example youth mental health services,juvenile justice centres, and among college students (Hall et al., 2008a). Such interventions couldadvise users to reduce the frequency of cannabis use and not to use it before driving. A ‘check-up’ approach modelled on the Brief Drinker Check-up (Miller and Sovereign, 1989) provides apromising model for raising the issue of health risks of cannabis use in a non-confrontationalway (see Berghuis et al., 2006). This approach has been trialled and evaluated with promisingresults in a number of studies (Martin and Copeland, 2008; Stephens et al., 2007).The question of how best to inform young people about the risks of cannabis dependencerequires research on young people’s views about the type of information that they find mostpersuasive. In the interim the following are suggestions about what advice could be given:• annabis users can become dependent on cannabis. The risk (around 10 %) is lower than that Cfor alcohol, nicotine and opiates, but the earlier that a young person begins the higher the risk.• sing cannabis more than weekly increases the risks of developing dependence and other Uhealth problems.• egular use probably also increases the risk of psychosis in young people who have a Rfamily member with a psychosis or other mental disorder, or who have unusualpsychological experiences after using cannabis.• riving within a few hours of cannabis use increases the risk of both fatal and non-fatal Dmotor vehicle accident involvement and should be avoided, especially after drinkingalcohol.239
Harm reduction: evidence, impacts and challenges
Cognitive behavioural therapy can be used to treat cannabis dependence on an outpatientbasis. Rates of abstinence have been modest — for example, around 15 % reported continuousabstinence at six-month follow-ups, according to Copeland et al. (2001) — but cannabis useand cannabis-related problems are substantially reduced (Denis et al., 2006; Roffman andStephens, 2006). A recent review by Nordstrom and Levin (2007) concluded that while anumber of psychotherapies have been found to be effective in treating this disorder, none hasbeen found to be more effective than any other, although offering vouchers as a reward toreinforce negative urine toxicology screens improved abstinence during treatment.Informing young people about the mental health risks of cannabis useA major public health challenge will be finding effective ways of explaining the mental healthrisks of cannabis use to young people. In addition to a possible increased risk of psychosis,young people also need to be informed about the risks of developing dependence, impairingtheir educational attainment, and possibly increasing their risk of depression (Hall, 2006;Patton et al., 2002). These risks add weight to the prudential argument for discouragingcannabis use by young people.Policymakers need to be realistic about the impacts of educational messages (Caulkins et al.,2004; White and Pitts, 1998). Small, statistically significant reductions in cannabis use maybe observed in well-conducted programmes (Caulkins et al., 2004; Gorman, 1995; Tobler,Lessard, Marshall et al., 1999; White and Pitts, 1998) but the primary impact is onknowledge rather than behaviour (White and Pitts, 1998). Any behaviour change is morelikely to occur among less frequent rather than heavier users (Gorman, 1995). Given this, thenature and delivery of the advice may need to differ for different groups facing differentlevels of risk (Toumbourou et al., 2004). The best way to deliver the advice will depend upongood social marketing research on the views of young people (Grier and Bryant, 2005).Education about the risks of cannabis use should explain the mental health risks of regularintoxication with alcohol and cannabis; and define the high-risk groups, namely those with afamily history of psychosis and those who have had bad experiences with cannabis. Sucheducation needs to be directed not only at cannabis users but also at their peers to increaserecognition of these problems among young people so that they can encourage affectedpeers to cease using or seek help earlier than might otherwise be the case.A major challenge is framing the magnitude of the risk of psychosis. The risk for anyindividual increases from around 7 in 1 000 (Saha et al., 2005) to 14 in 1 000, but theconsequences of psychosis for those individuals who are vulnerable are serious. Thetemptation for parents and health educators is to play up the risk, arguing that everyone is atrisk because it is difficult to predict which young people are most vulnerable. This strategy isof doubtful effectiveness and may undermine the credibility of the message by being seen toexaggerate the risk.It is prudent to encourage young people who use cannabis and experience psychoticsymptoms to stop, or at the very least to reduce the frequency of their cannabis use. The240
Chapter 8: Harm reduction policies for cannabis
challenge in implementing this goal is finding effective ways of persuading persons withschizophrenia to stop doing something that they enjoy and to help those who want to stopbut find it difficult to do so. Many persons with schizophrenia have characteristics that predicta poor outcome from psychological interventions for cannabis dependence, namely, theylack social support, may be cognitively impaired, are often unemployed, and do not complywith treatment (Kavanagh, 1995; Mueser et al., 1992). There are very few controlled outcomestudies of substance abuse treatment in schizophrenia (Lehman et al., 1993). A recentCochrane review identified only six relevant studies, four of which were small (Jeffery et al.,2004) and found no clear evidence that supported substance abuse treatment inschizophrenia over standard care.Reducing respiratory risksThe respiratory risks of cannabis smoking could be eliminated if cannabis users adoptedeating or ingesting rather than smoking cannabis. This is unlikely to happen, because mostlong-term users find smoking a more efficient and easier way to titrate their dose of THC thanthe oral route (Grotenhermen, 2004; Iversen, 2007).Putatively ‘safer’ forms of cannabis smoking, such as water pipes, are popular amongyounger cannabis users in Australia (Hall and Swift, 2000) but United States and Australian(Gowing et al., 2000) research suggests that water pipes deliver more tar per dose of THCthan do joints. It is also unclear how much the respiratory risks of cannabis smoking might bereduced if users were to smoke lesser amounts of the more potent cannabis products(Melamede, 2005). There has been too little research to determine whether users can reliablytitrate their dose and, if they can, whether in fact they do so (Hall and Pacula, 2003).It is reasonable to advise cannabis smokers to avoid breath-holding or ‘deep inhalation’techniques to maximise the absorption of THC in the lungs. This practice increases thequantities of tar and particulate matter that are retained in the lungs without necessarilyincreasing the THC delivered. It is also advisable for cannabis users to eliminate the use oftobacco in smoked cannabis preparations because of tobacco’s addictiveness andcarcinogenicity.Vaporisers appear to be a more promising way of reducing the carcinogens and toxicantsinhaled when cannabis is smoked (Gieringer et al., 2004; Grotenhermen, 2004; Melamede,2005). These devices are designed to deliver inhaled THC without carcinogens and toxicants.They do so by heating cannabis to a temperature (180oC), which releases THC without burningthe plant material. A study by Gieringer et al. (2004) found that vaporisers achieved a similarefficacy in delivery of THC to smoking a cannabis cigarette while very substantially reducinglevels of carcinogens. Hazekamp et al. (2006) evaluated the performance of the same device indelivering pure THC and found that it had acceptable safety properties. However, Bloor et al.(2008) found that while vaporisers reduced levels of released ammonia, compared to smokedcannabis these levels (170 ppm) were still well above recommended safe levels (35 ppm) forshort-term occupational exposures. These levels of ammonia increase respiratory irritation, butthe respiratory effects of long-term intermittent exposure in daily users are unknown.241
Harm reduction: evidence, impacts and challenges
Abrams et al. (2007) compared the effects of varying doses of cannabis vaporised andsmoked in a joint in 18 subjects under double blind conditions. They found that the vaporiserdelivered similar amounts of THC and produced similar psychological effects. Sixteen of the18 subjects preferred the vaporiser. They did not test for delivery of tars and carcinogens butdid find lower CO levels in blood when using a vaporiser. Earleywine and Barnwell (2007)found suggestive evidence that vaporisers had reduced respiratory symptoms in aconvenience sample of 6 883 cannabis users interviewed via the Internet. The rate ofrespiratory symptoms (bronchitis, wheeze, breathlessness) among the 150 who reported onlyusing vaporisers was 40 % of that reported by cannabis smokers (after controlling forcigarette smoking, duration of use and amount typically used). The reduction in symptomsamong vaporiser users appeared to be larger in heavier cannabis users. More work isneeded to evaluate the long-term safety and efficacy of vaporisers in reducing therespiratory risks of cannabis use.Reducing the harms arising from cannabis control policiesUnder current criminal cannabis control policies in many European and other developedcountries, cannabis users can nominally be sentenced to prison if caught in possession ofcannabis. Even if prison sentences are rarely imposed, the acquisition of a criminal convictionor record for the personal use of cannabis can adversely affect the lives of otherwise law-abiding users (Lenton, 2000) in ways that some have argued are more serious than anyharms that result from using cannabis (Wodak et al., 2002), for example, by impedingprofessional or travel opportunities and adversely affecting personal relationships (Room etal., 2008). The limited research (Erickson, 1980; Lenton et al., 1999a; Lenton et al., 1999b)suggests: that many persons convicted of cannabis offences have no other criminal records;that a criminal conviction adversely affects their employment prospects and their reputations;and that it has a negligible effect on their cannabis use.The enforcement of cannabis control laws is also often applied in a highly selective, if notdiscriminatory, way. In Australia in the early 1990s cannabis offenders appearing before thecriminal courts were more likely to be unemployed and socially disadvantaged males thanwere cannabis users in community surveys (Advisory Committee on Illicit Drugs, 1993). RecentUS studies show higher rates of arrests for cannabis offences among Hispanic and Blackminorities (Gettman, 2000; Human Rights Watch, 2000). It is uncertain to what extent the sameis true in European countries with substantial ethnic minorities or immigrant populations.The non-enforcement or removal of criminal penalties for personal use is one way ofreducing the adverse effects of the law on users. The Netherlands was one of the firstEuropean countries to do so in 1976 (see box ‘De facto cannabis decriminalisation in theNetherlands’, p. 243), and Portugal has more recently done so among other Europeancountries (see box ‘Cannabis decriminalisation in Portugal’, p. 243). In several Australianstates, personal cannabis use is subject to a non-criminal ‘infringement’ or ‘expiation’ notice,an offence similar to a speeding ticket and punished by a limited fine (Room et al. 2008).Studies of the impact of these changes have typically found that reductions in the severity ofpenalties for cannabis use have little, if any, impact on rates of population cannabis use in242
Chapter 8: Harm reduction policies for cannabis
Australia (e.g. Donnelly et al., 1999), the United States (Pacula et al., 2004) and Europe(Greenwald, 2009; Room et al., 2008). The lack of any evidence of a large impact on ratesof use also suggests that this policy may have little or no effect on cannabis-related harms,while at the same time reducing enforcement costs and effects on users (Room et al., 2008).
De facto cannabis decriminalisation in the NetherlandsThe Netherlands decriminalised cannabis possession for personal use on a ‘de facto’ basisfrom 1976. This means that while personal possession is still formally prohibited by criminallaw, the law is not enforced. The Dutch system tolerates cannabis users possessing andbuying small amounts of cannabis for personal use, most notably in several hundred ‘coffeeshops’ across the country. Also in the Netherlands, no major changes in cannabis use rateshave been observed that could be unambiguously attributed to this policy, and use rates arelower than the EU average. This approach aims to separate the cannabis market from that ofother illicit drugs. While this de facto decriminalisation has been well-supported politicallyand socially in the Netherlands, it has recently come under some pressure from neighbouringcountries concerned about ‘drug tourism’ (Chatwin, 2003; MacCoun and Reuter, 1997;Pakes, 2004; Room et al., 2008). The Dutch government has responded to these concerns byreducing the number of coffee shops and the amount of cannabis that can be sold.
Cannabis decriminalisation in PortugalPortugal formally decriminalised use of all illicit drugs by changing its drug control laws in2001. Cannabis use and possession remains illegal but it is treated as an ‘administrativeviolation’. Drug use offenders are brought to the attention of ‘Dissuasion Commissions’ whotypically suspend any punitive proceedings. In serious cases, such as those of repeat offenders,administrative penalties — like fines, suspension of driver’s licence or community serviceorders — can be imposed and problematic users can be referred to treatment. Since thesereforms, no significant changes have been observed in cannabis use, which remains lowcompared to other EU countries and North America. The number of drug use infractions hasbeen stable since the reforms, which have been well-accepted politically and by the generalpublic (Greenwald, 2009; Hughes and Stevens, 2007; Room et al., 2008).
An unintended consequence of depenalisation via civil penalties can be an increase innumbers of persons fined or diverted into non-criminal interventions (e.g., education ortreatment measures) by the police, an effect referred to as ‘net widening’. This occurs becausethe police find it easier and less time-consuming to enact non-criminal measures (e.g. imposea fine) than to formally arrest and process a criminal charge. If a substantial proportion ofoffenders do not pay their fines, more cannabis users may end up in prisons for fine-defaultthan would be the case if cannabis use remained as a criminal offence (Room et al., 2008).The removal or the non-enforcement of any penalties for personal use (as in the Netherlands)avoids this problem (Hall and Pacula, 2003; Room et al., 2008), as does allowing non-custodial ways to enforce the payment of fines (Room et al., 2008).243
Harm reduction: evidence, impacts and challenges
Research priorities for cannabis harm reductionResearch is needed on the effectiveness of these policies that aim to reduce the harms ofcannabis use. Among the priorities for future inquiry are the following questions:• hat do cannabis users believe are the harms of using cannabis?W• oes the type of evidence presented about these adverse effects persuade them?D• re they prepared to act on advice about how to reduce these harms?A• oes roadside drug testing deter cannabis users from driving while intoxicated? If so, does Dthis reduce motor vehicle accident fatalities? Does it do so at an acceptable social and economic cost? Are there better ways than deterrence policies to reduce risks related to cannabis and driving?• o adolescent users accept that cannabis use can be harmful? Are they prepared to act Don harm reduction advice? Are brief interventions in medical or non-medical settings effective in changing risk patterns of use or practices?• oes the use of vaporisers substantially reduce the respiratory risks of cannabis smoking?D• o cannabis users titrate their doses of cannabis products?DAmong priorities for research on the effects of harm reduction measures such asdepenalisation and decriminalisation are the following:• o depenalisation or decriminalisation policies result in changes in patterns or rates of Dcannabis use, or attitudes towards cannabis use, especially among vulnerable/high-riskpopulations (e.g., youth/students)?• ill more tolerant policies for cannabis use reduce access or exposure to other illicit drugs?W• o decriminalisation approaches result in tangible savings of public resources (e.g., Denforcement time) without increasing the prevalence of harmful cannabis use (e.g.,numbers seeking treatment for cannabis dependence)?
ConclusionsCannabis is the most widely used illicit drug in Europe, as it is globally. While cannabis useclearly does not result in harms that are comparable to those of alcohol or tobacco, its use isassociated with significant potential risks and harms. Based on existing evidence, a numberof these risks and harms are modifiable by harm reduction approaches directed at users. Thismore pragmatic, ‘public health’ approach that builds on experiences from the alcohol fieldrequires substantial additional research and policy engagement. Its utility is still hindered bythe century-old illegal status of cannabis in most European jurisdictions.Driving under the influence of cannabis has been given considerable attention in recent years.Governments in Australia, Norway and Sweden have implemented random roadside salivatesting to detect the presence of cannabis in drivers to reduce cannabis-impaired driving andprevent accidents as a primary harm. However, the scope of this policy might be overly punitivein penalising drivers who are not actually impaired by cannabis while driving. Thus, theeffectiveness, cost-effectiveness and social effects of this policy remains to be evaluated.244
Chapter 8: Harm reduction policies for cannabis
Given the existing knowledge around the acute and long-term harms associated withcannabis use, and key predictors of these effects, there appears to be considerable room forinterventions with or advice to cannabis users towards reducing the odds or severity ofproblems resulting from use. For example, harm reduction advice that could be given tocurrent cannabis users includes the following:• void more than weekly use to minimise the risks of developing mental health problems or Adependence.• void smoking as a route of administration or use a vaporiser instead, rather than smoke Aa bong or joint.• f you smoke cannabis, avoid deep inhalation or breath-holding practices in order to Ireduce the risks of respiratory problems.• o not drive or use machinery when intoxicated.DThere is a need for research on how to effectively convey such messages, and tomeasure their potential impacts on individual and/or population levels of harm fromcannabis use.There is reasonable evidence that removing criminal penalties for personal possessionand use of cannabis reduces some of the harms of current control policy incurred byusers who come to the attention of criminal control. This policy can reduce the extensivesocial and economic harms of use prohibition (rather than the effects of cannabis use)without producing large increases in the prevalence of cannabis use, as recent policyreform experiments in a number of countries have suggested. Such efforts would alsohelp to bring cannabis use more into a policy framework of public health rather thanrepressive control. They may facilitate steps towards a more integrated and rationalregulation of all commonly used psychoactive substances guided by their potential tocause harm and evidence on the benefits and costs of different interventions (Nutt et al.2007).
ReferencesAbrams, D., Vizoso, H., Shade, S., Jay, C., Kelly, M. and Benowitz, N. (2007), ‘Vaporization as a smokelesscannabis delivery system: a pilot study’,Clinical Psychopharmacology & Therapeutics82, pp. 572–8.Advisory Committee on Illicit Drugs (1993),Cannabis and the law in Queensland: a discussion paper,QueenslandCriminal Justice Commission, Brisbane.Andréasson, S., Engstrom, A., Allebeck, P. and Rydberg, U. (1987), ‘Cannabis and schizophrenia: a longitudinalstudy of Swedish conscripts’,Lancet2, pp. 1483–6.Anthony, J. C. (2006), ‘The epidemiology of cannabis dependence’, in Roffman, R. A. and Stephens, R. S. (eds),Cannabis dependence: its nature, consequences and treatment,Cambridge University Press, Cambridge, UK, pp.58–105.
245
Harm reduction: evidence, impacts and challenges
Anthony, J. C., Warner, L. and Kessler, R. (1994), ‘Comparative epidemiology of dependence on tobacco,alcohol, controlled substances and inhalants: basic findings from the National Comorbidity Survey’,Experimentaland Clinical Psychopharmacology2, pp. 244–68.Arseneault, L., Cannon, M., Poulton, R., et al. (2002), ‘Cannabis use in adolescence and risk for adult psychosis:longitudinal prospective study’,BMJ325, pp. 1212–13.Bachman, J. G., Wadsworth, K. N., O’Malley, P. M., et al. (1997),Smoking, drinking, and drug use in youngadulthood: the impacts of new freedoms and new responsibilities,Lawrence Erlbaum, Mahwah, NJ.Begg, S., Vos, T., Barker, B., Stanley, L. and Lopez, A. D. (2007),The burden of disease and injury in Australia2003,AIHW, Canberra. Available from http://www.aihw.gov.au/publications/index.cfm/title/10317.Berghuis, J. P., Swift, W., Roffman, R., Stephens, R. and Copeland, J. (2006), ‘The teen cannabis check-up:exploring strategies for reaching young cannabis users’, in Roffman, R. A. and Stephens, R. S. (eds),Cannabisdependence: its nature, consequences and treatment,Cambridge University Press, Cambridge, UK, pp. 275–92.Bloor, R. N., Wang, T. S., Spanel, P. and Smith, D. (2008), ‘Ammonia release from heated “street” cannabis leafand its potential toxic effects on cannabis users’,Addiction103, pp. 1671–7.Budney, A. J. (2006), ‘Are specific dependence criteria necessary for different substances: how can research oncannabis inform this issue?’,Addiction101 (Supplement 1), pp. 125–33.Butler, M. (2007), ‘Australia’s approach to drugs and driving’,Of Substance: The National Magazine on Alcohol,Tobacco, and Other Drugs5, pp. 24–6.Cameron, L. and Williams, J. (2001), ‘Cannabis, alcohol and cigarettes: substitutes or complements?’,EconomicRecord77, pp. 19–34.Caulkins, J. P., Pacula, R. L., Paddock, S. and Chiesa, J. (2004), ‘What we can — and cannot — expect fromschool-based drug prevention’,Drug and Alcohol Review23, pp. 79–87.Chatwin, C. (2003), ‘Drug policy developments within the European Union: the destabilizing effects of Dutch andSwedish drug policies’,British Journal of Criminology43, pp. 567–82.Copeland, J., Swift, W., Roffman, R. and Stephens, R. (2001), ‘A randomized controlled trial of briefcognitive-behavioral interventions for cannabis use disorder’,Journal of Substance Abuse Treatment21, pp.55–64.Degenhardt, L. and Hall, W. D. (2006), ‘Is cannabis a contributory cause of psychosis?’,Canadian Journal ofPsychiatry51, pp. 556–65.Degenhardt, L., Hall, W. D. and Lynskey, M. T. (2001), ‘The relationship between cannabis use, depression andanxiety among Australian adults: findings from the National Survey of Mental Health and Well-being’,SocialPsychiatry and Psychiatric Epidemiology36, pp. 219–27.Degenhardt, L., Hall, W. D., Warner-Smith, M. and Lynskey, M. T. (2004), ‘Illicit drug use’, in Ezzati, M.,Lopez, A., Rodgers, A. and Murray, C. (eds),Comparative quantification of health risks: global and regionalburden of disease attributable to selected major risk factors,World Health Organization, Geneva, Vol. 1, pp.1109–76.Degenhardt, L., Chiu, W., Sampson, N., et al. (2008), ‘Toward a global view of alcohol, tobacco, cannabis andcocaine use: findings from the WHO World Mental Health Surveys’,PLoS Medicine5, p. e141.
246
Chapter 8: Harm reduction policies for cannabis
Denis, C., Lavie, E., Fatseas, M. and Auriacombe, M. (2006), ‘Psychotherapeutic interventions for cannabisabuse and/or dependence in outpatient settings’,Cochrane Database of Systematic Reviews 3,CD005336.Donnelly, N., Hall, W. D. and Christie, P. (1995), ‘The effects of partial decriminalisation on cannabis use inSouth Australia, 1985 to 1993’,Australian Journal of Public Health19, pp. 281–7.Donnelly, N., Hall, W. D. and Christie, P. (1999),Effects of the Cannabis Expiation Notice Scheme on levels andpatterns of cannabis use in South Australia: evidence from the National Drug Strategy Household Surveys 1985–1995,Australian Government Publishing Service, Canberra.Drummer, O. H., Gerostamoulos, J., Batziris, H., et al. (2004), ‘The involvement of drugs in drivers of motorvehicles killed in Australian road traffic crashes’,Accident Analysis and Prevention36, pp. 239–48.Dutch National Alcohol and Drug Information System (2004), ‘Treatment demand of cannabis clients inoutpatient addiction care in the Netherlands (1994–2001)’,LADIS Bulletin.Earleywine, M. (2002),Understanding marijuana: a new look at the scientific evidence,Oxford University Press,Oxford.Earleywine, M. and Barnwell, S. S. (2007), ‘Decreased respiratory symptoms in cannabis users who vaporize’,Harm Reduction Journal4, p. 11.EMCDDA (2006),Annual report 2006: the state of the drugs problem in Europe,European Monitoring Centre forDrugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/publications/annual-report/2006.EMCDDA (2008),Annual report 2008: the state of the drugs problem in Europe,European Monitoring Centre forDrugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/attachements.cfm/att_64227_EN_EMCDDA_AR08_en.pdf.EMCDDA (2009),General population surveys (GPS),Statistical bulletin, 2009, tables. European Monitoring Centrefor Drugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/stats09/gps.Erickson, P. G. (1980),Cannabis criminals: the social effects of punishment on drug users,Addiction ResearchFoundation, Toronto.Essau, C. (2006), ‘Epidemiological trends and clinical implications of adolescent substance abuse in Europe’, inLiddle, H. A. and Rowe, C. L. (eds),Adolescent substance abuse: research and clinical advances,CambridgeUniversity Press, Cambridge, UK, pp. 129–47.Fergusson, D. M. and Horwood, L. J. (2000), ‘Does cannabis use encourage other forms of illicit drug use?’,Addiction95, pp. 505–20.Fergusson, D. M., Horword, L. J. and Swain-Campbell, N. (2002), ‘Cannabis use and psychosocial adjustment inadolescence and young adulthood’,Addiction97, pp. 1123–35.Fergusson, D. M., Horwood, L. J. and Swain-Campbell, N. R. (2003), ‘Cannabis dependence and psychoticsymptoms in young people’,Psychological Medicine33, pp. 15–21.Gerberich, S. G., Sidney, S., Braun, B. L., et al. (2003), ‘Marijuana use and injury events resulting inhospitalization’,Annals of Epidemiology13, pp. 230–7.Gettman, J. (2000),United States marijuana arrests, part two: racial differences in drug arrests,NationalOrganization for the Reform of Marijuana Laws, Washington, DC. Available at http://norml.org/index.cfm?Group_ID=5326.
247
Harm reduction: evidence, impacts and challenges
Gieringer, D., St Laurent, J. and Goodrich, S. (2004), ‘Cannabis vaporizer combines efficient delivery of THCwith effective suppression of pyrolytic compounds’,Journal of Cannabis Therapeutics4, pp. 7–27.Gorman, D. M. (1995), ‘On the difference between statistical and practical significance in school-based drugabuse prevention’,Drugs: Education, Prevention & Policy2, pp. 275–83.Gowing, L. R., Ali, R. L. and White, J. M. (2000),Respiratory harms of smoked cannabis: DASC monograph 8,Drug and Alcohol Services Council South Australia, Parkside, SA. Available at http://www.dassa.sa.gov.au/webdata/resources/files/MONOGRAPH8.pdf.Greenwald, G. (2009),Drug decriminalization in Portugal: lessons for creating fair and successful drug policies,Cato Institute, Washington, DC.Grier, S. and Bryant, C. A. (2005), ‘Social marketing in public health’,Annual Review of Public Health26, pp.319–39.Grotenhermen, F. (2004), ‘Cannabinoids for therapeutic use: designing systems to increase efficacy andreliability’,American Journal of Drug Delivery2, pp. 229–40.Grotenhermen, F., Leson, G., Berghaus, G., et al. (2007), ‘Developing limits for driving under cannabis’,Addiction102, pp. 1910–17.Hall, W. D. (2006), ‘Cannabis use and the mental health of young people’,Australian and New Zealand Journalof Psychiatry40, pp. 105–13.Hall, W. D. (2006), ‘The mental health risks of adolescent cannabis use’,PLoS Medicine3, pp. 159–62.Hall, W. D. and Homel, R. (2007), ‘Reducing cannabis-impaired driving: is there sufficient evidence for drugtesting of drivers?’,Addiction102, pp. 1918–19.Hall, W. D. and Lynskey, M. T. (2005), ‘Is cannabis a gateway drug? Testing hypotheses about the relationshipbetween cannabis use and the use of other illicit drugs’,Drug and Alcohol Review24, pp. 39–48.Hall, W. D. and MacPhee, D. (2002), ‘Cannabis use and cancer’,Addiction97, pp. 243–7.Hall, W. D. and Pacula, R. L. (2003),Cannabis use and dependence: public health and public policy,CambridgeUniversity Press, Cambridge, UK.Hall, W. D. and Swift, W. (2000), ‘The THC content of cannabis in Australia: evidence and implications’,Australian and New Zealand Journal of Public Health24, pp. 503–08.Hall, W. D., Teesson, M., Lynskey, M. T. and Degenhardt, L. (1999), ‘The 12-month prevalence of substance useand ICD-10 substance use disorders in Australian adults: findings from the National Survey of Mental Health andWell-being’,Addiction94, pp. 1541–50.Hall, W. D., Degenhardt, L. and Patton, G. C. (2008a), ‘Cannabis abuse and dependence’, in Essau, C. A. (ed.),Adolescent addiction: epidemiology, treatment and assessment,Academic Press, London, pp. 117–48.Hall, W. D., Degenhardt, L. and Sindicich, N. (2008b), ‘Illicit drug use and the burden of disease’, inHeggenhougen, K. and Quah, S. (eds),International encyclopedia of public health,Elsevier, Amsterdam, pp.523–30.Harkin, A., Anderson, P., Goos, P. (1997),Smoking, drinking and drug taking in the European Region,WHORegional Office for Europe, Copenhagen.Hazekamp, A., Ruhaak, R., Zuurman, L., van Gerven, J. and Verpoorte, R. (2006), ‘Evaluation of a vaporizingdevice (Volcano) for the pulmonary administration of tetrahydrocannabinol’,Journal of Pharmaceutical Sciences95, pp. 1308–17.
248
Chapter 8: Harm reduction policies for cannabis
Henquet, C., Krabbendam, L., Spauwen, J., et al. (2004), ‘Prospective cohort study of cannabis use,predisposition for psychosis, and psychotic symptoms in young people’,BMJ330, p. 11.Henstridge, J., Homel, R. and Mackay, P. (1997),The long-term effects of random breath testing in four Australianstates: a time series analysis,Federal Office of Road Safety, Canberra. Available at http://www.infrastructure.gov.au/roads/safety/publications/1997/Alc_Random.aspx.Hughes, C. E. and Stevens, A. (2007),The effects of decriminalization of drug use in Portugal,Briefing paper 14,The Beckley Foundation Drug Policy Program, London.Human Rights Watch (2000),Punishment and prejudice: Racial disparities in the war on drugs,Human RightsWatch Report 12/2, New York. Available at http://www.hrw.org/legacy/reports/2000/usa/.Iversen, L. (2007),The science of marijuana,Oxford University Press, Oxford.Jeffery, D., Ley, A., McLaren, S. and Siegfried, N. (2004), ‘Psychosocial treatment programmes for people withboth severe mental illness and substance misuse’,Cochrane Database of Systematic Reviews 2000,2, CD001088.Jones, A. W., Holmgren, A. and Kugelberg, F. C. (2008), ‘Driving under the influence of cannabis: a 10-yearstudy of age and gender differences in the concentrations of tetrahydrocannabinol in blood’,Addiction103, pp.452–61.Kaplan, J. (1970),Marijuana: the new prohibition,World Publishing Company, New York.Kavanagh, D. J. (1995), ‘An intervention for substance abuse in schizophrenia’,Behaviour Change12, pp. 20–30.Laumon, B., Gadegbeku, B., Martin, J. L. and Biecheler, M. B. (2005), ‘Cannabis intoxication and fatal roadcrashes in France: population based case-control study’,BMJ331, p. 1371.Lehman, A. F., Herron, J. D., Schwartz, R. P. and Myers, C. P. (1993), ‘Rehabilitation for adults with severe mentalillness and substance use disorders: a clinical trial’,Journal of Nervous and Mental Disease181, pp. 86–90.Lenton, S. (2000), ‘Cannabis policy and the burden of proof: is it now beyond reasonable doubt that cannabisprohibition is not working?’,Drug and Alcohol Review19, pp. 95–100.Lenton, S., Bennett, M. and Heale, P. (1999a),The social impact of a minor cannabis offence under strict prohibition:the case of Western Australia,National Centre for Research into the Prevention of Drug Abuse, Perth.Lenton, S., Christie, P., Humeniuk, R., et al. (1999b),Infringement versus conviction: the social impact of a minorcannabis offence under a civil penalties system and strict prohibition in two Australian states,CommonwealthDepartment of Health and Aged Care, Canberra.Llewellyn, C. D., Linklater, K., Bell, J., Johnson, N. W. and Warnakulasuriya, S. (2004), ‘An analysis of risk factorsfor oral cancer in young people: a case-control study’,Oral Oncology40, pp. 304–13.Lynskey, M. T. and Hall, W. D. (2000), ‘The effects of adolescent cannabis use on educational attainment: areview’,Addiction96, pp. 433–43.MacCoun, R. and Reuter, P. (1997), ‘Interpreting Dutch cannabis policy: reasoning by analogy in the legalizationdebate’,Science278, pp. 47–52.Macleod, J., Oakes, R., Copello, A., et al. (2004), ‘Psychological and social sequelae of cannabis and otherillicit drug use by young people: a systematic review of longitudinal, general population studies’,Lancet363, pp.1579–88.Mann, R. E., Stoduto, G., Macdonald, S. and Brands, B. (2008), ‘Cannabis use and driving: implications forpublic health and transport policy’, in Sznitman, S. R., Olsson, B., Room, R. (eds),A cannabis reader: global issuesand local experiences,EMCDDA, Lisbon, pp. 173–98.
249
Harm reduction: evidence, impacts and challenges
Marselos, M. and Karamanakos, P. (1999), ‘Mutagenicity, developmental toxicity and carcinogeneity ofcannabis’,Addiction Biology4, pp. 5–12.Martin, G. and Copeland, J. (2008), ‘The adolescent cannabis check-up: randomized trial of a brief interventionfor young cannabis users’,Journal of Substance Abuse Treatment34, pp. 407–14.Mehra, R., Moore, B. A., Crothers, K., Tetrault, J. and Fiellin, D. A. (2006), ‘The association between marijuanasmoking and lung cancer: a systematic review’,Archives of Internal Medicine166, pp. 1359–67.Melamede, R. (2005), ‘Harm reduction: the cannabis paradox’,Harm Reduction Journal2, p. 17.Miller, W. R. and Sovereign, R. G. (1989), ‘The check-up: a model for early intervention in addictive behaviors’,in Leberg, T., Miller, W., Nathan, G. and Marlatt, G. (eds.),Addictive behaviors: prevention and early intervention,Swets and Zeitlinger, Amsterdam, pp. 219–31.Moore, T. H., Zammit, S., Lingford-Hughes, A., et al. (2007), ‘Cannabis use and risk of psychotic or affectivemental health outcomes: a systematic review’,Lancet370, pp. 319–28.Mueser, K. T., Bellack, A. S. and Blanchard, J. J. (1992), ‘Comorbidity of schizophrenia and substance abuse:implications for treatment’,Journal of Consulting and Clinical Psychology60, pp. 845–56.Mura, P., Kintz, P., Ludes, B., et al. (2003), ‘Comparison of the prevalence of alcohol, cannabis and other drugsbetween 900 injured drivers and 900 control subjects: results of a French collaborative study’,Forensic ScienceInternational133, pp. 79–85.Nordstrom, B. R. and Levin, F. R. (2007), ‘Treatment of cannabis use disorders: a review of the literature’,American Journal of Addiction16, pp. 331–42.Nutt, D., King, L., Saulsbury, W., Blakemore, C. (2007), ‘Development of a rational scale to assess the harm ofdrugs of potential misuse’,Lancet369 (9566), pp. 1047–53.Pacula, R. L., Chriqui, J. F. and King, J. (2004),Marijuana decriminalization: what does it mean in the UnitedStates?,Working Paper WR-126, RAND, Santa Monica. Available at http://www.rand.org/pubs/working_papers/WR126/.Pakes, F. (2004), ‘The politics of discontent: the emergence of a new criminal justice discourse in theNetherlands’,The Howard Journal43, pp. 284–98.Patton, G. C., Coffey, C., Carlin, J. B., et al. (2002), ‘Cannabis use and mental health in young people: cohortstudy’,BMJ325, pp. 1195–8.Ramaekers, J. G., Berghaus, G., van Laar, M. and Drummer, O. H. (2004), ‘Dose related risk of motor vehiclecrashes after cannabis use’,Drug and Alcohol Dependence73, pp. 109–19.Roffman, R. A. and Stephens, R. S. (eds) (2006),Cannabis dependence: its nature, consequences and treatment,Cambridge University Press, Cambridge, UK.Room, R., Fischer, B., Hall, W. D., Lenton, S. and Reuter, P. (2008),Cannabis policy: moving beyond stalemate, TheGlobal Cannabis Commission Report,Beckley Foundation, Oxford, UK. Available at http://www.beckleyfoundation.org/.Rosenblatt, K. A., Daling, J. R., Chen, C., Sherman, K. J. and Schwartz, S. M. (2004), ‘Marijuana use and risk oforal squamous cell carcinoma’,Cancer Research64, pp. 4049–54.Saha, S., Chant, D., Welham, J. and McGrath, J. (2005), ‘A systematic review of the prevalence ofschizophrenia’,PLoS Medicine2, p. e141.
250
Chapter 8: Harm reduction policies for cannabis
SAMHSA (2006),Results from the 2005 National Survey on Drug Use and Health: Detailed tables. Prevalenceestimates, standard errors, p values. Section 1.Substance Abuse and Mental Health Administration, Office ofApplied Studies, Rockville, MD. Available at http://www.oas.samhsa.gov.Shand, F., Gates, J., Fawcett, J. and Mattick, R. (2003),The treatment of alcohol problems: a review of the evidence,Commonwealth Department of Health and Ageing, Canberra.Sidney, S., Quesenberry, C. P., Jr., Friedman, G. D. and Tekawa, I. S. (1997), ‘Marijuana use and cancerincidence (California, United States)’,Cancer Causes and Control8, pp. 722–8.Single, E. W. (1989), ‘The impact of marijuana decriminalization: an update’,Journal of Public Health Policy9, pp.456–66.Smart, R. G. and Ogborne, A. C. (2000), ‘Drug use and drinking among students in 36 countries’,AddictiveBehaviors25, pp. 455–60.Solowij, N. (1998),Cannabis and cognitive functioning,Cambridge University Press, Cambridge, UK.Stephens, R. S., Roffman, R. A., Copeland, J. and Swift, W. (2006), ‘Cognitive behavioral and motivationalenhancement treatments for cannabis dependence’, in Roffman, R. A. and Stephens, R. S. (eds),Cannabisdependence: its nature, consequences and treatment,Cambridge University Press, Cambridge, UK, pp. 131–53.Stephens, R. S., Roffman, R. A., Fearer, S. A., Williams, C. and Burke, R. S. (2007), ‘The marijuana check-up:promoting change in ambivalent marijuana users’,Addiction102, pp. 947–57.Swift, W., Copeland, J. and Lenton, S. (2000), ‘Cannabis and harm reduction’,Drug and Alcohol Review19, pp.101–12.Tashkin, D. P. (1999), ‘Effects of cannabis on the respiratory system’, in Kalant, H., Corrigall, W., Hall, W. D. andSmart, R. (eds),The health effects of cannabis,Centre for Addiction and Mental Health, Toronto, pp. 311–45.Tobler, N. S., Lessard, T., Marshall, D., Ochshorn, P. and Roona, M. (1999), ‘Effectiveness of school-based drugprevention programs for marijuana use’,School Psychology International20, pp. 105–37.Toumbourou, J., Williams, J., Waters, E. and Patton, G. (2004), ‘What do we know about preventing drug-relatedharm through social developmental intervention with children and young people?’, in Stockwell, T., Gruenewald,P., Toumbourou, J. and Loxley, W. (eds),Preventing harmful substance use: the evidence base for policy and practice,John Wiley & Sons Ltd, Chichester, pp. 87–100.UNODC (United Nations Office on Drugs and Crime) (2006),World drug report 2006. Volume 1: Analysis,UnitedNations Office on Drugs and Crime, Vienna.UNODC (2007),World drug report 2007. Volume 1: Analysis,United Nations Office on Drugs and Crime, Vienna.van Os, J., Bak, M., Hanssen, M., et al. (2002), ‘Cannabis use and psychosis: a longitudinal population-basedstudy’,American Journal of Epidemiology156, pp. 319–27.White, D. and Pitts, M. (1998), ‘Educating young people about drugs: a systematic review’,Addiction93, pp.1475–87.Williams, J. (2004), ‘The effects of price and policy on marijuana use: what can be learned from the Australianexperience?’Health Economics13, pp. 123–37.Wodak, A., Reinarman, C. and Cohen, P. (2002), ‘Cannabis control: costs outweigh benefits’,BMJ324, pp.105–06.
251
Harm reduction: evidence, impacts and challenges
Zammit, S., Allebeck, P., Andréasson, S., Lundberg, I. and Lewis, G. (2002), ‘Self reported cannabis use asa risk factor for schizophrenia in Swedish conscripts of 1969: historical cohort study’,BMJ325, pp. 1199–201.Zhang, Z. F., Morgenstern, H., Spitz, M. R., et al. (1999), ‘Marijuana use and increased risk of squamous cellcarcinoma of the head and neck’,Cancer Epidemiology, Biomarkers and Prevention8, pp. 1071–8.Zimmer, L., Morgan, J. P. (1997),Marijuana myths, marijuana facts: a review of the scientific evidence,TheLindesmith Center, New York.
252
Chapter 9Harm reduction policies for tobaccoCoral Gartner, Wayne Hall and Ann McNeill
AbstractTobacco smoking is the leading cause of preventable premature mortality and disability inEuropean and other developed countries. This chapter first reviews strategies that (1) aim toreduce harm to non-smokers (public smoking bans and reduced ignition propensitycigarettes) and (2) aim to reduce harm to the smoker who is unable or unwilling to quitnicotine use, namely, regulating the harmfulness of cigarettes, and encouraging smokers toswitch to less harmful nicotine products. The putative tobacco harm reduction productsdiscussed include: modified tobacco cigarettes and cigarette-like devices, smokeless tobaccoproducts and pharmaceutical nicotine products. The evidence for the harm reductionpotential of each of these is discussed, as are adverse public health outcomes that maypotentially arise from their promotion. The chapter concludes with a description of the mostpromising options for promoting tobacco harm reduction.Keywords:smokeless tobacco, snus, reduced ignition propensity cigarettes, smoking bans,potential reduced exposure products, pharmaceutical nicotine.
IntroductionTobacco can be smoked as cigarettes, in a pipe, or as cigars or used via non-smokedproducts such as chewing tobacco or oral and nasal snuff. Nicotine is the primary substanceresponsible for tobacco dependence but the majority of harm caused by tobacco use is notfrom nicotine but from the by-products of smoked tobacco (e.g. fine particulates, carcinogens,and noxious gases including carbon monoxide). Cigarettes are the most addictive andhazardous tobacco product, because cigarette smoke is readily drawn deep into the lungswhere it is rapidly absorbed into the bloodstream and from which nicotine quickly reachesthe brain (Benowitz, 2008).In Europe, as in many regions of the world, the cigarette has become the dominant form oftobacco use over the past century (Berridge, 2007). The rise in the popularity of the cigarettewas followed with a lag of several decades by increases in tobacco-caused diseasesincluding cancers, pulmonary and cardiovascular diseases. By mid century tobacco smokinghad become the leading cause of preventable premature mortality and disability in Europeand other developed countries. Cigarette smoking is currently responsible for around730 000 deaths in the European Union (EU) each year (including 80 000 from passivesmoking) (ASPECT Consortium, 2004).Smoking prevalence has declined in most western European countries over the past 40 years,but prevalence remains high in many eastern European countries (ASPECT Consortium,255
Harm reduction: evidence, impacts and challenges
2004; WHO Regional Office for Europe, 2007). The disparities in smoking prevalence acrossEurope largely reflect differences in the intensity with which tobacco control policies havebeen implemented, such as increasing cigarette taxes, banning cigarette advertising, publicmass media anti-smoking campaigns and restricting smoking in indoor public spaces(ASPECT Consortium, 2004; WHO Regional Office for Europe, 2003; WHO Regional Officefor Europe, 2007).Policies that encourage existing smokers to quit and discourage non-smokers from startingremain the most effective ways of reducing tobacco-related harm (World Bank, 2003).Nonetheless, even in countries that have most rigorously enforced these types of policies(Australia, the United States, Canada, the United Kingdom and Sweden), none have reducedoverall smoking prevalence below one in six adults. Plausible projections show that morethan 10 % of adults will be smoking in another 20 years if current rates of cessation andinitiation continue (Gartner et al., 2009; Kemm, 2003; Mendez et al., 1998).The persistence of smoking in a substantial minority of adults has prompted some toadvocate tobacco harm reduction (THR) policies as an addition to conventional strategiesthat promote abstinence from tobacco. Harm reduction policies are generally those that‘attempt to prevent problems by targeting risky contexts or patterns of use, or by moderatingthe relation between use and problem outcomes, without necessarily affecting overall rates ofuse’ (Toumbourou et al., 2007, pp. 1398–9). In the case of THR, this approach involvesattempting to reduce the harmfulness of tobacco use without necessarily advocating cessationor abstinence, typically by advocating the use of much less harmful forms of tobacco ornicotine use.
Policies that reduce the harm to othersPublic smoking bansNon-smokers who are exposed to second-hand smoke (the emissions from the end of litcigarettes and the exhaled smoke from a smoker) are at increased risk of many of the samediseases that affect smokers (US Department of Health and Human Services, 2006). Workersin smoky environments, such as bar staff, are particularly at risk due to their regular andprolonged exposure. Legislated bans on smoking in enclosed public spaces such as officebuildings, restaurants, cafes, bars and clubs provide protection of employees and patronsand are the most widespread and non-controversial tobacco harm reduction policy. Researchhas shown that public smoking bans in countries like the United States and Australia havebeen effective in reducing exposure to second-hand smoke in these previously smokyenvironments (Hopkins et al., 2001). There is also evidence that these policies can provideimmediate population health improvements, such as a reduction in the number ofhospitalisations for acute coronary events (Pell et al., 2008).A number of European countries have recently introduced indoor public smoking bans (forexample, Republic of Ireland, United Kingdom), but many countries still do not havecomprehensive smoking bans (Joossens and Raw, 2007). To be effective at reducing the256
Chapter 9: Harm reduction policies for tobacco
exposure of non-smokers, these bans need to cover all enclosed areas and should alsoextend to outdoor areas that are serviced by waiting staff. Smoking bans also have theadded benefit of increasing cessation in the smoking population by reducing theopportunities to smoke and contributing to the de-normalisation of smoking (Fichtenbergand Glantz, 2002).Reduced ignition propensity (RIP) cigarettesFires started by cigarettes cause substantial damage to property and loss of life. Internaltobacco industry documents show that the industry knew how to reduce the ignitionpropensity of cigarettes many years ago (Gunja et al., 2002) by reducing tobacco density,paper porosity and cigarette circumference, eliminating burn additives and by increasingthe length of filters (Chapman and Balmain, 2004). Legislation requiring cigarettes to meetRIP performance standards has now been implemented in 22 US states and Canada(Arnott and Berteletti, 2008). In 2007, the EU Member States endorsed plans to develop amandatory standard to reduce the ignition propensity of cigarettes sold in the EU (Arnottand Berteletti, 2008; Commission of the European Communities, 2008). An evaluation ofNew York’s RIP standard (implemented in 2004), showed that it substantially reduced theignition propensity of cigarettes sold in that state, largely via ‘paper banding’, withoutincreasing the toxicity of the emissions (Alpert et al., 2005). There is as yet no evidence thatthe introduction of RIP standards has reduced cigarette-related fires. Nevertheless,implementation of a RIP performance standard in Europe would not be costly to the public,would have very little risk of producing adverse outcomes and could reduce the number offires caused by discarded cigarettes.
Policies that reduce harm to the smokerThe main putative tobacco harm reduction products in order of decreasing relativeharmfulness are modified tobacco cigarettes and cigarette-like devices, smokeless tobacco(SLT) products and pharmaceutical nicotine (PN) products (Stratton et al., 2001).Modified tobacco cigarettes and cigarette-like devicesRegulating the harmfulness of cigarette emissionsThe tobacco industry began developing a ‘safer’ cigarette in response to the emergingevidence of the harm from cigarette smoking in the 1950s (Glantz et al., 1996). The firstexample was the filtered cigarette, followed by so-called light, low-tar and low-nicotinecigarettes in the 1980s (Stratton et al., 2001). These cigarette modifications, which consistedof the addition of tiny ventilation holes in the side of the filter to dilute the smoke with airdrawn in through these holes, were popular with smokers; however, they did not reduce thehealth risks of smoking as smokers compensated by drawing harder on the cigarette,covering the filter ventilation holes and smoking the cigarettes down to a shorter butt length.Research later revealed that the cigarette manufacturers knew these were not genuine257
Harm reduction: evidence, impacts and challenges
reduced harm products, but marketed them to reassure health-conscious smokers anddiscourage quitting (Glantz et al., 1996).The World Health Organization’s Study Group of Tobacco Product Regulation (TobReg)advocates mandatory maximum permissible levels of key toxicants in mainstream cigarettesmoke (Burns et al., 2008) and the tobacco industry has developed and marketed cigarettesmade with low nitrosamine tobacco and carbon filters, both of which are claimed to exposesmokers to fewer toxins than regular cigarettes (Hatsukami et al., 2004; Rees et al., 2008). Amajor problem with this approach is that reductions in some toxins are often achieved byincreasing others (King et al., 2007). Given that tobacco smoke contains more than 4 000different chemicals, it will be difficult to achieve a substantial reduction in overall harmfulness(Stratton et al., 2001). Futhermore, there is no evidence that reducing or removing knowntoxins in cigarettes will produce observable reductions in smoking-related lung cancer(Pankow et al., 2007), yet publicity around mandating these changes may give consumersthe impression that they do significantly reduce harm. Monitoring and enforcing a cigaretteemissions standard will also require substantial laboratory and regulatory resources that mayarguably be better used in other ways.Cigarette-like devicesThe tobacco industry has also marketed cigarette-like devices that aim to minimise tarsand maximise nicotine by heating tobacco to produce an aerosol or vapour rather thansmoke (for example, Eclipse, Premier, Accord and Heatbar) (Shiffman et al., 2002a;Stratton et al., 2001). Some of these products reduce emissions of one or more key toxins,but some studies report higher emissions of others (Breland et al., 2002; Breland et al.,2006; Fagerström et al., 2000; Stratton et al., 2001). Given the long latency of manytobacco-related diseases, it will take several decades before we know whether theseproducts substantially reduce tobacco-related mortality and morbidity. Given thesedifficulties, we should arguably abandon attempts to reduce the harmfulness of cigaretteemissions by modifying cigarettes or producing cigarette-like tobacco products in favourof harm reduction using non-smoked forms of tobacco and clean nicotine products(Stratton et al., 2001).Smokeless tobacco (SLT) productsSLT products present greater opportunity for THR than smoked tobacco because there isno combustion/vaporisation and therefore no risk of respiratory disease, fire or passivesmoking. SLT products include traditional chewing tobacco and snuff, and new productssuch as compressed tobacco lozenges, tobacco chewing gum and dissolvable strips(Hatsukami et al., 2007; Stepanov et al., 2006). Most policy attention has focused on aform of moist oral snuff used in Sweden, known as snus (see box on p. 262). It has muchlower levels of tobacco-specific nitrosamines than snuffs marketed in the United States andelsewhere because it is produced by pasteurisation rather than fermentation (Hoffmann etal., 1995; Österdahl et al., 2004; Ramström, 2000). Levels of nitrosamines in Swedish snushave decreased over the past 20 or so years in response to the development of an258
Chapter 9: Harm reduction policies for tobacco
industry standard (Hatsukami et al., 2007; Österdahl et al., 2004). The development ofportion snus in the 1970s (tea-bag-like sachets of snus) has produced a more user-friendlyversion that has increased prevalence of snus use among Swedish men. The fact that untilrecently snus was taxed at a much lower rate than cigarettes may also have contributedto its increased popularity. Increased snus use by Swedish men has been accompanied bydecreased cigarette smoking and tobacco-related disease mortality (Foulds et al., 2003;Ramström, 2003).A major barrier to the adoption of this form of harm reduction is the ban on the sale of theleast harmful smokeless tobacco products in many countries. In Australia and NewZealand, for example, oral snuff and chewing tobacco products cannot be sold(Commonwealth of Australia, 1974; Parliament of New Zealand, 1990). With the exceptionof Sweden, the same is true in all EU Member States, where the sale of these tobaccoproducts is prohibited, although chewing tobacco and nasal snuff can be sold (EuropeanCourt of Justice, 2004).Pharmaceutical nicotine (PN)PN products in the form of gum, patches, inhalers and sprays have been available formany years. A new PN product under development is an oral nicotine pouch that mimicsportion snus (Fagerström and Jiménez-Ruiz, 2008). PN is generally a safe (except perhapsin pregnancy), modestly effective and cost-effective way to help smokers to quit (Bertram etal., 2007; Stead et al., 2008), or, potentially, also as a long-term alternative to cigarettesmoking (Warner et al., 1997). These products have minimal risk of abuse, in part becauseof their design. The long-term use of PN appears to be safe, as no treated morbidity ormortality was observed in five years of follow-up of nicotine gum users (Murray et al.,1996). Long-term use of PN in ex-smokers may also help prevent relapse to smoking (Hajeket al., 2007; Medioni et al., 2005).The major disadvantages of PN are that, like other smoking cessation aids (bupropion,varenicline), most smokers who use it do not succeed in quitting (Nides, 2008; Shiffman etal., 2002b), and it has not been taken up by smokers as an alternative to smoking despiteits wide availability in many developed countries. This seems to be because these productshave been engineered for smoking cessation, with the aim of minimising their abuse bydelivering a lower nicotine dose at a slower speed to cigarettes. They are also notmarketed as long-term alternatives to tobacco smoking. For these products to gainpopularity, PN regulation would need to be relaxed to allow these products to be mademore attractive to inveterate smokers.Recreational nicotine productsThe marketing of the ‘e-cigarette’, a device that looks like a standard tobacco cigarette butcontains only nicotine in a carrier vapour, is a recent attempt to commercialise arecreational nicotine product. Its similarity to cigarettes has led most tobacco controladvocates to refer to it as a cigarette-like device. The e-cigarette produces a propylene259
Harm reduction: evidence, impacts and challenges
glycol vapour and has a glowing red tip to simulate a lit cigarette. The manufacturers havenot marketed it as a smoking cessation aid and this has created regulatory barriers insome countries (for example, Australia and New Zealand) (National Drugs and PoisonsScheduling Committee, 2009; New Zealand Public Health Directorate, 2006). Some EUMember States have defined e-cigarettes as medical devices and require them to obtain aConfirmatory European (CE) mark before sale (e.g. Denmark, Austria) (Danish MedicinesAgency, 2009; European Commission Health and Consumer Protection Directorate-General, 2008). A safety assessment of one brand of e-cigarette funded by themanufacturer suggests the product may be relatively safe (Laugesen, 2008; Laugesen etal., 2008), but there are no data on the patterns of use in smokers or uptake by non-smokers in countries where these products are sold, and there are no safety studies bygroups that are independent of the industry.There are claims in the popular media in the United Kingdom that the e-cigarette is beingused in response to smoking bans in pubs and clubs (Sikora, 2007). Critics of thee-cigarette also argue that it maintains a visible smoking-like behaviour that mayundermine the de-normalisation of smoking produced by public smoking bans (Chapmanand Freeman, 2008). The substantial cost of the device and its replacement cartridges, thegimmicky nature of the smoke and glowing tip, and the regulatory hurdles in mostcountries will probably limit its use for THR (Arendt, 2008). However, more data is neededon whether smokers find these devices an acceptable substitute for smoking regularcigarettes.The e-cigarette illustrates the inadequacy of current regulatory structures. Claims aboutaiding cessation would result in the e-cigarette being classified as a medicine and wouldrequire safety, quality and efficacy data before being marketed. If no such claims are made,the e-cigarette is likely to be regulated like tobacco cigarettes, and would then be subject toall the regulations that apply to tobacco products. Neither set of regulations are appropriatefor e-cigarettes, the relative harmfulness of which is likely to fall somewhere between tobaccocigarettes and PN.
Will tobacco harm reduction products reduce harm to users?There is no evidence that modified smoked tobacco products and cigarette-like devicessubstantially reduce harm. Experience with ‘light’ cigarettes also provides strong reasonsfor not allowing them to be promoted as THR products (Stratton et al., 2001; Warner,2001). ‘Light’ cigarettes failed to reduce harm in smokers due to compensatory changes inthe way they were smoked, such as inhaling more deeply, smoking a greater number ofcigarettes and more of each cigarette, and blocking ventilation holes designed to dilutesmoke exposure (Stratton et al., 2001). The mistaken image of a less harmful cigarette alsoprovided reassurance to health-concerned smokers, which discouraged quitting. Similarcompensatory changes, and/or ‘risk swapping’ by decreasing some toxins whilstincreasing others, and false reassurance of safety, are likely to limit any benefits from THRproducts that involve the combustion or vaporisation of tobacco (e.g. Gray, 2004; Pierce,2002; Stratton et al., 2001).260
Chapter 9: Harm reduction policies for tobacco
This argument does not apply to THR using PN and low nitrosamine SLT (LNSLT). The safetyof PN is well established in the short to medium term with users having been followed forup to five years (Murray et al., 1996). PN may carry some residual health risks, such as anincreased risk of cardiovascular disease arising from chronic nicotine intake, and adversefoetal outcomes if used in pregnancy, but these effects are small by comparison with thoseof cigarette smoking (Benowitz, 2000). Literature reviews of the health effects of SLT(Broadstock, 2007; Royal College of Physicians, 2007; SCENIHR, 2008) have concludedthat some forms of SLT such as Swedish snus, which is low in nitrosamines, are significantlyless harmful than smoking cigarettes. SLT use is not associated with respiratory diseases,including lung cancer and chronic obstructive pulmonary disease (COPD), but somepotential health risks remain, namely oral and pancreatic cancer, cardiovascular diseaseand type 2 diabetes. Even so, these risks appear to be much lower than those of smoking.An expert panel estimated on the basis of the epidemiological literature that the overall riskof tobacco-related mortality in LNSLT users was 10 % of the risk of cigarette smokers (Levyet al., 2004). Epidemiological modelling of the aggregate health effects of quitting tobaccoand switching from smoking to LNSLT suggest there is little difference in years of healthylife gained by those who quit tobacco and those who switch to LNSLT (Gartner et al.,2007b) (see box on p. 262).
Effects of tobacco harm reduction on aggregate harmWhether THR produces a net benefit or harm depends on: the relative harmfulness of theTHR product compared to regular cigarettes; how popular the THR product is among currentsmokers, ex-smokers and never smokers; and its effect on rates of smoking cessation andinitiation. The risks of overall net harm are greatest for modified cigarettes and cigarette-likedevices, because these produce the least reduction in risk and could discourage cessation inmuch the same way as ‘light’ cigarettes did.Epidemiological modelling of the aggregate health effects of smoking and LNSLT usesuggests that relaxations of bans on LNSLT use would only produce net harm if theseproducts proved much more attractive to non-smokers than to smokers; led non-smokers tostart to smoke; and/or maintained cigarette use in smokers by dual use rather than completeswitching (Gartner et al., 2007a) (see box on p. 262). These putative effects of LNSLT havenot been observed in Sweden and there are good reasons for thinking that they are unlikelyto occur. As Kozlowski and colleagues (Kozlowski et al., 2001) have shown, PN would stillproduce a net population health gain, even if we made: (1) the most pessimistic assumptionsabout its residual health risks; and (2) we assumed that PN was used by the whole adultpopulation (Kozlowski et al., 2001). A similar argument can be made for LNSLT.
261
Harm reduction: evidence, impacts and challenges
Epidemiological modelling of the aggregate health effects of lifelong smoking, ex-smoking,switching to snus and lifelong snus useGartner et al (2007b) used multistate life tables and expert panel risk estimates to model theyears of healthy life lost (YHLL) due to lifelong smoking, quitting tobacco use, switching fromsmoking to snus and lifelong snus use without smoking. The results showed that smokers whoswitched to snus would achieve health gains nearly as good as quitting all tobacco use. Menwho switched from smoking to snus would lose 1.2–3.6 months of healthy life and women1.2–4.8 months compared to smokers who quit tobacco altogether.Figure 9.1:Years of healthy life lost by lifelong smoking, ex-smoking, switching to snus andlifelong snus use65432Years of healthy life lost1054321035–3940–4445–4950–5455–5960–6465–6970–7475+WomenMen
Current age*Lifelong smokersSmokers who switch to snusSmokers who quitLifelong snus user who never smoked*Age at quittingor switching
262
Chapter 9: Harm reduction policies for tobacco
‘Gateway’ effectsThere is no evidence that PN in its currently available forms encourages non-smokers totake up smoking (Gerlach et al., 2008; Klesges et al., 2003). This situation could change ifPN was re-engineered to be more rapidly absorbed and produced higher blood nicotine,and if it were allowed to be marketed as a recreational nicotine product, like smokedtobacco. The current marketing of the e-cigarette in some countries may allow anassessment of the risks of more liberal regulation of the nicotine market, although thenicotine dose and delivery of currently marketed e-cigarettes may be too similar to existingPN cessation aids for a full assessment. The cost of the e-cigarette may also preclude itswidescale uptake.
The Swedish experienceSnus is a traditional moist oral snuff used in Sweden. Snus use declined as cigarettes becamepopular. However, a marketing campaign that started in the 1970s reinvigorated the snusmarket and resulted in increased uptake among Swedish men, with as many Swedish mennow using snus as smoking cigarettes (Ramström, 2000). The Swedish experience has beendescribed as a natural experiment of tobacco harm reduction (Brandt, 2007; Henningfieldand Fagerström, 2001) as the shift from cigarette smoking to snus use has occurred withoutthe support of the Swedish health community.Figure 9.2:Prevalence of daily smoking for men and women (ages 18–70 years) in Sweden1976–2002 and prevalence of daily snus use for men (age 18–70 years) inSweden 1976–200250454035Prevalence (%)30252015105019761980198419881992Year19962000Daily smoking menDaily smoking womenDaily snus men
Source:Reproduced from Foulds et al., 2003.
The increase in snus use was accompanied by a decline in cigarette smoking from 40 % in1976 to 15 % in 2002 (see Figure 9.2). Contrary to the gateway hypothesis, there were noincreases in smoking among adolescent males, who were the heaviest users of snus. Instead,snus use appears to deter smoking initiation in young men and promote smoking cessation in
263
Harm reduction: evidence, impacts and challenges
older men (Foulds et al., 2003; Furberg et al., 2005; Ramström, 2000). Most critically, theincrease in snus use was accompanied by a decline in lung cancer mortality and the absenceof an increase in either cardiovascular mortality or head and neck cancers (Foulds et al.,2003). The plausibility of a causal relationship between increased snus use and these goodhealth outcomes was strengthened by the absence of any similar changes in smokingprevalence or lung cancer mortality in Swedish women, who did not adopt snus at the samerate as men (Foulds et al., 2003).Figure 9.3:Lung cancer incidence for men and women in Sweden and Norway 1960–99 forage-standardised rates per 100 000 inhabitants based upon census populationin each country
Age-standardised rates per 100 000
807060504030201001960
Men in NorwayMen in SwedenWomen in NorwayWomen in Sweden
1964
1968
1972
1976
1980
Year
1984
1988
1992
1996
2000
Source:Reproduced from Foulds et al., 2003.
Whether SLT serves as a gateway to smoking is a more contentious issue. The Swedishexperience with snus contradicts the pessimistic view about the population impact of THR(Foulds et al., 2003) (see box on p. 263). The relationship between SLT use and smokinghas been more varied in American studies. In some studies the same pattern has beenreported as in Sweden (Ault et al., 2004; O’Connor et al., 2005). Other studies, however,have reported an apparent ‘gateway’ effect with young SLT users ‘graduating’ tosmoking (Haddock et al., 2001). It is challenging to quantify how much smoking isattributable to prior SLT use because it is difficult to determine whether smokers who usedSLT before cigarettes would have become smokers in the absence of SLT use. Oneanalysis suggests that when the demographic and social factors associated with smokinginitiation are taken into account, SLT does not appear to increase the uptake of smoking(Timberlake et al., 2009). In the United States, public health authorities may have alsoinadvertently encouraged SLT users to switch to cigarettes by claiming that the healthrisks of SLT are the same as those of smoking (Kozlowski and Edwards, 2005; Kozlowskiand O’Connor, 2003; Waterbor et al., 2004).
264
Chapter 9: Harm reduction policies for tobacco
‘Dual use’The use of PN to relieve nicotine withdrawal during periods of temporary abstinence is anapproved use in some countries (for example, United Kingdom, Republic of Ireland, France,Austria, Denmark, Norway, Portugal, Brazil, Venezuela, New Zealand and Canada), as is itsuse to reduce smoking in preparation for quitting (ASH UK, 2008). Some studies havereported that users of PN often use it for purposes other than cessation (Hammond et al.,2008; Klesges et al., 2003). Such use does not appear to reduce quitting (Levy et al., 2007);indeed, such use may increase cessation in smokers who were not initially interested inquitting (Carpenter et al., 2004; Le Houezec and Sawe, 2003).The tobacco industry has begun to market SLT for smokers to use when smoking is notpermitted (Gartner et al., 2007a). This pattern of use could perpetuate smoking by reducingthe incentive to quit provided by public smoking bans (Fichtenberg and Glantz, 2002).Alternatively, such use of SLT could lead some smokers to switch fully to SLT or even to quittobacco use, as happens with PN. This pattern of short-term dual use as an intermediate stepto full switching or quitting appears more common in Sweden than long-term dual use of SLTand cigarettes (Ramström and Foulds, 2006). It is a pattern that could be encouraged by acombination of policies, such as educating smokers about health risks, imposing differentialtax rates on smoked tobacco and SLT products based on their relative harmfulness, andregulating the availability and accessibility of these products to favour SLT.
Ethical issuesDo public health practitioners have the ethical right to prevent smokers from being informedabout THR products in order to reduce the possibility that THR may increase populationnicotine use? Those who argue that smokers should not be told how to reduce their risks promote a paternalistic policy that sacrifices smokers’ interests to the greater public good.Others argue that informing smokers about THR is an effective public health measure thatproperly respects their autonomy (Kozlowski, 2003; Kozlowski and Edwards, 2005;Waterbor et al., 2004).Some opposition to THR reflects the belief that the goal of tobacco control policy should be theelimination of all nicotine use (for example, Pierce, 2002). Some opponents also argue that THRis morally wrong because it involves the long-term use of an addictive substance (Warner et al.,1997). These views contrast with the consequentialist ethical views of proponents who arguethat the benefits of THR outweigh its harms (for example, Kozlowski, 2002).The THR debate is complicated by the role of the tobacco industry whose interests conflictwith those of public health. THR is seen as benefiting the tobacco industry by condoningcontinued tobacco use and thereby allowing the industry’s continued existence (Bullen et al.,2006). Whilst the abolition of the tobacco industry would arguably be preferable, most THRproponents see this as an unrealistic goal, at least in the short to medium term (Hall andGartner, 2009) and accept that enabling the tobacco industry to become part of the solutioncould accelerate change in the nicotine market over time.265
Harm reduction: evidence, impacts and challenges
Options for promoting tobacco harm reductionRegulating the harmfulness of tobacco productsMandating standards for RIP of cigarettes is unlikely to cause harm and may reduce cigarette-related fires. It is much less certain whether mandated maximum levels of key toxins in cigaretteemissions will reduce aggregate harm because of the risk that any gains will be offset bycompensatory smoking, higher levels of other toxins, and/or the impression of a significantreduction in harm. It will in any case take decades to assess. Mandated standards for toxins,such as tobacco-specific nitrosamines, in SLT should be less problematic to implement becausethe feasibility of this strategy has already been demonstrated (Österdahl et al., 2004; Stepanovet al., 2006) and, on Swedish experience, it is likely to minimise oral cancer risk.Information about THR productsHarm reduction could be promoted through advising smokers to use less harmful products,such as LNSLT and PN. This could be done via product warning labels on cigarettes and lessharmful tobacco and nicotine products that indicate the relative harmfulness of each product.This option is currently most relevant for non-EU countries and Sweden because of the salesban on most of these products in EU Member States. Information provided by governmentsand health authorities could also clearly indicate the relative harms of each product, ratherthan misleadingly suggesting that all tobacco products are equally hazardous (Kozlowski,2003; Kozlowski and O’Connor, 2003; Waterbor et al., 2004).Regulation and promotion of THR productsSmokers who fail to quit after obtaining cessation assistance could be encouraged to use PNas a long-term alternative (Kozlowski, 2002; Kozlowski et al., 2003). This is one of the fewTHR strategies supported by the majority of US tobacco control advocates (Warner andMartin, 2003) and advocated by the Royal College of Physicians in the United Kingdom(Royal College of Physicians, 2007) and experts in the EU (ASPECT Consortium, 2004). Itwould probably have limited public health impact if it was aimed solely at high-risk smokerswho failed to quit, because only a minority of these smokers seek help to quit, and probablyfew of whom find existing forms of PN attractive (Stratton et al., 2001; Warner et al., 1997).In order to have a larger public health impact, THR requires as many smokers as possible toswitch to either PN or LNSLT. The Swedish experience suggests that LNSLT may be more likelyto achieve this goal than current forms of PN as more smokers in Sweden have switched toLNSLT than PN (Foulds et al., 2003; Ramström, 2000). This could change if regulators allowedmore attractive forms of PN to be developed and marketed to smokers. In EU countries otherthan Sweden, consideration could be given to relaxing the sales ban on non-smoked, non-chewed oral tobacco products. More equal competition between cigarettes and less hazardousnicotine delivery devices could be achieved by making it harder to introduce new cigarette-liketobacco products and easier to introduce and promote the use of non-smoked THR productsand recreational PN products (Stratton et al., 2001; Warner et al., 1997). Thought should be266
Chapter 9: Harm reduction policies for tobacco
given to the regulation of products that fall between current PN products and cigarettes. Thee-cigarette could provide a test case for developing a more flexible regulatory structure thatworks in favour of public health, by regulating nicotine-containing products according tocriteria that consider the relative harmfulness of each product.
A graduated policy sequenceWe believe that exploring the use of LNSLT for THR is the most promising route facingregulators at the moment. The development of faster-acting PN is likely to take some time ande-cigarettes are probably too similar to PN products. The following steps could be used toexplore the public health potential of THR using LNSLT in those countries in which theirproduction and sale is prohibited, such as the EU, Australia and New Zealand(Commonwealth of Australia, 1974; European Parliament and Council of the European Union,2001; Parliament of New Zealand, 1990).First, the utility of LNSLT for smoking cessation could be cautiously trialled among smokers whohad failed to quit with the use of PN and other smoking cessation medications by encouragingthem to switch to LNSLT rather than return to smoking. Evaluations of this approach wouldprovide information on how attractive these products may be to inveterate smokers.Second, relaxation of PN product regulation could encourage the use of existing PN for long-term substitution if smokers fail to stop, and enable the delivery of nicotine doses in waysmore like SLT, thereby encouraging smokers who failed to quit smoking to use these productsinstead.Third, if there was sufficient interest in switching to LNSLT among inveterate smokers,permitting restricted sale of LNSLT products to these smokers (e.g. from specialist tobacconists)could provide an alternative to continued smoking. Legislation could impose differential taxesto reflect the relative harmfulness.Fourth, the impacts of the sale of these products on: population smoking cessation rates; allforms of tobacco use among youth; and tobacco industry marketing should be rigorouslyevaluated.
ConclusionsPublic smoking bans and mandatory reduced ignition propensity standards for cigarettes arestrategies that reduce tobacco-related harm to non-smokers and should be implemented as apriority. The most promising strategy for reducing harm to tobacco smokers is to encouragesmokers who are unable or unwilling to quit to switch to pharmaceutical nicotine or lownitrosamine smokeless tobacco products. There is good support for this policy fromepidemiological studies in Sweden. Modelling studies indicate that this would verysubstantially reduce the risks of tobacco use. Nonetheless, this remains a controversial policybecause the view of some in the tobacco control community is that our policy goal should be267
Harm reduction: evidence, impacts and challenges
elimination of all nicotine use. A major barrier to its implementation is that many states in theEU ban the sale of these products, and proposals to remove these bans have been opposedbecause of concerns that THR may increase the uptake of tobacco smoking and the harmthat it causes.
ReferencesAlpert, H. R., Carpenter, C., Connolly, G. N., Rees, V. and Wayne, G. F. (2005),‘Fire safer’ cigarettes: the effect ofthe New York State Cigarette Fire Safety Standard on ignition propensity, smoke toxicity, and the consumer market. Apreliminary report,Harvard School of Public Health, Boston. Available at http://www.firesafecigarettes.org/assets/files/harvardstudy.pdf.Arendt, P. (2008), ‘One month of ... electronic cigarettes’,Guardian,8 December, Comment and features, p. 17.Arnott, D. and Berteletti, F. (2008), ‘Europe: agreement on reducing cigarette fires’,Tobacco Control17, pp. 4–5.ASH UK (2008),Beyond Smoking Kills: protecting children, reducing inequalities,Action on Smoking and Health,London. Available at www.ash.org.uk/beyondsmokingkills.ASPECT Consortium (2004),Tobacco or health in the European Union,European Commission, Luxembourg.Available at http://ec.europa.eu/health/ph_determinants/life_style/Tobacco/Documents/tobacco_fr_en.pdf.Ault, R. W., Ekelund, R. B., Jackson, J. D. and Saba, R. P. (2004), ‘Smokeless tobacco, smoking cessation andharm reduction: an economic analysis’,Applied Economics36, pp. 17–29.Benowitz, N. (2008), ‘Clinical pharmacology of nicotine: implications for understanding, preventing, and treatingtobacco addiction’,Clinical Pharmacology & Therapeutics83, pp. 531–41.Benowitz, N. L. (2000), ‘Nicotine toxicity’, in Ferrence, R., Slade, J., Room, R. and Pope, M. (eds),Nicotine andpublic health,American Public Health Association, Washington, DC, pp. 65–76.Berridge, V. (2007),Marketing health: smoking and the discourse of public health in Britain, 1945–2000,OxfordUniversity Press, Oxford.Bertram, M. Y., Lim, S. S., Wallace, A. L. and Vos, T. (2007), ‘Costs and benefits of smoking cessation aids:making a case for public reimbursement of nicotine replacement therapy in Australia’,Tobacco Control16, pp.255–60.Brandt, A. (2007),The cigarette century: the rise, fall, and deadly persistence of the product that defined America,Basic Books, New York.Breland, A. B., Evans, S. E., Buchhalter, A. R. and Eissenberg, T. (2002), ‘Acute effects of AdvanceTM: a potentialreduced exposure product for smokers’,Tobacco Control11, pp. 376–8.Breland, A. B., Kleykamp, B. A. and Eissenberg, T. (2006), ‘Clinical laboratory evaluation of potential reducedexposure products for smokers’,Nicotine & Tobacco Research8, pp. 727–38.Broadstock, M. (2007),Systematic review of the health effects of modified smokeless tobacco products, New ZealandHealth Technology Assessment Report 10/1,Department of Public Health and General Practice, ChristchurchSchool of Medicine and Health Sciences, Christchurch. Available at http://nzhta.chmeds.ac.nz/publications/smokeless_tobacco.pdf.
268
Chapter 9: Harm reduction policies for tobacco
Bullen, C., McRobbie, H., Thornley, S., Walker, N. and Whittaker, R. (2006), ‘Working with what we have beforegetting into bed with the tobacco industry’,New Zealand Medical Journal119, p. U2139.Burns, D. M., Dybing, E., Gray, N., et al. (2008), ‘Mandated lowering of toxicants in cigarette smoke: adescription of the World Health Organization TobReg proposal’,Tobacco Control17, pp. 132–41.Carpenter, M. J., Hughes, J. R., Solomon, L. J. and Callas, P. W. (2004), ‘Both smoking reduction with nicotinereplacement therapy and motivational advice increase future cessation among smokers unmotivated to quit’,Journal of Consulting and Clinical Psychology72, pp. 371–81.Chapman, S. and Balmain, A. (2004),Reduced-ignition propensity cigarettes: a review of policy relevant informationprepared for the Commonwealth Department of Health and Ageing,Commonwealth of Australia, Canberra.Available at http://www.health.gov.au/internet/main/publishing.nsf/Content/health-pubhlth-publicat-document-smoking_rip.htm.Chapman, S. and Freeman, B. (2008), ‘Markers of the denormalisation of smoking and the tobacco industry’,Tobacco Control17, pp. 25–31.Commission of the European Communities (2008),Commission Decision of 25 March 2008 on the fire safetyrequirements to be met by European standards for cigarettes pursuant to Directive 2001/95/EC of the EuropeanParliament and of the Council,Official Journal of the European Union, Office for Official Publications of theEuropean Communities, Luxembourg. Available at http://eur-lex.europa.eu/.Commonwealth of Australia (1974),Trade Practices Act No. 51 of 1974,Attorney General’s Department. Availableat http://www.comlaw.gov.au/.Danish Medicines Agency (2009),Classification of electronic cigarettes, March 9 2009 (medicinal products),Lægemiddelstyrelsen, Copenhagen. Available at http://www.dkma.dk/1024/visUKLSArtikel.asp?artikelID=14819.European Commission Health and Consumer Protection Directorate-General (2008),Orientation note: electroniccigarettes and the EC legislation,European Commission, Brussels. Available at http://ec.europa.eu/health/ph_determinants/life_style/Tobacco/Documents/orientation_0508_en.pdf.European Court of Justice (2004), ‘The Court declares the prohibition on tobacco products for oral use to bevalid’, press release No. 99/04, Judgments of the Court of Justice in Cases C-210/03 and C-434/02, EuropeanCourt of Justice, Luxembourg. Available at http://curia.europa.eu/.European Parliament and Council of the European Union (2001),Directive 2001/37/EC of the European Parliamentand of the Council of 5 June 2001 on the approximation of the laws, regulations and administrative provisions of theMember States concerning the manufacture, presentation and sale of tobacco products,Official Journal of theEuropean Union, Luxembourg. Available at http://eur-lex.europa.eu/.Fagerström, K. O. and Jiménez-Ruiz, C. A. (2008), ‘Pharmacological treatments for tobacco dependence’,European Respiratory Review17, pp. 192–8.Fagerström, K. O., Hughes, J. R., Rasmussen, T. and Callas, P. W. (2000), ‘Randomised trial investigating effectof a novel nicotine delivery device (Eclipse) and a nicotine oral inhaler on smoking behaviour, nicotine andcarbon monoxide exposure, and motivation to quit’,Tobacco Control9, pp. 327–33.Fichtenberg, C. M. and Glantz, S. A. (2002), ‘Effect of smoke-free workplaces on smoking behaviour: systematicreview’,British Medical Journal325, pp. 188–95.Foulds, J., Ramström, L., Burke, M. and Fagerström, K. (2003), ‘Effect of smokeless tobacco (snus) on smoking andpublic health in Sweden’,Tobacco Control12, pp. 349–59.
269
Harm reduction: evidence, impacts and challenges
Furberg, H., Bulik, C. M., Lerman, C., et al. (2005), ‘Is Swedish snus associated with smoking initiation orsmoking cessation?’Tobacco Control14, pp. 422–4.Gartner, C. E., Hall, W. D., Chapman, S. and Freeman, B. (2007a), ‘Should the health community promotesmokeless tobacco (snus) as a harm reduction measure?’,PLoS Medicine4, pp. 1703–04.Gartner, C. E., Hall, W. D., Vos, T., et al. (2007b), ‘Assessment of Swedish snus for tobacco harm reduction: anepidemiological modelling study’,Lancet369, pp. 2010–14.Gartner, C., Barendregt, J. and Hall, W. (2009), ‘Predicting the future prevalence of cigarette smoking inAustralia: how low can we go and by when?’Tobacco Control18, pp. 183–9.Gerlach, K. K., Rohay, J. M., Gitchell, J. G. and Shiffman, S. (2008), ‘Use of nicotine replacement therapy amongnever smokers in the 1999–2006 National Health and Nutrition Examination Surveys’,Drug and AlcoholDependence98, pp. 154–8.Glantz, S. A., Slade, J., Bero, L. A., Hanauer, P. and Barnes, D. E. (eds) (1996),The cigarette papers,University ofCalifornia Press, Berkeley.Gray, N. (2004), ‘The ethics of policies for the prevention of tobacco disease’,Acta Oncologica43, pp. 8–10.Gunja, M., Wayne, G. F., Landman, A., Connelly, G. and McGuire, A. (2002), ‘The case for fire safe cigarettesmade through industry documents’,Tobacco Control11, pp. 346–53.Haddock, C. K., Vander Weg, M., DeBon, M., et al. (2001), ‘Evidence that smokeless tobacco use is a gatewayfor smoking initiation in young adult males’,Preventive Medicine32, pp. 262–7.Hajek, P., McRobbie, H. and Gillison, F. (2007), ‘Dependence potential of nicotine replacement treatments:effects of product type, patient characteristics, and cost to user’,Preventive Medicine44, pp. 230–4.Hall, W. D. and Gartner, C. E. (2009), ‘Supping with the devil? The role of law in promoting tobacco harmreduction using low nitrosamine smokeless tobacco products’,Public Health123, pp. 287–91.Hammond, D., Reid, J. L., Driezen, P., et al. (2008), ‘Smokers’ use of nicotine replacement therapy for reasonsother than stopping smoking: findings from the ITC Four Country Survey’,Addiction103, pp. 1696–703.Hatsukami, D. K., Lemmonds, C., Zhang, Y., et al. (2004), ‘Evaluation of carcinogen exposure in people whoused “reduced exposure” tobacco products’,Journal of the National Cancer Institute96, pp. 844–52.Hatsukami, D. K., Ebbert, J. O., Feuer, R. M., Stepanov, I. and Hecht, S. S. (2007), ‘Changing smokeless tobaccoproducts: new tobacco delivery systems’,American Journal of Preventive Medicine33, pp. S368–S78.Henningfield, J. E. and Fagerström, K. O. (2001), ‘Swedish match company, Swedish snus and public health: aharm reduction experiment in progress?’,Tobacco Control10, pp. 253–7.Hoffmann, D., Djordjevic, M. V., Fan, J., et al. (1995), ‘Five leading U.S. commercial brands of moist snuff in1994: assessment of carcinogenic N-nitrosamines’,Journal of the National Cancer Institute87, pp. 1862–9.Hopkins, D. P., Briss, P. A., Ricard, C. J., et al. (2001), ‘Reviews of evidence regarding interventions to reducetobacco use and exposure to environmental tobacco smoke’,American Journal of Preventive Medicine20, pp.16–66.Joossens, L. and Raw, M. (2007),Progress in tobacco control in 30 European countries, 2005 to 2007,SwissCancer League, Berne. Available at http://www.ensp.org/files/30_european_countries_text_final.pdf.Kemm, J. (2003), ‘A model to predict the results of changes in smoking behaviour on smoking prevalence’,Journal of Public Health Medicine25, pp. 318–24.
270
Chapter 9: Harm reduction policies for tobacco
King, B., Borland, R. and Fowles, J. (2007), ‘Mainstream smoke emissions of Australian and Canadian cigarettes’,Nicotine & Tobacco Research9, pp. 835–44.Klesges, L. M., Johnson, K. C., Somes, G., Zbikowski, S. and Robinson, L. (2003), ‘Use of nicotine replacementtherapy in adolescent smokers and nonsmokers’,Archives of Pediatrics and Adolescent Medicine157, pp. 517–22.Kozlowski, L. T. (2002), ‘Harm reduction, public health, and human rights: smokers have a right to be informed ofsignificant harm reduction options’,Nicotine & Tobacco Research4, pp. S55–S60.Kozlowski, L. T. (2003), ‘First, tell the truth: a dialogue on human rights, deception, and the use of smokelesstobacco as a substitute for cigarettes’,Tobacco Control12, pp. 34–6.Kozlowski, L. T. and Edwards, B. Q. (2005), ‘“Not safe” is not enough: smokers have a right to know more thanthere is no safe tobacco product’,Tobacco Control14, pp. II3–II7.Kozlowski, L. T. and O’Connor, R. J. (2003), ‘Apply federal research rules on deception to misleading healthinformation: an example on smokeless tobacco and cigarettes’,Public Health Reports118, pp. 187–92.Kozlowski, L. T., Strasser, A. A., Giovino, G. A., Erickson, P. A. and Terza, J. V. (2001), ‘Applying the risk/useequilibrium: use medicinal nicotine now for harm reduction’,Tobacco Control10, pp. 201–03.Kozlowski, L. T., O’Connor, R. J. and Quinio Edwards, B. (2003), ‘Some practical points on harm reduction: whatto tell your lawmaker and what to tell your brother about Swedish snus’,Tobacco Control12, pp. 372–3.Laugesen, M. (2008),Second safety report on the Ruyan� e-cigarette,Health New Zealand Ltd, Christchurch.Available at http://www.healthnz.co.nz/2ndSafetyReport_9Apr08.pdf.Laugesen, M., Thornley, S., McRobbie, H. and Bullen, C. (2008),How safe is an e-cigarette? The results ofindependent chemical and microbiological analysis(poster), SRNT 14th Annual Meeting, Society for Research onNicotine and Tobacco, Portland, Oregon.Le Houezec, J. and Sawe, U. (2003), ‘Smoking reduction and temporary abstinence: new approaches forsmoking cessation’,Journal des Maladies Vasculaires28, pp. 293–300.Levy, D. T., Mumford, E. A., Cummings, K. M., et al. (2004), ‘The relative risks of a low-nitrosamine smokelesstobacco product compared with smoking cigarettes: estimates of a panel of experts’,Cancer Epidemiology,Biomarkers and Prevention13, pp. 2035–42.Levy, D. E., Thorndike, A. N., Biener, L. and Rigotti, N. A. (2007), ‘Use of nicotine replacement therapy to reduceor delay smoking but not to quit: prevalence and association with subsequent cessation efforts’,Tobacco Control16, pp. 384–9.Medioni, J., Berlin, I. and Mallet, A. (2005), ‘Increased risk of relapse after stopping nicotine replacementtherapies: a mathematical modelling approach’,Addiction100,pp. 247–54.Mendez, D., Warner, K. E. and Courant, P. N. (1998), ‘Has smoking cessation ceased? Expected trends in theprevalence of smoking in the United States’,American Journal of Epidemiology148, pp. 249–58.Murray, R. P., Bailey, W. C., Daniels, K., et al. (1996), ‘Safety of nicotine polacrilex gum used by 3,094participants in the Lung Health Study. Lung Health Study Research Group’,Chest109, pp. 438–45.National Drugs and Poisons Scheduling Committee (2009),Standard for the uniform scheduling of drugs andpoisons (SUSDP) No. 23,Department of Health and Ageing, Commonwealth of Australia, Canberra. Available athttp://www.comlaw.gov.au/.
271
Harm reduction: evidence, impacts and challenges
New Zealand Public Health Directorate (2006), ‘Classification of medicines notice, schedule 3, pharmacy-onlymedicines: nicotine’,New Zealand Gazette,NZ Department of Internal Affairs, Wellington, p. 188.Nides, M. (2008), ‘Update on pharmacologic options for smoking cessation treatment’,American Journal ofMedicine121, pp. S20–S31.O’Connor, R. J., Kozlowski, L. T., Flaherty, B. P. and Edwards, B. Q. (2005), ‘Most smokeless tobacco use doesnot cause cigarette smoking: results from the 2000 National Household Survey on Drug Abuse’,AddictiveBehaviors30, pp. 325–36.Österdahl, B. G., Jansson, C. and Paccou, A. (2004), ‘Decreased levels of tobacco-specific N-nitrosamines inmoist snuff on the Swedish market’,Journal of Agricultural and Food Chemistry52, pp. 5085–8.Pankow, J. F., Watanabe, K. H., Toccalino PL, Luo, W. and Austin, D. F. (2007), ‘Calcuated cancer risk forconventional and “potentially reduced exposure product” cigarettes’,Cancer Epidemiology, Biomarkers andPrevention16, pp. 584–92.Parliament of New Zealand (1990),Smoke-free environments act no. 108.Available at http://www.legislation.govt.nz/act/public/1990/0108/latest/DLM223191.html?search=ts_act_smoke-free+environments&;sr=1.Pell, J. P., Haw, S., Cobbe, S., et al. (2008), ‘Smoke-free legislation and hospitalizations for acute coronarysyndrome’,New England Journal of Medicine359, pp. 482–91.Pierce, J. P. (2002), ‘Harm reduction or harm maintenance?’,Nicotine and Tobacco Research4, pp. S53–S4.Ramström, L. (2003), ‘Snus: part of the problem or part of the solution?’,Addiction98, pp. 1198–9.Ramström, L. M. (2000), ‘Snuff: an alternative nicotine delivery system’, in Ferrence, R., Slade, J., Room, R. andPope, M. (eds),Nicotine and public health,American Public Health Association, Washington, DC.Ramström, L. M. and Foulds, J. (2006), ‘Role of snus in initiation and cessation of tobacco smoking in Sweden’,Tobacco Control15, pp. 210–4.Rees, V. W., Wayne, G. F. and Connolly, G. N. (2008), ‘Puffing style and human exposure minimally altered byswitching to a carbon-filtered cigarette’,Cancer Epidemiology Biomarkers & Prevention17, p. 2995.Royal College of Physicians (2007),Harm reduction in nicotine addiction: helping people who can’t quit. A report bythe Tobacco Advisory Group of the Royal College of Physicians,RCP, London. Available at http://www.rcplondon.ac.uk/.SCENIHR (2008),Health effects of smokeless tobacco products,Scientific Committee on Emerging and NewlyIdentified Health Risks, European Commission, Brussels. Available at http://ec.europa.eu/health/ph_risk/committees/04_scenihr/docs/scenihr_o_013.pdf.Shiffman, S., Gitchell, J. G., Warner, K. E., et al. (2002a), ‘Tobacco harm reduction: conceptual structure andnomenclature for analysis and research’,Nicotine & Tobacco Research4, pp. S113–S129.Shiffman, S., Rolf, C. N., Hellebusch, S. J., et al. (2002b), ‘Real world efficacy of prescription and over-the-counter nicotine replacement therapy’,Addiction97, pp. 505–16.Sikora, K. (2007), ‘Electric cigarette beats pub smoking ban’,Daily Telegraph15 November. Available at http://www.news.com.au/story/0,23599,22762416-13762,00.html.Stead, L. F., Perera, R., Bullen, C., Mant, D. and Lancaster, T. (2008), ‘Nicotine replacement therapy for smokingcessation’,Cochrane Database of Systematic Reviews,CD000146.Stepanov, I., Jensen, J., Hatsukami, D. and Hecht, S. S. (2006), ‘Tobacco-specific nitrosamines in new tobaccoproducts’,Nicotine & Tobacco Research8, pp. 309–13.
272
Chapter 9: Harm reduction policies for tobacco
Stratton, K., Shetty, P., Wallace, R. and Bondurant, S. (eds) (2001),Clearing the smoke: assessing the science basefor tobacco harm reduction,National Academy Press, Washington, DC.Timberlake, D. S., Huh, J. and Lakon, C. M. (2009), ‘Use of propensity score matching in evaluating smokelesstobacco as a gateway to smoking’,Nicotine and Tobacco Research11, pp. 455–62.Toumbourou, J. W., Stockwell, T., Neighbors, C., et al. (2007), ‘Adolescent health 4: interventions to reduce harmassociated with adolescent substance use’,Lancet369, pp. 1391–401.US Department of Health and Human Services (2006),The health consequences of involuntary exposure to tobaccosmoke: a report of the Surgeon General,U.S. Department of Health and Human Services, Centers for DiseaseControl and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office onSmoking and Health, Atlanta, GA. Available at http://www.surgeongeneral.gov/library/secondhandsmoke/.Warner, K. E. (2001), ‘Reducing harm to smokers: methods, their effectiveness and the role of policy’, in Rabin, R.L. and Sugarman, S. D. (eds),Regulating tobacco,Oxford University Press, Oxford, pp. 111–42.Warner, K. E. and Martin, E. G. (2003), ‘The US tobacco control community’s view of the future of tobacco harmreduction’,Tobacco Control12, pp. 383–90.Warner, K. E., Slade, J. and Sweanor, D. T. (1997), ‘The emerging market for long-term nicotine maintenance’,JAMA278, pp. 1087–92.Waterbor, J. W., Adams, R. M., Robinson, J. M., Crabtree, F. G., Accortt, N. A. and Gilliland, M. J. (2004),‘Disparities between public health educational materials and the scientific evidence that smokeless tobacco usecauses cancer’,Journal of Cancer Education19, pp. 17–28.WHO Regional Office for Europe (2003),WHO European country profiles on tobacco control,World HealthOrganization, Copenhagen. Available at http://www.euro.who.int/tobaccofree/publications/publications.WHO Regional Office for Europe (2007),The European tobacco control report 2007,World Health Organization,Copenhagen. Available at http://www.euro.who.int/tobaccofree/publications/publications.World Bank (2003),Tobacco control at a glance,World Bank Group, Washington, DC. Available at http://go.worldbank.org/3HHPVQI020.
273
Chapter 10Alcohol harm reduction in EuropeRachel Herring, Betsy Thom, Franca Beccaria, Torsten Kolind and Jacek Moskalewicz
AbstractThis chapter provides an overview of harm reduction approaches to alcohol in Europe. First,definitions ascribed to alcohol harm reduction are outlined. Then, evaluated alcohol harmreduction interventions in European countries are described and the evidence for theireffectiveness examined. These include multi-component programmes, improvements to thedrinking environment, and initiatives to reduce the harms associated with drink-driving. Third,harm reduction activities that have been recorded and described but not yet evaluated are brieflyoutlined. These include ‘grassroots’ initiatives and more formal local initiatives. To conclude, thechapter raises questions about how alcohol harm reduction is defined and put into practice, theevidence-base that is available for policymakers, and how information is shared. It highlights theneed to develop systems to facilitate knowledge transfer on alcohol harm reduction betweenresearchers, policymakers and practitioners in Europe but stresses the importance of respectinglocal and cultural diversity in the development and implementation of harm reduction initiatives.Keywords:alcohol, harm reduction, Europe, evaluation.
IntroductionThe consumption of alcohol is an integral part of many European cultures and is embedded ina variety of social practices. Whilst drinking alcohol is, for the most part, a pleasurableexperience often associated with relaxation and celebrations, there are a number of societaland health harms associated with its consumption. The European Union (EU) is the heaviestdrinking region of the world (Anderson and Baumberg, 2006) and alcohol is linked to multiplehealth and social problems. Health-related conditions include cancer, injury, liver cirrhosis andcardiovascular disease; it is estimated that in the EU alcohol is responsible for 7.4 % of alldisability and premature deaths (Anderson and Baumberg, 2006, p. 401). At a global level, itis estimated that 3.8 % of all deaths and 4.6 % of disability-adjusted life years are attributableto alcohol (Rehm et al., 2009, p. 2223). There is also a broad range of societal harmsassociated with alcohol consumption including crimes, violence, unemployment andabsenteeism, which place a significant burden on societies and economies (WHO, 2008a)A wide array of measures are employed by European countries to reduce the harmsassociated with alcohol. These include restrictions on availability, taxation, educationcampaigns, laws on drink-driving, and a range of formal and informal interventionscommonly referred to as ‘harm reduction’ or ‘risk reduction’ measures. Yet the concept ofharm reduction is contested — as is the usefulness of this approach — and there is very littlerigorous evaluation of harm reduction projects or programmes, including in Europe.275
Harm reduction: evidence, impacts and challenges
This chapter begins with a brief overview of alcohol consumption and alcohol-related harms inEurope. This will be followed by an examination of what is meant by the term ‘harm reduction’in relation to alcohol. It then considers harm reduction interventions that have been evaluatedin European countries, also drawing upon the broader published literature, much of which isNorth American or Australasian. We briefly outline harm reduction activities that have beenrecorded and described but not yet evaluated. These include ‘grass roots’ initiatives and moreformal local initiatives. In conclusion, we argue for a clarification of what is meant by the term‘alcohol harm reduction’, and the creation of more effective systems for sharing information andcollecting data, alongside research to examine the extent to which harm reduction is seen as anappropriate approach to reducing alcohol-related harms in the different countries of Europe.
Alcohol-related harm in EuropeThe relationship between alcohol consumption and health and social outcomes is complex andmultidimensional. Key factors include: volume of alcohol drunk over time; pattern of drinking (forexample, occasional or regular drinking to intoxication); and drinking context (e.g. place,companions, occasion) (WHO, 2008a). The countries with the highest overall alcoholconsumption in the world are in eastern Europe, around Russia, but other areas of Europe alsohave high overall consumption (WHO Europe region 11.9 litres per adult; Rehm et al., 2009, p.2228). In all regions worldwide, including Europe, men consume more alcohol than women, andare more likely to die of alcohol-attributable causes, suffer from alcohol-attributable diseasesand alcohol-use disorders (Rehm et al., 2009; Anderson and Baumberg, 2006). Europe has thehighest proportion of alcohol-attributable net deaths and within Europe the highest proportion isfor the countries of the former Soviet Union (Rehm et al., 2009, p. 2229). Alcohol is thought tobe responsible for 12 % of male and 2 % of female deaths in Europe (Anderson and Baumberg2006, p. 3), and 25 % of male youth mortality and 10 % of female youth mortality (Andersonand Baumberg 2006). The health impact of alcohol is seen over a wide range of conditions (seeTable 10.1 for examples) and includes acute harms (e.g. accidents and injuries as a result ofintoxication) and harms associated with longer-term consumption (e.g. cirrhosis).
Table 10.1:The impact of alcohol on health in EuropeHarmRoad traffic accidentsHomicidesAccidental deathsSuicideCancerLiver cirrhosisNeuropsychiatric conditionsDepressionAlcohol dependence
Impact17 000 deaths per year (1 in 3 of all road traffic fatalities)2 000 (4 in 10 of all murders and manslaughters)27 000 deaths10 000 deaths (1 in 6 of all suicides)50 000 deaths45 000 deaths17 000 deaths200 000 episodes23 million people in any one year (5 % men and 1 % women)
Source:Compiled from data in Anderson and Baumberg 2006, pp. 3 and 6).
276
Chapter 10: Alcohol harm reduction in Europe
Alcohol consumption can negatively impact on an individual’s work, their relationships andstudies (e.g. absenteeism, breakdown of relationships) and consequently on other people (e.g.families, colleagues) and society as a whole. At a societal level the harms associated with theconsumption of alcohol include public nuisance (e.g. disturbance, fouling of the streets),public disorder (e.g. fights), drink-driving and criminal damage. The tangible costs of alcoholto the EU (that is, to the criminal justice system, health services, economic system) wereestimated to be EUR 125 bn in 2003; this included EUR 59 bn in lost productivity due toabsenteeism, unemployment and lost working years through premature death (Anderson andBaumberg, 2006, p. 11); the intangible costs of alcohol (which describe the value peopleplace on suffering and lost life) to the EU were estimated to be EUR 270 bn in 2003(Anderson and Baumberg, 2006, p. 11).
What is alcohol harm reduction?Although in recent times the term ‘harm reduction’ has mostly been associated with the illicitdrug field, alcohol harm reduction strategies have been used for centuries (Wodak, 2003;Nicholls, 2009). For instance, in England, the idea that those serving alcoholic beveragesshould be legally responsible for preventing customers from getting drunk can be tracedback to James I’s 1604 ‘Act to restrain the inordinate haunting and tipling of inns, alehousesand other victualling houses’; in practice the law was largely ignored, but it did establish animportant principle (Nicholls, 2009, p. 11). Examples of similar formal and informalconstraints on behaviour can be found in other European countries and, indeed, worldwide.In sixteenth century Poland an innkeeper was supposed to make sure that farmers had nodangerous objects with them in a pub, as they often became violent after drinking and thenwould try to use drunkenness as an excuse for their behaviour (Bystoń, 1960). Thus, thosewho served alcohol combined their profit-oriented job with harm reduction. Women haveoften served as social control or harm reduction agents; in Patagonia, Indian Tehuelcheyoung women, not yet of drinking age, collected all weapons, including knives and axes,prior to a drinking party to prevent severe injures in a case of alcohol-induced violence(Prochard, 1902).Measures to ensure the safety of alcoholic beverages (that is, free from harmfuladulteration or contamination, regulation of the alcohol content of drinks) are also long-standing and remain important. Austrian wine adulterated with diethylene glycol (found inantifreeze) to make it taste sweeter was withdrawn from sale across the world in the mid-1980s (Tagliabue, 1985). Regulation of the sale and size of containers of medicinal (pure)alcohol has reduced the harms associated with its consumption in Nordic countries(Lachenmeier et al., 2007). Research in Estonia (Lang et al., 2006) examining thecomposition of illegally produced (such as home-produced) and surrogate alcohol products(e.g. aftershave, fire lighting fuel) found high levels of alcohol by volume (up to 78.5 %) andvarious toxic substances (e.g. long chain alcohols). Moreover, it is likely that theconsumption of surrogate alcohol and illegally produced alcohol contributes to the highmortality and morbidity associated with alcohol consumption in other countries in transition(see, for example, McKee et al., 2005; Leon et al., 2007 on Russia).277
Harm reduction: evidence, impacts and challenges
Harm reduction principles were central to the influential ‘Gothenburg System’, named afterthe Swedish city that first adopted the approach in 1865 (Pratt, 1907). Under Swedish lawprivate companies could be established that were empowered to buy up the sprits trade inspecific localities and run it on a not-for-profit basis, thus removing the financial incentive tosell large quantities of spirits. Managers whose salaries were not dependent on high sales ofspirits (the law did not cover sales of beer or food) were employed to run the pubs. Althoughthe effectiveness of the Gothenburg System in reducing excessive consumption was notentirely clear (Nicholls, 2009), it was an idea that attracted much interest and was adoptedin other places, including Bergen, Norway. The Gothenburg system also inspired the systemof ‘disinterested management’, established in late nineteenth century England, wherebycompanies were formed that bought up pubs and employed salaried managers;shareholders, in return for their investment, received a capped dividend on their investment.However, the impact of this scheme was limited by the small number of establishments run onthese lines (Nicholls, 2009).Whilst not a new idea, harm reduction was not particularly formulated as a concept forpolicy intervention until it came to prominence in the illicit drugs field in response to HIV/AIDSin conjunction with the spread of HIV through sexual intercourse and drug injecting(Stronach, 2003). There was a recognition that sexual abstinence and stopping injectingdrugs was not a feasible option for many people, so realistic and pragmatic strategies wererequired that focused on managing the outcomes of behaviour rather than eliminating orchanging the behaviour (Stronach, 2003). As Stockwell (2006) notes, what made harmreduction distinctive when it emerged in the drugs field was the practice of encouraging saferbehaviour (e.g. not sharing injecting equipment and using condoms for sex) withoutnecessarily reducing the occurrence of the behaviour (see, for example, Lenton and Single,1998 and box below).
World Health Organization definition of harm reductionIn the context of alcohol or other drugs, describes policies or programmes that focus directly onreducing the harm resulting from the use of alcohol or drugs. The term is used particularly ofpolicies or programmes that aim to reduce the harm without necessarily affecting the underlyingdrug use; examples includes needle/syringe exchanges to counteract needle-sharing amongheroin users, and self-inflating airbags in automobiles to reduce injury in accidents, especially asa result of drinking-driving. Harm reduction strategies thus cover a wider range than the dichotomyof supply reduction and demand reduction.(WHO, 1994)
With respect to alcohol, Robson and Marlatt (2006) have argued that the World HealthOrganization (WHO) has emphasised total population measures, such as restricting supply,almost to the point of discounting other approaches. However, the WHO are in the processof drafting a global strategy to reduce the harmful use of alcohol (to be considered by theWorld Health Assembly in May 2010) and harm reduction has been identified as one of ninepossible strategy and policy element options (WHO, 2008a). At the same time, whilst278
Chapter 10: Alcohol harm reduction in Europe
acknowledging the positive contribution of harm reduction measures, the WHO note that theevidence base is not, as yet, as well established as that for regulating the availability anddemand for alcohol (WHO, 2008a).However, since the 1990s harm reduction has become increasing influential in the alcoholfield; indeed Robson and Marlatt (2006, p. 255) contend that ‘it is now, up to a point, theconventional wisdom’. So what is alcohol harm reduction? As is common with such terms it will depend on whom you ask or where you look. Stockwell (2006) has shown that the termis applied in many different ways, some of which rather push the boundaries of ‘harmreduction’. For Stockwell, what distinguishes harm reduction from other approaches is that itdoes not require a reduction in use for effectiveness, rather it is about seeking to ‘make theworld safer for drunks’ (2004, p. 51). On their website the International Harm ReductionAssociation (IHRA) state, ‘Alcohol harm reduction can be broadly defined as measures thataim to reduce the negative consequences of drinking’ (IHRA, n.d.), whilst Robson and Marlatt(2006, p. 255) suggest that the common feature of harm reduction interventions is that theydo not aim at abstinence.These broader definitions encompass interventions that do not attempt to reduceconsumption, such as the provision of safety (shatterproof) glassware in drinking venues,‘wet’ shelters, ‘sobering up’ stations, and which often focus on specific risk behaviours (e.g.drink-driving), particular risk groups (e.g. young people) and particular drinking contexts (e.g.clubs, bars). They also encompass interventions that implicitly or explicitly do aim to reducealcohol consumption, for example server training, brief interventions and controlled drinking.But the labelling of approaches that aim to reduce alcohol use as ‘harm reduction’ has beenchallenged, with Stockwell (2004, 2006) arguing that such interventions would be betterdescribed as ‘risk reduction’ as they require the reduction of alcohol intake to less risky levels.Furthermore, a recent round-table discussion involving health professionals and non-governmental organisations about harmful alcohol use, concluded that: ‘Brief interventionsare not considered to constitute a harm reduction approach because they are intended tohelp people drink less’ (WHO, 2008b, p. 8).Stronach (2003, p. 31) identified five key elements that should underpin alcohol harm policiesand interventions:• arm reduction is a complementary strategy that sits beside supply control and demand Hreduction.• ts key focus is on outcomes rather than actual behaviours per se.I• t is realistic and recognises that alcohol will continue to be used extensively in many Icommunities, and will continue to create problems for some individuals and somecommunities.• arm reduction is non-judgemental about the use of alcohol, but is focused on reducing Hthe problems that arise.• t is pragmatic — it does not seek to pursue policies or strategies that are unachievable or Ilikely to create more harm than good.279
Harm reduction: evidence, impacts and challenges
Thus, within policy and research discourse, the notion of ‘alcohol harm reduction’, althoughinfluential, has not gone unchallenged or without controversy. Indeed, there has been atendency, particularly within the media, to dismiss or even ridicule harm reductionapproaches. Within the United Kingdom, recent harm reduction interventions, includinghanding out ‘flip-flops’ to women drinkers to prevent injuries caused by falling over in highheels or walking barefooted, have attracted negative headlines (Hope, 2008; Salked,2008).This lack of consensus can be reflected in the responses of service and policy providersacross Europe. To capture how harm reduction is understood and how related strategies areimplemented in practice in Europe, we conducted a brief survey of the 30 EuropeanMonitoring Centre for Drugs and Drug Addiction (EMCDDA) Heads of Focal Groups. Wereceived responses from Austria, Belgium, Croatia, the Czech Republic, Cyprus, Estonia,Finland, Latvia, Netherlands, Norway, Portugal, Slovakia, Spain and Sweden.We asked our survey informants what they understood by the term ‘harm reduction’. Thedefinitions they gave were anchored around the concept of limiting or reducing the negativehealth, social and economic consequences of alcohol consumption on both individuals andcommunities. A key idea was that harm reduction approaches do not seek to convinceindividuals to abstain or to introduce prohibition but rather take a ‘pragmatic’ approach toreducing harms associated with drinking.Distinctions were made between harm reduction initiatives, which aimed to minimiseharm once it has actually been caused, and risk reduction initiatives, which aimed toprevent harm being caused. Several respondents placed qualifiers; for example, therespondent from Norway did not classify ‘responsible host’ or educational campaigns asharm reduction measures. Similarly the Swedish respondent classified as ‘harmreduction’ only those measures that aimed to reduce harm that already exists to someextent.Such variations were not unexpected but do highlight the fact that, whilst there might be ashared language, the meaning attributed to the term ‘harm reduction’ can differ from oneEuropean country to another. While the meaning of harm reduction varies by country, it isimportant that the measures used are based on evidence and focused on outcomes (WHO,2008b, p. 14). Evidence, however, is scanty.
Reducing alcohol-related problems: the international evidenceAccording to findings from international research, the most effective interventions includealcohol taxes, restrictions on the availability of alcohol and measures to reduce drink-driving; interventions identified as the least effective include alcohol education, publicawareness programmes and designated driver schemes and many of the ‘harmreduction’ approaches (Babor et al., 2003; Anderson, et al., 2009). Stockwell (2004, p.49) argues that the most effective interventions to prevent alcohol-related harm require280
Chapter 10: Alcohol harm reduction in Europe
reduction in the amount of alcohol consumed on a single occasion but suggests thatother measures can be employed alongside measures to reduce total populationconsumption.There is some international evidence about ‘what works’ to reduce alcohol-related harm asdefined in this chapter. The impact of screening and brief intervention (sometimes referred toas ‘identification and brief advice’), particularly in primary care settings, in reducing harmfulalcohol consumption has been extensively evidenced as effective (Babor et al., 2003; Kaneret al., 2007), although, as mentioned earlier, the inclusion of brief interventions as a harmreduction measure is contested.Graham and Homel (2008, pp. 196–238) provide a useful overview of the problems ofreducing alcohol-related aggression in and around pubs and clubs and review theevidence for prevention and harm reduction measures. As they report, only a small numberof interventions have been evaluated with sufficient rigour to draw conclusions. Theymention a large randomised controlled trial of the Safer Bars Programme (a ‘stand-alone’programme in Ontario, Canada), which consists of a risk assessment component, a trainingcomponent and a pamphlet outlining legal responsibilities, as having a modest butstatistically significant effect on incidents of aggression. Police enforcement trials did notprovide sufficient evidence to make recommendations but the Alcohol Linking Programme(Australia) indicated the success of using place of last drinks data as the basis for targetedenforcement. Community action models to implement local policy depend heavily onpartnerships but have demonstrated some success. This approach, evaluated largely inNorth America, Australia, New Zealand and Scandinavia, has been described as ‘anyestablished process, priority, or structure that purposefully alters local social, economic orphysical environments to reduce alcohol problems’ (Holder 2004, p. 101); it is discussedmore fully below.In a comprehensive synthesis and assessment of the international evidence, Babor et al.(2003) offer a menu of interventions, which they have rated on four major criteria:evidence of effectiveness, breadth of research support, extent of testing across diversecountries and cultures, relative cost of the intervention in terms of time, resources andmoney. The assessment reflects a consensus view of the 15 expert authors. For illustration,Table 10.2 (adapted from Babor et al., 2003) shows ratings for two of the criteria:interventions that were rated on effectiveness from none (zero) to highest (three ), andinterventions rated on breadth of research support from none (zero) to highest (three). Thetable tells us, for example, that alcohol education in schools has five or more studies ofeffectiveness but that there is no good evidence of effectiveness. It clearly indicates thattypical harm reduction measures such as warning labels on alcohol, designated driverschemes and voluntary codes of practice are judged as least effective, although, asillustrated in the second column, many harm reduction measures have few well-designedevaluation studies. However, increasing attention has been given to the potential ofprogrammes of projects rather than stand-alone initiatives to achieve change. These ‘multi-component’ programmes, which include many of the harm reduction interventions rated asleast successful, are discussed in the following sections.281
Harm reduction: evidence, impacts and challenges
Table 10.2:What works in reducing alcohol problems?Strategy or interventionAlcohol taxesMinimum legal purchase ageGovernment monopoly of retail salesHours and days of sale restrictionsRestrictions on density of outletsRandom breath testingLowered limits of blood alcohol concentration (BAC)Low BAC for young driversBrief intervention for hazardous drinkersDesignated drivers and ride servicesAdvertising bansVoluntary controls of advertising by alcohol industryAlcohol education in schoolsAlcohol education in collegesAlcohol education targeting general publicWarning labelsVoluntary codes of bar practiceNotes:(1) 0 = lack of effectiveness, + = evidence for limited effectiveness, ++ = evidence for moderate effectiveness, +++ =evidence for high effectiveness.(2) 0 = no well-designed study of effectiveness, + = only one study completed, ++ = from two to four studies completed,+++ = five or more studies completed.Source:Adapted from Babor, T. F., et al. (2003, Table 16.1, pp. 264–6).
Effectiveness (1) Researchsupport (2)++++++++++++++++++++++++0+000000++++++++++++++++++++++++++++++++++++
Harm reduction approaches to alcohol in Europe: evaluated initiativesAlthough the focus of this section is on harm reduction initiatives that have been evaluated ina European context, we also draw on the broader literature. Table 10.3 provides a summaryof the evaluated alcohol harm reduction interventions we have identified either from theEuropean literature or from international sources. Many evaluated harm reductioninterventions are part of multi-component community programmes designed to prevent andreduce alcohol-related harm, whilst others are ‘stand alone’ interventions delivered at thelocal or national level. First, the multi-component approach will be outlined, followed by anexamination of harm reduction interventions under two broad themes: improving the drinkingenvironment and reducing the harms associated with drink-driving. Interventions that formpart of multi-component programmes are summarised in the box on p. 288 and some will beconsidered in more detail under the relevant theme. Although brief interventions are oftenregarded as harm reduction, this chapter will not consider brief interventions, in part becausesuch classification has been contested (as noted above) and because an extensive literaturealready exists and has been reviewed elsewhere (Nilsen et al., 2008).282
Table 10.3:Examples of evaluations of alcohol harm reduction initiatives in Europe: summariesGoal, intervention and outcome measuresReduce over-serving and serving to minors.Reduce problems related to alcohol consumptionin licensed premises, including violence.RBS, enforcement, partnership working.Test purchases. Police reported incidents ofviolence between 10pm–6am. Pre and postintervention measures, control area.Calculate cost-effectiveness of ‘restaurantintervention’ from a societal perspective.Survey of victims of violence, costs, savings,quality adjusted life years (QALYS)Reduce over-serving of alcohol to intoxicatedindividuals and sale of medium strength beer tothose aged under 18.RBS, enforcement, partnership working.Six trial and six control municipalities.Decrease under-age drinking, reduce heavydrinking occasion and related acute problems,develop a model for sustainable preventionstructure at local level. RBS, enforcement,partnership working, public discussion.Two test communities and two control. Pre- andpost-intervention measures
Name of project
Start date
Country
Main findingsStatistically significant reduction in over-servingand serving to minors in both project and controlarea. Possible ‘spill-over’ effects from changes inalcohol policy in both areas.(Wallin et al., 2003a)29 % reduction in police-reported violence(Wallin et al., 2003b)39 times higher savings than cost but caution needsto be exercised because of low response rate(35 %).(Månsdotter et al., 2007)No reduction in serving to intoxicated patrons intrial or controls.Harder for youths to be served in control areas butdifferences not significant.(SNIPH, 2008)Outline of research and discussion of methods.(Holmila and Warpenius, 2007)
‘Restaurant1998intervention’— responsiblebeverage service(RBS), StockholmPrevents Alcohol andDrug Problems (STAD)
Sweden
‘Restaurantintervention’ — RBS,STAD
1998
Sweden
Alcohol and drugprevention in sixmunicipalities
2003
Sweden
Local Alcohol PolicyProject (PAKKA)
2004–08
Finland
Chapter 10: Alcohol harm reduction in Europe
283
Harm reduction: evidence, impacts and challenges
284
Table 10.3(continued)Goal, intervention and outcome measuresReduce alcohol-related violence, over-serving andserving to minors.RBS.Pre- and post-intervention measures.Low participation in RBS training (12 % of licensedpremises) — intervention thus not fully exploited.No impact: no changes in police-reported violencein/around licensed premises, underage sales,over-serving or attitudes/perceptions of staff.(Baklien and Buvik, 2006)Consumption declined in men but not women.Alcohol-related problems showed a statisticallysignificant reduction for men, and a decline forbinge drinkers, but no reduction among women.High awareness (67 %) of project.(Hanson et al., 2000)DWI: Only 11 % of eligible DWI offendersparticipated. 60 % alcohol dependent/abusers.Reduced alcohol consumption during programme(Bjerre, 2005). Post-treatment (when compared to fiveyear period prior to treatment) recidivism 60 % lowerand police-recorded accidents 80 % lower.Control – accident reduction similar but not DWIrecidivism (Bjerre and Thorsson, 2008).Commercial: Among 600 heavy vehicles, 0.19 % of allstarts prevented as BAC >0.02 % (20 mg/dl), mostlyat weekends or mornings.(Bjerre and Kostela, 2008)
Name of project
Start date
Country
Main findings
Responsible HostsProgramme:Trondheim
2000
Norway
Kirseberg project
1988
Sweden
Reduce alcohol consumption in the populationand decrease the incidence of alcohol-relatedproblems. Consumption measures, problemmeasures, survey of exposure to project.
Alcohol-interlockprogramme
1999
Sweden
To prevent drink-driving. Two programmes:driving while intoxicated (DWI) offenders (insteadof licence revocation); and commercial drivers(buses/taxis/trucks).DWI: two-year programme, biomarkers/AUDIT.Control groups. Post-intervention measures.Commercial: Primary prevention. Blood alcoholconcentration (BAC) tests.
Table 10.3(continued)Goal, intervention and outcome measuresReduce alcohol-related injury, violence anddisorder in the city centre.RBS, ‘Best Bar None’ (BBN), test purchasing.‘Nite Zone’: transport/community safetyimprovements (e.g. relocation of bus stops, taxiwardens, extra CCTV with loudspeakers).Awareness raising (conference, radio campaignsand website, police custody cards).
Name of project
Start date
Country
Main findingsDecrease (–9.7 %) in police-recorded crimes anddecrease (–4.4 %) in ambulance incidents. Increase(+74.4 %) in police-recorded alcohol-relatedincidents, increase (+6.5 % in emergencydepartment attendances.Nite Zone: decrease in road accidents (–11.4 %),violent crime (–19 %), serious assault (–4.4 %),robbery (–21.5 %).Awareness: >100 000 websites hits, >2 000 calls toradio station, 2 889 information packs supplied, 17treatment referrals from 400 cards.(Mistral et al., 2007)Decrease (–25.7 %) in emergency departmentattendances, but increase (+33 %) in police-recorded crimes/incidents.= 9 % of city centre staff successfully trained.30 % of premises failed test purchasing.Audits — minority heavily intoxicated, trainingtargeted to problem premises, details of public litter.(Mistral et al., 2007)
Reducing alcohol-2004related injury,violence and disorderin Glasgow city centre
Scotland
Multi-agency,community-basedintervention to reduceexcessive drinking inCardiff city centre
2004
Wales
Reduce excessive drinking in the city centre.Improve regulation of licensed premises byfeedback of individual risk assessments ofpremises and RBS. Awareness-raising.Community Safety Partnership focus on reducingcrime and disorder.Test purchasing, police/National Health Servicestatistics, environmental audits.Reduce alcohol-related harm in the communityusing a multi-component approach. Focus onlicensed premises. Engage in partnershipworking.RBS, strict enforcement, awareness-raising —publicity campaigns and partnership working.Test purchasing, police statistics, survey.
‘Route 50’ Project,Birmingham
2005
England
Chapter 10: Alcohol harm reduction in Europe
285
Public place wounding decreased by –29.5 % within800m of project area and more than neighbouringpolice area (–17.2 %) (but caution as numbers small).Signs that awareness raised — e.g. Pubwatchestablished and active, community forum on alcohol.Partnerships established and active (e.g. police,licensees, local government).(Mistral et al., 2007)
Harm reduction: evidence, impacts and challenges
286
Table 10.3(continued)Goal, intervention and outcome measuresA controlled experiment in a provincial town,focusing on normative misperceptions/exaggerated beliefs amongst Danish youth inrelation to the use of tobacco, alcohol and drugs.To prevent drink-driving: information campaignduring a beer festival in Arezzo province in2005.During the festival social and health workersoffered information and the opportunity tomeasure BAC using alcohol tests.To prevent drink-driving: social campaign ondrink-driving (radio, poster, free cards, discoevents with information and alcohol testing).Evaluation of the campaign: 1 451questionnaires, 1 235 interviews, 1 focus group,11 health worker diaries.More than 50 % of people who did the alcoholtests were positive (more than 0.5g/l BAC).(Ranieri et al., 2007)Statistically significant reduction in the use ofalcohol and general risk behaviour.(Balvig et al., 2005)
Name of project
Start date
Country
Main findings
The Ringsted Project
2001
Denmark
‘Caschiamoci’
2005
Italy
‘Questa serachiamatemi Bob’ — adesignated drivercampaign
2005
Italy(Piedmont)
Positive evaluation of the campaign.Positive evaluation of information activities in thediscos (10), both about methods (gadget, alcoholtesting) and quality of information.Positive evaluation about security driving courseaward.Suggestion for future campaign.(Beccaria and Marchisio, 2006)
Chapter 10: Alcohol harm reduction in Europe
Multi-component programmesMulti-component programmes involve the identification of alcohol-related problems at thelocal level and implementation of a programme of coordinated projects to tackle theproblem, based on an integrative design where singular interventions run in combinationwith each other and/or are sequenced together over time; the identification, coordinationand mobilisation of local agencies, stakeholders and community are key elements (Thom andBayley, 2007). Furthermore, as Thom and Bayley (2007) note, evaluation is an integral partof multi-component programmes; both the overall programme and the individual projectswithin it should have clearly defined aims, objectives and measures of effectiveness. Anotherkey element is that projects and the programme as a whole should have a strategicframework underpinned by a theoretical base.The ‘systems theory approach’, which is closely associated with the work of Holder andcolleagues in the United States (Holder, 1998), and the ‘community action’ approach havebeen particularly influential (see Thom and Bayley, 2007, pp. 35–9). The United States,Australia and New Zealand were at the forefront of the development of multi-componentprogrammes in the alcohol field and influenced the establishment of such programmes inEurope (e.g. Holmila, 2001). Multi-component programmes have been conducted inScandinavia, Italy, Poland and the United Kingdom (see box on p. 288 and Table 10.3) andhave included a range of harm reduction projects. Whilst the specific targets of the multi-component programmes vary, the majority aim to influence community systems and changedrinking norms, and most aim to mobilise local communities with the intention of securingsustainable, long-term change. For example, STAD (Stockholm prevents Alcohol and Drugproblems), a multi-component community programme in Sweden that ran 1996–2006,included responsible beverage service training, community mobilisation and strictenforcement of alcohol laws (Wallin, 2004; Wallin et al., 2003a; Wallin et al., 2003b; Wallinet al., 2004; Månsdotter et al., 2007).So, do multi-component programmes work? There is, as Thom and Bayley (2007) conclude, ‘no simple answer’ to this question. Whilst there is evidence from internationalresearch as to what is likely to work at a ‘stand alone’ level (see Table 10.2), what is lessclear is how they work in combination or what kind of combinations may result in aneffective multi-component programme. This is in part because of the expected synergisticeffect of the components and also the possible cumulative effects over time; furthermore,it has not been possible to identify the contribution of particular components toprogramme outcomes as a whole (US Department of Health and Human Services, 2000).For example, educational and awareness-raising campaigns are often cited as ineffectivein changing behaviour (see Table 10.2) but are seen as a crucial element of most multi-component programmes. Anderson and colleagues (2009) argue that although theevidence shows that information and education programmes do not reduce alcohol-related harm, they do play a key role in providing information and in increasingawareness of the need to place alcohol issues firmly on public and political agendas(Anderson, et al., 2009).287
Harm reduction: evidence, impacts and challenges
Examples of multi-component programmes in Europe
Name of projectAquarius South Birmingham Community Alcohol Action Project(‘Route 50’ project) (UKCAPP)Lahti ProjectMetropolitan Suburbs ProjectLocal Alcohol Policy Project (PAKKA)Florence (Rifredi) Community Alcohol Action ProjectFlorence (Scandici) Community Alcohol Action ProjectDrinking and driving related injuries, FlorenceCommunity Action Project, MalczyceReducing alcohol-related injury, violence and disorder in the citycentre: Glasgow (UKCAPP)The Kiresberg Project (demonstration)Kungsholmen ProjectStockholm Prevents Alcohol and Drug Problems (STAD)Six Communities ProjectMulti-agency, community-based intervention to reduce excessivedrinking in Cardiff city centre (‘Lion’s Breath’) (UKCAPP)Source:Adapted from Thom and Bayley, 2007, pp. 62–3.
CountryEngland
Start date2004
FinlandFinlandFinlandItalyItalyItalyPolandScotland
19921997200419921999200419942004
SwedenSwedenSwedenSwedenWales
19881990199620032004
Although evaluation is integral to multi-component programmes, in reality these evaluationsare complex and it is not only difficult to untangle the effects of the interventions from eachother, but also from other activities in the locality. In relation to the evaluation of the threeprojects in the United Kingdom Community Alcohol Prevention Programme (UKCAPP), Mistralet al. commented:The UKCAPP projects were part of a multi-faceted web of other local projects, partnerships, andinterventions … The complexity of these partnerships meant that it was impossible to consider anyUKCAPP project as a discrete set of interventions, clearly delineated in space, and time, theeffects of which could be evaluated independently of other local activities.(Mistral et al., 2007, p. 86)
288
Chapter 10: Alcohol harm reduction in Europe
Another important issue highlighted by the UKCAPP evaluation was the inadequacy ofstatistical datasets, which meant that it was impossible to judge the effectiveness ofinterventions over time (Mistral et al., 2007). This was in part due to the different methods ofdata collection, analysis and retrieval used by police, ambulance service and emergencycare departments, which made data validity hard to verify and comparison across sources orsites highly problematic (Mistral et al., 2007). In addition, local issues (e.g. timing ofintervention, funding delays, getting agreement from all partners) can make systematic localevaluation challenging.In summary, whilst some programmes have reported considerable successes (e.g. CommunityTrials Project, reported by Holder, 2000), others have yielded more mixed results, includingthe Lahti project in Finland (Holmilia, 1997), Kiresberg project (Hanson et al., 2000) andSTAD (Wallin et al., 2003a) in Sweden. However, Thom and Bayley (2007) in their overviewconclude that the evidence suggests that a multi-component approach has a greater chanceof success than stand-alone projects.
Harm reduction interventionsImproving the drinking environmentObservational studies indicate that the drinking environment of licensed premises can impacton the risk of violence and injury. A lack of seating, loud music, overcrowding, unavailabilityof food are considered risk factors (Graham and Homel, 2008; Homel et al., 2001; Rehm etal., 2003). A variety of initiatives to improve the drinking environment have beenimplemented. These include server training, awards to well-managed licensed premises andthe use of safety glassware (or plastic). A recent systematic review concluded that there wasno reliable evidence that interventions such as these in the alcohol server setting are effectivein preventing injuries (Ker and Chinnock, 2008). Nevertheless, we look at some of theresearch findings for each of these interventions in turn.Server trainingA number of European countries including Spain, United Kingdom, Ireland and theNetherlands have developed national responsible beverage service (RBS) training andaccreditation schemes (EFRD website, 2009). Responsible beverage service is a keyfeature of many Scandinavian and United Kingdom multi-component programmes (seeTable 10.3), with the aim of reducing sales to minors, over-serving and violence in andaround licensed premises. These interventions usually involve formal training of staff andstrict enforcement of existing alcohol laws; outcome measures include test purchasing andpolice statistics.Results have been mixed. The STAD project in Sweden took a quasi-experimental approachwith a control area, also located in central Stockholm, but not adjacent to the project area. In289
Harm reduction: evidence, impacts and challenges
relation to both over-serving and serving to minors there was a statistically significantreduction in both the control and project areas, although in the project area the improvementin relation to over-serving was slightly higher (but not statistically significant) (Wallin et al.,2003a). Wallin et al. (2003a) note that during the time of research the Stockholm LicensingBoard (which covers both areas) altered practices and policy, and this might be oneexplanation for why there were changes in alcohol service in both the project and the controlarea (i.e. spill-over effects).In contrast, there was a reduction in violence only in the project area, with a 29 % reductionin police-reported violence in and around licensed premises (Wallin et al., 2003b). Theauthors put forward several explanations for this result. First, there were a greater number oflarge nightclubs in the project area and changes in practice in large establishments mayhave a greater impact than changes in smaller establishments. Second, it may be a synergyeffect, with improved serving practices and increased enforcement combining to produce apositive effect (Wallin et al., 2003b; SNIPH, 2008). Although it did appear to be harder foryouths to get served in the project site than the control, the differences were not statisticallysignificant (SNIPH, 2008).Other studies, for example in Trondheim, Norway, experienced a low uptake of theintervention, and not surprisingly no impact was observed (Baklien and Buvik, 2006). The‘Route 50’ project in Birmingham, an area with no history of partnership working, facedsimilar challenges, but boosted uptake by providing incentives (e.g. waived the course fee)(Mistral et al., 2007). Whilst there were decreases in police-recorded statistics compared tothe adjacent area, the number of crimes was low and thus no inferences could be safelydrawn (Mistral et al., 2007).
Awards for management of premisesIn 2003, as part of a broad, multi-agency programme to reduce alcohol-related crime anddisorder in the city centre area, Manchester developed a scheme, called ‘Best Bar None’(BBN), to identify and recognise the best-managed licensed premises in the area (HomeOffice, 2004) (see box on p. 291 for details). The scheme has since been rolled outnationally, but despite this BBN has yet to be fully evaluated. Although ‘a detailedassessment’ of the impact of BBN on reducing disorder is planned (Harrington, 2008), asmall-scale evaluation concluded that there was ‘a lack of credible evidence to suggest thatthe implementation of the BBN scheme in Croydon has specifically had an impact on thereduction of crime and disorder in the town centre on its own’ (GOL, 2007, p. 2). Whilstacknowledging there were benefits for those who implemented the scheme, these benefitswere difficult to measure and ‘largely amount to perception rather than evidenced reality’(GOL, 2007, p. 2). The report recommended that if the BBN is to continue, then an agreedmeasuring tool (that is, set of indicators) is required, so that the impact of the schemes canbe assessed and can provide credible evidence for other areas considering itsimplementation (GOL, 2007).290
Chapter 10: Alcohol harm reduction in Europe
From pilot project to national scheme — Best Bar None2003BBN developed within Manchester’s ‘City Safe Scheme’.Quickly adopted by other towns in the United Kingdom.2007Agreement reached between Greater Manchester Police, the Home Office and British Instituteof Innkeeping (the professional body for the licensed retail sector), to develop the schemenationally.2008Over 90 schemes in place (Harrington, 2008).Features of the BBN scheme:• nvolves:partnership with the licensing industry, police, local and central government,Ihealth workers and other agencies.• ims:to make licensees and the public aware of safety levels within premises, and reduceAalcohol-related crime and irresponsible drinking.• ets:national standards of good practice in the management of licensed premises.S• wards:the best-managed licensed premises in an area — gold, sliver and bronze-Arepresent the levels to which the premises are assessed as meeting the standards.Premises gaining an award display a plaque.
Use of safety glasswareResearch in the United Kingdom identified that bar glasses were being used as weapons toinflict injuries, in particular to the face (Shepherd et al., 1990b). Further research concludedthat the use of toughened glass would reduce injuries (Shepherd et al., 1990a; Warburtonand Shepherd, 2000). This research led to the replacement of ordinary glassware withtoughened glassware in licensed premises and there is evidence from the British CrimeSurvey that this change resulted in a significant reduction of violent incidents involving the useof glasses or bottles as weapons (Shepherd, 2007). However, Shepherd (2007) notes thatreductions in glass injury have not been sustained — probably because of the increasedavailability of bottled drinks and the use of poorly toughened glass. Despite repeated calls,there is, as yet, no manufacturing standard but the use of alternative materials, particularlyplastics, is seen as a way forward.In 2006, as part of its approach to reducing alcohol-related violence and disorder in thecity centre, Glasgow city council banned the use of glassware (other than special ‘safety’glass) from venues holding an entertainment licence — which in practice meant nightclubs(Forsyth, 2008). However, individual premises could apply for an exemption for291
Harm reduction: evidence, impacts and challenges
champagne/wine glasses (Forsyth, 2008). The study, based on naturalistic observationsand interviews, reported that exemptions to the ban had allowed some premises tocontinue to serve in glass vessels, and this resulted in injuries. Although disorder in all-plastic venues was observed, it incurred less injury risk and Forsyth (2008) concluded thatthe research demonstrated the potential of such policy to reduce the severity of alcohol-related violence in the night-time economy. Earlier initiatives, for example ‘Crystal Clear’in Liverpool, aimed to remove glass from outdoor public places in the city centre in orderto reduce glass injuries; a high-profile awareness campaign was mounted and actiontaken by bar and door staff to prevent glass being removed (Young and Hirschfield,1999). The evaluation found that there was high recognition of the campaign and policeand hospital data showed a reduction in glass injuries during the campaign (Young andHirschfield, 1999).Reducing the harms associated with drink-drivingSystematic reviews and meta-analyses have found that highly effective drink-driving policiesinclude lowered blood alcohol concentration (BAC), unrestricted (random) breath testing,administrative licence suspension, and lower BAC levels and graduated licenses for novicedrivers (Babor, et al., 2003; Anderson, et al., 2009). Less effective are designated driverschemes and school-based education schemes (Babor et al., 2003). We look at threeexamples — BAC measures, ‘alcolocks’ (or alcohol-interlocks, which are devices that preventa motor vehicle from starting when a driver’s BAC is elevated) and designated driverschemes.BAC measuresAll European countries place legal limits on the BAC of drivers and the 2001 EuropeanCommission Recommendation on the maximum permitted blood alcohol concentration(BAC) for drivers of motorized vehicles called for all Member States to adopt a BAC of0.5 g/L, lowered to 0.2 g/L for novice, two-wheel, large vehicle or dangerous goodsdrivers; in addition, random breath testing was recommended so that everyone is checkedevery three years on average (Anderson, 2008). There are currently three Member Statesof the EU-27 that have a BAC limit of greater than 0.5 g/L (Ireland, Malta and the UnitedKingdom) (ETSC, 2008). There is evidence that the reduction in BAC limits supported bystrict enforcement and publicity can reduce drink-driving at all BAC levels. For example,Switzerland reduced the legal BAC limit from 0.8 g/L to 0.5 g/L and introduced randombreath testing in January 2005. The number of alcohol-related road deaths in 2005reduced by 25 per cent and contributed to an overall 20 % reduction in the number ofroad deaths (ETSC, 2008).AlcolocksAlcolocks (or alcohol-interlocks) are devices that prevent a motor vehicle from startingwhen a driver’s BAC is elevated. Sweden introduced two alcolock programmes in 1999,292
Chapter 10: Alcohol harm reduction in Europe
which have been evaluated. One programme involved commercial drivers (of taxis,lorries and buses); in 600 vehicles, 0.19 % of all starts were prevented by a BAC higherthan the legal limit and lock point of 0.2 g/L, mostly during weekends and mornings(Bjerre and Kostela, 2008). Another was a voluntary two-year programme for drinkingwhile intoxicated (DWI) offenders, which included regular medical monitoring designedto reduce alcohol use and was offered in lieu of having licence revoked for a year. Therewere two control groups; one group had revoked licences but did not have theopportunity to participate in an interlock programme, and the other comprised DWIoffenders who had declined the opportunity to participate in the programme (Bjerre andThorsson, 2008). Only 11 % of eligible drivers took part in the programme. Theintervention group were significantly more likely to be re-licensed two and three yearsafter the DWI offence than the control groups and also, according to Alcohol UseDisorder Identification Test (AUDIT) scores, had lower rates of harmful alcoholconsumption. In the post-treatment period the rate of DWI recidivism was about 60 %lower, and the rate of police-reported traffic accidents about 80 % lower than during theyears before the offence. Among the controls being re-licensed, a similar reduction intraffic accidents was observed but not in DWI recidivism. Bjerre and Thorsson (2008)conclude that these results suggest that the alcolock programme was more effective thanthe usual licence revocation and also that it was a useful tool in achieving lastingchanges in the alcohol and drink-driving behaviour of DWI offenders. To date systematicreviews of research indicate that alcolocks are only effective whilst in situ (Willis et al.,2004; Anderson, 2008) and further work is required into what steps need to be taken toprevent recidivism and ensure behaviour changes are sustained.
Designated driver schemesThe designated driver concept was first initiated in Belgium in 1995, jointly by the(industry-funded) Belgian Road Safety Institute and Arnouldous (EFRD, 2007). Designateddriver campaigns are currently running in 16 European countries (EFRD, 2009) and wereco-financed by the European Commission for five years (ETSC, 2008). Table 10.3provides a summary of an evaluated designated driver scheme in Italy (Beccaria andMarchisio, 2006). There is no universal definition of a ‘designated driver’, but the mostcommon definition requires that the designated driver does not drink any alcohol, beassigned before alcohol consumption, and drive other group members to their homes(see Ditter et al., 2005). Other definitions adopt a risk and harm reduction strategy, inwhich the main goal is not necessarily abstinence, but to keep the designated driver’sblood alcohol content (BAC) at less than the legal limit. The evidence is that although theBACs of designated drivers are generally lower than those of their passengers they arestill often higher than the legal limit for drinking and driving. Furthermore, an increase inpassenger alcohol consumption is often found when a designated driver is available. Todate, no study has evaluated whether the use of designated drivers actually decreasesalcohol-related motor vehicle injuries (Anderson, 2008). Anderson (2008) argues thatexisting designated driver campaigns should be evaluated for their impact in reducingdrink-driving accidents and fatalities before financing and implementing any newcampaigns.293
Harm reduction: evidence, impacts and challenges
Alcohol harm reduction in Europe: non-evaluated harm reductioninitiativesIn this section, we look at examples of harm reduction initiatives that have been recordedand described in the literature but not thoroughly evaluated, and also at examples given byour key informants (see box below). Harm reduction initiatives often begin as practicalresponses to a problem rather than as a research question and thus are not usually formallyevaluated, at least not in the first instance. Information about such initiatives at the local levelis often difficult to come by. This indicates that there is a need for systematic pooling ofinformation, particularly for dissemination of knowledge about smaller local or regionalinitiatives. One attempt at systematic collection of data is being promoted in the UnitedKingdom. The Hub of Commissioned Alcohol Projects and Policies (HubCAPP) is an onlineresource of local alcohol initiatives focused on reducing alcohol-related harms to healththroughout England (www.hubcapp.org.uk) launched in 2008. The focus of HubCAPP is onidentifying and sharing local and regional practice in relation to reducing alcohol harm, andit is constantly expanding. Although not exclusively a database of harm reduction initiatives,many of the projects can be classified as such, for example, the ‘Route 50 Project’ a multi-component, community-based initiative in Birmingham (Goodwin and McCabe, 2007).
Harm reduction initiatives: some examples that have been recorded and described• Flip-flops’ (simple flat shoes) given to women who are experiencing difficulties walking in‘high heels (to prevent injuries from falling over or from walking barefoot). United Kingdomtowns including Torquay, Bognor, Rugby.• ollipops (sweets) given to people as they leave venues by door staff (to keep them quiet andLto raise blood sugar so that they are more alert and less inclined to violence). United Kingdomtowns including Southampton, Manchester, Guildford, London.• ubble blowers (which double as pens) handed out (focus on having fun blowing bubbles,Breduce anti-social behaviour and violence). Bolton, United Kingdom.• arent volunteers known as natteravnene (Night Owls) walk the streets at night in distinctivePyellow jackets. They do not intervene in the night life but believe that their presence canreduce trouble, fights and vandalism. They also hand out sweets, water, sandwiches andcondoms. Denmark.• irst aid assistance provided for young people at open air drinking gatherings. Spain.F• lcohol testing for drivers leaving a three-day music festival. Slovakia.A• MS service — text what you have drunk and get back an estimate of BAC. CzechSRepublic.• arent-organised youth parties for 14- to 18-year-olds. Young people bring their ownPbeverages and drink under the supervision of parents. Denmark.• ublic transport runs until the early morning at the weekends and provided free on NewPYear’s Eve. Poland.• obering up stations — safe places where intoxicated drinkers are taken to sober up (i.e.Saway from the cold and threats of violence). Poland, Czech Republic, Russia and otherformer Soviet nations.
294
Chapter 10: Alcohol harm reduction in Europe
Some of the non-evaluated initiatives can be described as ‘grassroots’ interventions, that is,they have been devised and initiated by lay people (e.g. parents, members of a localcommunity) to reduce alcohol-related harm within the local community. For example, inprovincial Denmark, parents have organised parties where young people drink alcoholunder adult supervision, with the aim of reducing harmful drinking in unsupervised outdoorareas (Kolind and Elmeland, 2008). In similar vein, in Slovakia, in an attempt to supervisethe behaviour of young people coming home from parties, pubs and discos, local peopleand police formed patrols to guide young people home safely and with minimaldisturbance to the community. Grassroots initiatives are generally pragmatic and reactiveand they may also be very specific to a time and place. However, if such initiatives appearto be ‘successful’ they may over time be subject to formal evaluation and also beimplemented in other areas.Other initiatives have been developed by agencies such as police, local government, healthand welfare agencies, often working in partnership, and like the ‘grassroots’ initiatives theyare aimed at reducing alcohol-related harm in the local area. Such initiatives are ofteninnovative, for example, giving out ‘goody bags’ containing items including sweets, ‘flip-flops’(simple flat shoes), water, condoms and information leaflets on alcohol and safer sex, as partof campaigns to reduce alcohol-related harm and disorder in town centres (ChichesterObserver,2008; Hope, 2008; Lewisham Drug and Alcohol Strategy Team, 2007). Theinnovative nature of these interventions generates media coverage, much of which is negativeor cynical (e.g. Hope, 2008; Salkeld, 2008; Smith, 2008 — on bubble blowers, flip-flops andlollipops), and some groups (e.g. Taxpayers’ Alliance, United Kingdom) dismiss these harmreduction measures as ‘gimmicks’ and a ‘waste of money’.Whilst most of these measures have been introduced relatively recently, other interventionshave a longer history. For example, the first ‘sobering up station’ (záchytka) opened inCzechoslovakia (now the Czech Republic) in 1951. It provided a place for intoxicated peopleto sober up. It was a model that was soon adopted by other countries, including Polandwhich established sobering up stations following the decriminalisation of public drunkennessin 1956 (Moskalewicz and Wald,1987). Facilities that serve a similar function are dottedacross Europe; for example Scotland has two ‘designated places’ (in Aberdeen andInverness), which provide an alternative to custody for persons arrested for being drunk andincapable; they are monitored in a safe environment until fit to leave, and further help isavailable. There have been calls for a comprehensive system of ‘designated places’ toprovide a safe place for intoxicated people to sober up and to divert them from the criminaljustice and health systems (BBC, 2007).There are a number of routes by which knowledge of successful interventions is spread,both informal and more formal, including identification, dissemination and awards for‘best practice’ (e.g. by government agencies, interest groups), fact finding visits, webresources (e.g. HubCAPP in the United Kingdom), stakeholder networks and organisations(e.g. Global Alcohol Harm Reduction Network — GAHRA-Net). The Internet plays a keyrole in the exchange of information globally through websites, online publications, andvirtual networks.295
Harm reduction: evidence, impacts and challenges
Policy and knowledge transfer can be aided by thorough evaluation of interventions. Butwhilst it is straightforward to find a description of a simple ‘evaluation’ of a particularintervention, as we have seen in the case of BBN, robust, comprehensive evaluation is oftenlacking. However, it is not merely a question of the evaluation of interventions. What works inprovincial Denmark may not work in inner city Paris, and care needs to be taken not tosimply ‘cherry pick’ interventions. Cultural and local contexts are important factors intransferring intervention models and are often ignored when apparently successful projectsor programmes are ‘rolled out’.
ConclusionCurrent usage and definition of the concept of harm reduction derives from the drugs fieldrather than from the long history of formal and informal regulation of alcohol-related harm.The lack of consensus regarding the definition and a tendency to include within the definitioninitiatives that are contested as being ‘prevention’ and not really ‘harm reduction’, suggests botha risk that the adoption of a very broad definition may result in loss of meaning and usefulnessof the concept for policy and practice and an opportunity to debate and clarify the conceptand its application in differing national, local and cultural contexts. Apart from the distinctionbetween measures that aim to reduce consumption, and measures that tackle only associatedharms, approaches to reduce or minimise harm once it has happened (harm reduction) can bedistinguished from risk reduction measures, which aim to prevent harm being caused in the firstplace. These nuances of meaning have important implications for the development of strategy,the adoption of specific projects and programmes, the evaluation of policies and initiatives andfor the effectiveness outcomes researchers choose to measure. Although the evidence base forharm reduction approaches appears less solid than the evidence for measures to reduceconsumption, there has been far less research and fewer evaluated studies of measures thataddress the harms without necessarily requiring lower consumption. This would be useful, bothin designing locally appropriate multi-component programmes and in providing a ‘menu’ ofevaluated initiatives to run alongside measures aimed at consumption levels.It is also essential to establish the boundaries of inclusion in ‘harm reduction’ if more effectivesystems for information sharing and data collection in Europe are to be agreed. Informationon harm reduction approaches — especially those that emerge from local or grassrootsactivity — is hard to come by. Descriptions on websites are often ephemeral, and this is areflection also of the origins of harm reduction activity, which is frequently rooted in transientlocal concern and crises. As the crisis or concern recedes, the initiatives fade away. At thesame time, most harm reduction activity appears to be semi-official (as opposed to grassrootsor lay), emerging at regional or local levels from professional and local authority action.Sometimes a particular initiative catches the policy and public attention and is transferredfrom one area to another, based more on the perception of success rather than on anyevaluation or formal assessment of effectiveness or of the appropriateness of transfer fromone setting to another. The development of information sharing systems, nationally andpossibly on a European scale, would be a step forward in providing the field with a morecomprehensive overview of harm reduction measures, settings in which they have beenimplemented and with what results, and measures of effectiveness.296
Chapter 10: Alcohol harm reduction in Europe
While harm reduction ‘thinking’ has joined the raft of policy strategies and local initiatives inmost European countries, remarkably few initiatives have been fully described, let alonescientifically evaluated with any degree of rigour. This in itself may be one reason whyassessments of effectiveness based on international research result in harm reductionmeasures being reported as less effective. However, before demanding conformity to ‘goldstandard’ evaluation studies, it is worth considering the nature and uses of many harmreduction approaches. If, as appears to be the case, harm reduction requires flexibility andimmediacy in its reaction to locally defined need, there is a case for arguing that descriptionsof the approach and narratives of the implementation and perceived outcomes are moreuseful than formal (expensive) evaluation. Such narratives are largely missing and could bean important addition to information banks such as the United Kingdom’s HubCAPP.Evaluation and research findings are, of course, only one element in decisions to adopt orreject harm reduction as a legitimate goal for policy and in decisions about which initiativesare suitable for implementation nationally or locally. Success or failure of harm reductioninitiatives can depend as much on media and public perceptions (as in the case of ‘flip-flops’)or on gaining the collaboration of stakeholders (as in the case of server training) or thewillingness of volunteers (as in the Danish ‘Night Owls’ and the Danish parents’ parties) as onthe evaluated effectiveness of a particular strategy or activity. This is especially the case if theevaluations emerge from projects located in very different social, cultural and politicalsystems. So questions arise as to what extent harm reduction is seen as an appropriateapproach to reducing alcohol-related harms in the different countries of Europe. Is harmreduction the ‘conventional wisdom’ in Europe or are there countries where harm reduction isthought to be inappropriate to that particular country’s cultural context and consumptionpatterns? These are questions that deserve further exploration. In the drive towards a Europe-wide planned approach to tackling alcohol-related harm, this overview of harm reductionapproaches highlights the need to develop opportunities and systems to facilitate knowledgetransfer on alcohol harm reduction between researchers, policymakers and practitioners inEurope, but stresses the importance of respecting local and cultural diversity in thedevelopment and implementation of harm reduction initiatives.
ReferencesAnderson, P. (2008),Reducing drinking and driving in Europe,Deutsche Hauptstelle für Suchtfragen e.V. (DHS),Hamm.Anderson, P. and Baumberg, B. (2006),Alcohol in Europe: a public health perspective. A report for the EuropeanCommission,Institute of Alcohol Studies, London. Available at http://ec.europa.eu/health-eu/doc/alcoholineu_content_en.pdf (accessed 20 July 2009).Anderson, P., Chisholm, D. and Fuhr, D. (2009), ‘Effectiveness and cost-effectiveness of policies and programmesto reduce the harm caused by alcohol’,Lancet373, pp. 2234–46.Babor, T., Caetano, R., Casswell, S., et al. (2003),Alcohol: no ordinary commodity,Oxford University Press,Oxford.Babor, T. F. (2008),Evidence-based alcohol control policy: toward a public health approach,Conference onTobacco and Alcohol Control — Priority of Baltic Health Policy, Vilnius.
297
Harm reduction: evidence, impacts and challenges
Baklien, B. and Buvik, K. V. (2006),Evaluation of a responsible beverage service programme in Trondheim,Sirus-Reports 4 (English summary), SIRUS, Oslo. Available at http://www.sirus.no/internett/alkohol/publication/310.html (accessed 20 January 2010).Balvig, F., Holmberg, L. and Sørensen, A-S. (2005),Ringstedforsøget. Livsstil og forebyggelse i lokalsamfundet[TheRingsted project: lifestyle and prevention in the local community], Jurist-og Økonomiforbundets Forlag,København.BBC (2007),Profits ‘to aid alcohol problems’,BBC News 10 October 2007. Available at http://news.bbc.co.uk/1/hi/scotland/north_east/7036806.stm (accessed16 July 2009).Beccaria, F. and Marchisio, M. (2006), ‘Progetto Bob. Vatutazione di una compagna di promozione delguidatore designato’,Dal fare al dire15 (2), pp. XII–XX.Bjerre, B. (2005), ‘Primary and secondary prevention of drink driving by the use of alcolock device and program:Swedish experiences’,Accident Analysis and Prevention37 (6), pp. 1145–52.Bjerre, B. and Kostela, J. (2008), ‘Primary prevention of drinking driving by the large-scale use of alcolocks incommercial vehicles’,Accident Analysis and Prevention40 (4), pp. 1294–9.Bjerre, B. and Thorsson, U. (2008), ‘Is an alcohol ignition interlock programme a useful tool for changing thealcohol and driving habits of drink-drivers?’,Accident Analysis and Prevention40 (1), pp. 267–73.Bystoń, J. (1960),Dzieje obyczajów w dawnej Polsce.Wiek XVI-XVII. PIW, Warszawa.Chichester Observer(2008), ‘Police to hand out flip flops to clubbers in Bognor’, 26 December.Ditter, S. M., Elder, R. W., Shults, R. A., et al., (2005), ‘Effectiveness of designated driver programs for reducingalcohol-impaired driving a systematic review’,American Journal of Preventative Medicine28 (5 Supplement), pp.280–7.EFRD (European Forum for Responsible Drinking) (2007),Guidelines to develop designated driver campaigns,EFRD, Brussels.EFRD (2009), European Forum for Responsible Drinking website at www.efrd.org/main.html (accessed 9 March2009).ETSC (European Transport Safety Council) (2008),Drink driving fact sheet.Available at www.etsc.eu/documents/Fact_Sheet_DD.pdf (accessed 9 March 2009).Forsyth, A. J. M. (2008), ‘Banning glassware from nightclubs in Glasgow (Scotland): observed impacts,compliance and patrons’ views’,Alcohol and Alcoholism43 (1), pp. 111–17.Goodwin, P. and McCabe, A. (2007),From loose, loose to win, win: Aquarius Route 50 project. Report to the AERC.Available at: www.hubcapp.org.uk (accessed 9 March 2009).GOL (Government Office for London) (2007),Best Bar None Croydon review,GOL, London. Available at http://ranzetta.typepad.com/Croydon_BBN_evaluation.doc (accessed 9 March 2009).Graham, K. and Homel, R. (2008),Raising the bar: preventing aggression in and around bars, pubs and clubs,Willan Publishing, Cullompton.Hanson, B. S., Larsson, S. and Rastram, L. (2000), ‘Time trends in alcohol habits: results from the Kiresbergproject in Malmo, Sweden’,Substance Use and Misuse35 (1 & 2), pp. 171–87.Harrington, J. (2008), ‘Sky’s the limit for Best Bar None’,Morning Advertiser,16 June. Available at http://www.morningadvertiser.co.uk/news.ma/article/62912 (accessed 12 March).
298
Chapter 10: Alcohol harm reduction in Europe
Holder, H. D. (1998),Alcohol and the community: a systems approach to prevention,Cambridge University Press,Cambridge.Holder, H. D. (2000), ‘Community prevention of alcohol problems’,Addictive Behaviours25 (6), pp. 843–59.Holder, H. D. (2004), ‘Community action from an international perspective’, in Müller, R. and Klingemann, H.(eds),From science to action? 100 years later – alcohol policies revisited,Kluwer Academic Publishers, Dordrecht,pp. 101–12.Holmlia, M. (1997),Community prevention of alcohol problems,Macmillan Press, Basingstoke.Holmlia, M. (2001), ‘The changing field of preventing drug and alcohol problems in Finland: can community-based work be the solution?’,Contemporary Drug Problems28 (2), pp. 203–20.Holmila, M. and Warpenius, K. (2007), ‘A study on effectiveness of local alcohol policy: challenges andsolutions in the PAKKA project’,Drugs: Education, Prevention and Policy14, pp. 529–41.Home Office (2004),Alcohol audits, strategies and initiatives: lessons from Crime and Disorder ReductionPartnerships,Home Office Development and Practice Report 20,Home Office, London.Homel, R., McIlwain, G. and Carvolth, R. (2001), ‘Creating safer drinking environments’, in Heather, N., Peters, T.and Stockwell, T. (eds),International handbook of alcohol dependence and problems,John Wiley & Sons Ltd,Chichester, pp 721–40.Hope, C. (2008), ‘Police give free goodie bags containing condoms, flip-flops and lollipops to drinkers’,DailyTelegraph,20 December. Available at www.telegraph.co.uk/news/newstopics/politics/lawandorder/3850898/Police-give-free-goodie-bags-containing-condoms-flip-flops-and-lollipops-to-drinkers.html (accessed 4 February2009).IHRA (International Harm Reduction Association) (n.d.), ‘What is alcohol harm reduction?’ Available at www.ihra.net/alcohol (accessed 4 February 2009).Kaner, E. F. S., Dickinson, H. O., Beyer, F. R., et al. (2007), ‘Effectiveness of brief alcohol interventions in primarycare populations’, Cochrane Database of Systematic Reviews 2007, Issue 2, Art. No.: CD004148. DOI:10.1002/14651858.CD004148.pub3.Ker, K. and Chinnock, P. (2008), ‘Intervention in the alcohol server setting for preventing injuries’, CochraneDatabase of Systematic Reviews, Issue 3, Art No.: CD005244. DOI: 10.1002/14651858.CD005244.pub3.Kolind, T. and Elmeland, K. (2008), ‘New ways of socializing adolescents to public party-life in Denmark’, inOlson, B. and Törrönen, J. (eds),Painting the town red: pubs, restaurants and young adults’ drinking cultures in theNordic countries,Vol. 51, NAD (Nordic Centre for Alcohol and Drug Research), Helsinki, pp. 191–219,Lachenmeier, D., Rehm, J. and Gmel, G. (2007), ‘Surrogate alcohol: where do we know and where do we go?’,Alcoholism: Clinical and Experimental Research31910, pp. 1613–27.Lang, K., Väli, M., Szűcs, S., Ádány, R. and McKee, M. (2006), ‘The composition of surrogate and illegal alcoholproducts in Estonia’,Alcohol and Alcoholism41 (4), pp. 446–50.Lenton, S. and Single, E. (1998), ‘The definition of harm reduction’,Drug and Alcohol Review,17 (2), pp. 213–19.Leon, D. A., Saburova, L.,Tomkins, S., et al. (2007), ‘Hazardous alcohol drinking and premature mortality inRussia: a population based case-control study’,Lancet369 (9578), pp. 2001–9.Lewisham Drug and Alcohol Strategy Team (2007),Don’t binge and cringe evaluation: Lewisham 2007 anti-bingedrinking festive campaign.Available at www.alcoholpolicy.net/files/dont_binge_and_cringe_evaluation.pdf(accessed 4 February 2009).
299
Harm reduction: evidence, impacts and challenges
Månsdotter, A. M., Rydberg, M. K., Wallin, E., Lindholm, L. A. and Andréasson, S. (2007), ‘A cost-effectivenessanalysis of alcohol prevention targeting licensed premises’,European Journal of Public Health17, pp. 618–23.McKee, M., Suzcz, S, Sárváry, A., et al. (2005), ‘The composition of surrogate alcohols consumed in Russia’,Alcoholism Clinical and Experimental Research29, pp. 1884–8.Mistral, W., Velleman, R., Mastache, C. and Templeton, L. (2007),UKCAPP: an evaluation of 3 UK CommunityAlcohol Prevention Programs. Report to the Alcohol Education and Research Council.Available at www.aerc.org.uk/documents/pdfs/finalReports/AERC_FinalReport_0039.pdf (accessed 10 February 2009).Moskalewicz, J. and Wald, I. (1987), ‘From compulsory treatment to the obligation to undertake treatment:conceptual evolution in Poland’,Contemporary Drug ProblemsSpring, pp. 39–51.Nicholls, J. (2009),The politics of alcohol: a history of the drink question in England,Manchester University Press,Manchester.Nilsen, P., Kaner, E. and Babor, T. F. (2008), ‘Brief intervention, three decades on: an overview of researchfindings and strategies for more widespread implementation’,Nordic Studies on Alcohol and Drugs25 (6), pp.453–67.Pratt, E. A. (1907),Licensing and temperance in Sweden, Norway and Denmark,John Murray, London.Prochard, H. (1902), ‘Through the heart of Patagonia, London’, quoted in Horton, D. (1943), ‘The functions ofalcohol in primitive societies: a cross-cultural study’,Quarterly Journal of Studies on Alcohol4.Ranieri, F. et al. (2007), ‘Prevenzione ad una festa della birra?’,S&P: Salute e Prevenzione: La Rassegna Italianadelle Tossicodipendenze22 (45), pp. 59–68.Rehm, J., Room, R., Monteiro, M., et al. (2003), ‘Alcohol as a risk factor for global burden of disease’,EuropeanAddiction Research9, pp. 157–64.Rehm, J., Mathers, C., Popova, S., et al. (2009), ‘Global burden of diseases and injury and economic costattributable to alcohol use and alcohol-use disorders’,Lancet373, pp. 2223–32.Robson, G. and Marlatt, G. A. (2006), ‘Harm reduction and alcohol policy’,International Journal of Drug Policy17, pp. 255–7.Salkeld, L. (2008), ‘Flipping madness! Police offer free flip-flops to binge drinkers who keep falling over in heels’,Daily Mail,27 November. Available at www.dailymail.co.uk/newsarticle-1089919/Flipping-madness-Police-offer-free-flip-flops-binge-drinkers-falling-heels.html (accessed 4 February 2009).Shepherd, J. (2007), ‘Preventing violence — caring for victims’,Surgeon5 (2), 114–21.Shepherd, J. P., Price, M. and Shenfine, P. (1990a), ‘Glass abuse and urban licensed premises’,Journal of theRoyal Society of Medicine83, pp. 276–7.Shepherd, J. P., Shapland, M., Pearce, N. X. and Scully, C. (1990b), ‘Pattern, severity and aetiology of injuries invictims of assault’,Journal of the Royal Society of Medicine83, pp. 75–8.Smith, D. (2008), ‘How to calm binge drinkers: get them all blowing bubbles’,Observer,30 November. Availableat: www.guardian.co.uk/society/2008/nov/30/binge-drinking-bubbles (accessed 9 February 2009).Stockwell, T. (2004), ‘Harm reduction: the drugification of alcohol policies and the alcoholisation of drugpolicies’, in Klingemann, H. and Müller, R. (eds),From science to action? 100 years later — alcohol policiesrevisited,Klewer Academic Publishers, Dordrecht, pp. 49–58.Stockwell, T. (2006), ‘Alcohol supply, demand, and harm reduction: what is the strongest cocktail?’,InternationalJournal of Drug Policy17, pp. 269–77.
300
Chapter 10: Alcohol harm reduction in Europe
Stronach, B. (2003), ‘Alcohol and harm reduction’, in Buning, E., Gorgullo, M, Melcop, A. G. and O’Hare, P.(eds),Alcohol and harm education: an innovative approach for countries in transition,Amsterdam, ICAHRE, pp.27–34.SNIPH (Swedish National Institute of Public Health) (2008),Alcohol prevention work in restaurant and medium-strength beer sales in six municipalities(English summary), Stockholm: SNIPH. Available at www.fhi.se/en/Publications/Summaries/Analysis-of-alcohol-and-drug-prevention-work-in-six-municipalities/ (accessed 28January 2009).Tagliabue, J. (1985), ‘Scandal over poisoned wine embitters village in Austria’,New York Times,2 August.Available at www.nytimes.com/1985/08/02/world/scandal-over-poisoned-wine-embitters-village-in-austria.html?sec=health (accessed 14 July 2009).Thom, B. and Bayley, M. (2007),Multi-component programmes: an approach to prevent and reduce alcohol-relatedharm,Joseph Rowntree Foundation, York.US Department of Health and Human Services (2000),10th special report to the US Congress on alcohol & health,US Department of Health and Human Services, National Institute on Alcohol and Alcoholism, Washington, DC.Warburton, A. L. and Shepherd, J. P. (2000), ‘Effectiveness of toughened glassware in terms of reducing injury inbars: a randomised controlled trial’,Injury Prevention,pp. 36–40.Wallin, E. (2004),Responsible beverage service: effects of a community action project,Karolinska Institutet,Stockholm.Wallin, E., Norström, T. and Andréasson, S. (2003a), ‘Effects of a community action project on responsiblebeverage service’,Nordic Studies on Alcohol and Drugs(English supplement) 20, pp. 97–100.Wallin, E., Norström, T. and Andréasson, S. (2003b), ‘Alcohol prevention targeting licensed premises: a study ofeffects on violence’,Journal of Studies on Alcohol64, pp. 270–7.Wallin, E., Lindewald, B. and Andréasson, S. (2004), ‘Institutionalization of a community action programtargeting licensed premises in Stockholm, Sweden’,Evaluation Review28 (5), pp. 396–419.Willis, C., Lybrand, S. and Bellamy, N. (2004), ‘Alcohol ignition interlock programmes for reducing drink drivingrecidivism’ (Review), Cochrane Database of Systematic Reviews 2004, Issue 3, Art. No.: CD004168.DOI:10.1002/14651858.CD004168.pub2.Wodak, A. (2003), ‘Foreword’, in Buning, E., Gorgullo, M., Melcop, A. G. and O’Hare, P. (eds),Alcohol andharm education: an innovative approach for countries in transition,ICAHRE, Amsterdam, pp. 1–4.WHO (World Health Organization) (1994), Lexicon of drug and alcohol terms. Available at http://www.who.int/substance_abuse/terminology/who_lexicon/en/index.html (accessed 24 June 2009).WHO (2008a),Strategies to reduce the harmful use of alcohol: report by the Secretariat to the 61st World HealthAssembly,20 March 2008, A61/13, World Health Organization, Geneva. Available at http://apps.who.int/gb/ebwha/pdf_files/A61/A61_13-en.pdf (accessed 24 June 2009).WHO (2008b),Report from a roundtable meeting with NGOS and health professionals on harmful use of alcohol,Geneva, 24 and 25 November,World Health Organization, Geneva. Available at http://www.who.int/substance_abuse/activities/msbngoreport.pdf (accessed 24 June 2009).Young, C. and Hirschfield, A. (1999),Crystal clear: reducing glass related injury. An evaluation conducted on behalfof Safer Merseyside Partnership,University of Liverpool, Liverpool.
301
Challenges andinnovations
PARTIII
Chapter 11Drug consumption facilities in Europe and beyondDagmar Hedrich, Thomas Kerr and Fran§oise Dubois-Arber
AbstractDrug consumption rooms (DCRs) are professionally supervised healthcare facilities wheredrug users can use drugs in safer and more hygienic conditions. Since 1986, more than90 DCRs have been set up in Switzerland, the Netherlands, Germany, Spain,Luxembourg, Norway, Canada and Australia. Consumption rooms aim to establishcontact with difficult-to-reach populations of drug users, provide an environment formore hygienic drug use, reduce morbidity and mortality risks associated with drug use— in particular street-based drug injecting — and promote drug users’ access to othersocial, health and drug treatment services. They also aim to reduce public drug use andimprove public amenity near urban drug markets. At times, their establishment has beencontroversial due to concerns that they may encourage drug use, delay treatment entryor aggravate problems of local drug markets. As with evaluations of other public healthinterventions, research on DCRs faces methodological challenges in taking account of theeffects of broader local policy or ecological changes. Despite these limitations, researchshows that the facilities reach their target population and provide immediateimprovements through better hygiene and safety conditions for injectors. At the sametime, the availability of safer injecting facilities does not increase levels of drug use orrisky patterns of consumption, nor does it result in higher rates of local drug acquisitioncrime. There is consistent evidence that DCR use is associated with self-reportedreductions in injecting risk behaviour such as syringe sharing, and in public drug use.Due to a lack of studies, as well as methodological problems such as isolating the effectfrom other interventions or low coverage of the risk population, evidence regarding DCRs— while encouraging — is insufficient for drawing conclusions with regard to theireffectiveness in reducing HIV or hepatitis C virus (HCV) incidence. However, use of thefacilities is associated with increased uptake of detoxification and treatment services.While there is suggestive evidence from modelling studies that they may contribute toreducing drug-related deaths at a city level where coverage is adequate, the review-levelevidence of this effect is still insufficient. Taken in sum, the available evidence does notsupport the main concerns raised about this kind of intervention and points to generallypositive impacts in terms of increasing drug users’ access to health and social care, andreducing public drug use and associated nuisance.
Keywords:injecting drug use, drug consumption rooms, safer injecting facilities, open drugscenes, public nuisance, Europe.305
Harm reduction: evidence, impacts and challenges
IntroductionDrug consumption rooms (DCRs), also called safer injecting facilities, are professionallysupervised healthcare facilities providing safer and more hygienic conditions for drug usersto take drugs (Stöver, 2000). They comprise highly targeted services within wider networks ofdrug services. While they often operate from separate areas located in existing facilities fordrug users or the homeless, some operate as stand-alone facilities.DCRs arose in specific local contexts in response to problems posed by public drug use,especially by drug injecting in streets, railway stations or staircases of residential buildings,that persisted despite the availability of a variety of drug treatment, harm reduction andsocial services, and despite law enforcement efforts to disperse or contain public drug use.The rationale for the establishment of DCRs was to address public health and communityproblems associated with specific populations of drug users, especially injectors whoconsume in public or other high-risk situations.These groups have important unmet healthcare needs and contribute to public orderproblems within local communities. A relationship between public injecting, elevated risk ofviral infections and socio-economic deprivation, especially precarious housing orhomelessness, has been long established by epidemiological research (for example, Latkinet al., 1994; Klee and Morris, 1995; Galea and Vlahov, 2002; Navarro and Leonard,2004; Corneil et al., 2006). Risk factors exogenous to the individual, including multipleinteracting physical, social and economic and policy factors, have been identified asconstituting a broader ‘risk environment’ affecting the health of injection drug users(Rhodes, 2002; Rhodes et al., 2003). Qualitative research has shown that public injectingis associated with reduced options to maintain safety and hygiene, often related to anindividual’s fear of interruption, feelings of shame and hasty injection (Small et al., 2007;Rhodes et al., 2007).DCRs aim to reduce high-risk and public drug use and to improve public amenity nearurban drug markets, by providing a hygienic and regulated environment for drug use offthe streets. They aim to create an acceptable situation for the public with regard to orderand safety concerns that arise from open drug scenes. As pragmatic ‘safer injectingenvironment’ interventions, DCRs aim to minimise the likelihood of police and publicinterference and enable individual and community risk reduction practices to occur(Rhodes et al., 2006).They further aim to reduce risk behaviour and improve health and social integration by:providing clean injecting equipment (needles, syringes, spoons, filters, wipes), good light,clean surfaces and sharps disposal; facilitating individually tailored health education, andpromoting access to healthcare and drug treatment. House rules prohibit violent andthreatening behaviour, alcohol use at the premises, drug dealing and the sharing of drugsand any injecting equipment, and define requirements regarding hygiene and injectingbehaviour. Staff are trained to provide assistance and emergency care in cases of overdose306
Chapter 11: Drug consumption facilities in Europe and beyond
or other adverse events but do not assist clients to inject (see Dolan et al., 2000; Kimber etal., 2005; Hedrich, 2004).The first legally sanctioned DCR was established in Berne, Switzerland in 1986 (Hämmig,1992). During the 1990s DCRs were set up in other Swiss cities, the Netherlands andGermany; and from 2000 they were set up in Spain, Norway, Luxembourg, Australia(Sydney) and Canada (Vancouver) (Stöver, 1991; Klee, 1991; Eastus, 2000; Zurhold et al.,2001; Parliament of New South Wales, 1998; Health Canada, 2002). By the beginning of2009 there were 92 operational DCRs in 61 cities, including in 16 cities in Germany, 30 citiesin the Netherlands and 8 cities in Switzerland.In Europe, most DCRs are integrated components of local service networks offering a rangeof social and health services. In Norway, and in Sydney and Vancouver, they are scientificpilot projects, operating under legal exemptions, which focus on supervising drugconsumption and providing referral to other services (MSIC Evaluation Committee, 2001; vanBeek, 2003; Wood et al., 2003; Skretting and Olsen, 2008). While most target druginjectors, some cater for heroin and crack smokers (Willen, 2002; Spreyermann and Willen,2003; Simmedinger and Vogt, 2008). In all cases, the drugs used are pre-obtained andprepared by the clients.With objectives in public health and public order, DCRs operate within a triangle ofindividual and public health interests and the public order interests of local communities(Stöver, 2002). More than many other public services, they rely on acceptance by a widerange of key actors: drug users, communities, other health and social agencies, police andpoliticians.The establishment of drug consumption rooms has led to some controversy anddisagreement between the International Narcotics Control Board (INCB) and some UNMember States. This has centred on the interpretation of the international DrugConventions, in particular in relation to the basic provision of the Conventions obligingStates to limit the use of narcotic drugs strictly to medical and scientific purposes (INCB,2008, p. 111).This chapter does not address this debate; nor does it comment on the position ofconsumption rooms in respect of international drug control treaties. Its purpose is tosummarise available evidence on the processes, outcomes and risks of DCRs, and also toidentify key challenges for their development as mechanisms of harm reduction. Ourreview is structured according to the objectives of DCRs, as outlined in Table 11.1. Thebalance of priorities attributed to DCRs varies, with some placing greater emphasis onhealth goals, and others on public order. The main concerns expressed regarding theestablishment of DCRs is that such facilities may promote initiation to drug injecting,conflict with treatment goals by encouraging users to continue injecting rather than entertreatment, and increase local drug dealing and drug-related crime by attracting usersfrom other areas.307
Harm reduction: evidence, impacts and challenges
Table 11.1:Aims and objectives of drug consumption roomsAims1. Provide anenvironment for saferdrug use
Outcome objectivesa) Reach and be accepted bytarget groupsb) Gain acceptabilityc) Establish conditions for safe,hygienic use
IndicatorsClient profiles, service usepatterns, client satisfactionResponses of local residents,businesses, police, politiciansVarious process indicatorsStreet drug use, risk awareness,injection hygiene, borrowing/lendingInjection injuries, infectiousdisease transmissionOverdose outcomesTreatment referral/uptakeSelf-reported rates of publicinjecting, ethnographicobservations of the burden ofpublic injectingPerceived nuisance, discardedsyringesCrime statistics
2. Improve health statusof target group
a) Improve risk-relatedbehavioursb) Reduce morbidityc) Reduce mortalityd) Improve access to healthcareand drug treatment
3. Reduce publicdisorder
a) Reduce public drug use
b) Improve public perceptionsc) No increases in localdrug-related crime
MethodsExperimental study designs, and in particular the randomised controlled trial, are consideredthe gold standard for the generation of scientific level-1 evidence about the effects oftreatments (Ashcroft et al., 1997). Maher and Salmon (2007) discuss this imperative withregard to the evaluation of the outcomes of DCRs, and conclude that ‘the scientific, practicaland ethical issues involved in applying this methodology to evaluating [such] complex publichealth interventions (…) mean that the likelihood of obtaining this level of evidence isnegligible’ (Maher and Salmon, 2007, p. 351f). To inform public health decision-making, theauthors recommend the use of prospective observational studies (level 2 evidence) as afeasible alternative (Maher and Salmon, 2007).There have been relatively few rigorous evaluations of DCRs, with evidence reviews relyingprimarily on analyses of descriptive data, cross-sectional survey data, and ecologicalindicators from a larger number of less sophisticated studies. This is especially the case inEurope, where DCRs emerged as a local service response with questions of evaluation arisingsubsequently. However, the Sydney and Vancouver facilities were established as scientificpilot studies, and thus incorporated more rigorous research designs (see below). TheVancouver study is so far the only DCR evaluation to have used an elaborate prospectivecohort-based design (Wood et al., 2004a; Wood et al., 2006b).308
Chapter 11: Drug consumption facilities in Europe and beyond
As with any health service evaluation, a key methodological challenge is to establish causality.It is difficult to attribute observed effects to DCRs since: (a) most users use these facilities only forsome consumption episodes and may otherwise continue to engage in risk behaviour (Dubois-Arber et al., 2008a); and (b) other factors (typically unmeasured) in the local environmentinfluence levels of risk behaviour and public drug use, including policy or ecological changessuch as those related to availability of substitution treatment and other harm reduction services,and changes in police operations or in the drug market (Maher and Dixon, 1999; Fischer et al.,2002; Hall and Kimber, 2005). If, as in the case of evaluating syringe exchange programmes,DCRs do succeed in attracting higher risk clients, then controlling for selection bias poses afurther challenge (Wood et al., 2007a; Schechter et al., 1999).Cross-sectional studies have limitations regarding their interpretation, as they provide a‘snapshot’ of the outcome and the characteristics associated with it at a specific point in time(Bland, 2001). Repeated cross-sectional studies can be useful for tracking trends over time(see an example in box on p. 317).The level to which coverage of the most risky consumptions can be achieved plays animportant role in whether any impact of DCRs can be detected at community level (Kimber etal., 2008a). For instance, in Frankfurt, in 1994 and 1995, the capacity of three DCRs with 22places and a total of 100 coordinated opening hours per week was insufficient to cover thedemand of 300 to 400 highly problematic street injectors out of an estimated population of6 000 to 8 000 drug users (Kemmesies, 1995). From 1996, when a fourth facility provided13 additional places, opening hours were extended to a total of 300 per week and 4 000injections were supervised each week. It was together with other measures and interventions,including shelters, day-centres and treatment programmes, that a visible reduction of publicdrug use in the city was achieved (Hedrich, 2004).Further, population HIV (and perhaps HCV) incidence rates may be too low to identifyintervention effects. As a result, most outcomes can reliably only be observed at individual,rather than at population level.Review methodsThe available evidence on DCRs was reviewed in 2004 (Hedrich, 2004), based mainly onresearch published during the 1990s in the languages of countries where DCRs wereoperating (German, Dutch, French and Spanish), and which were relatively inaccessible tothe English-speaking world.The present chapter draws on this review, on research reports resulting from the evaluationsof a medically supervised injecting centre in Sydney (MSIC Evaluation Committee, 2003;NCHECR, 2005, 2006, 2007a, 2007b) and of a safer injecting facility in Vancouver (ExpertAdvisory Committee on Supervised Injection Site Research, 2008; BC Centre for Excellence inHIV/AIDS, 2004; Wood et al., 2006b), as well as on peer-reviewed research articles on DCRoutcomes published between 2003 and 2009, and on other recent literature reviews309
Harm reduction: evidence, impacts and challenges
(Springer, 2003; Tyndall, 2003; Independent Working Group, 2006; Kerr et al., 2007a;Fischer and Allard, 2007).Relevant English language articles were identified using Medline. Further sources, especiallyfor the non-English scientific literature, which is under-represented in Medline, were identifiedby reviewing reference lists, searching by author names, or through direct contact withresearchers in different countries.Due to their scientific relevance, it is useful to note the research designs of the Sydney andVancouver studies. The Sydney evaluation used an observational design (MSIC EvaluationCommittee, 2001). The facility database provided data for process evaluation, includingclient utilisation, referrals, overdoses, and client and staff attitudes to the service. Serial cross-sectional studies were conducted to determine impact on individual health outcomes. Usingecological data, notifications of new infections and ambulance attendances at opioid-relatedoverdose events were compared between the DCR locality and control localities. Recently, theSydney evaluation incorporated a cohort-based element in its methodology, although onlylimited data are available from this cohort (NCHECR, 2007a; Kimber et al., 2008a).The Vancouver evaluation used a prospective cohort design (Wood et al., 2004a). Arandomly selected cohort of 1 000 users of the facility was monitored on a range of healthindicators and potential impacts including risk behaviour surveys, venous blood samples toassess HIV and HCV incidence, overdose events, and health service use. For ethical reasons,participation in the research was optional, although over 95 % of those invited agreed toparticipate. The Vancouver evaluation’s greatest strength was the existence of a community-recruited cohort of over 1 500 injectors, the Vancouver Injection Drug Users Study, whichwas initially recruited in 1996–97. This cohort consisted of individuals who did and did notuse the safer injecting facility, and therefore allowed for control-based comparisons, as wellas before and after analyses. As with the Sydney evaluation, the Vancouver design alsoincluded a facility database to track all key service events (referrals, overdose, drugs used),and data from both cohort studies were linked to a range of external databases(detoxification programme databases, hospital databases).Both the Sydney and Vancouver research projects included local resident surveys, qualitativeinterviews with users, staff and key stakeholders, and standardised evaluations of publicorder changes (discarded syringes, perceived nuisance, and crime data).
FeasibilityObjective 1a: reach and be accepted by target groupIn all countries, studies have shown that the profiles of clients contacted reflect the targetgroups and that DCRs generally succeed in attracting drug users who are at high risk of HIVinfection and overdose, as well as those who are likely to inject drugs in public (Hedrich,2004; Wood et al, 2005b; Simmedinger and Vogt, 2008; Dubois-Arber et al., 2008a,Scherbaum et al., 2009). In most of the recent studies, the majority of clients are male and310
Chapter 11: Drug consumption facilities in Europe and beyond
over 30 years old with long histories of drug use. According to current data from Frankfurt,4 520 individuals used the four local DCRs at least once in 2007. These clients have anaverage age of 34 years and are characterised by a high level of unemployment (65 %).Many suffer from drug use-related infectious diseases (HCV: 53 %; HIV: 5.9 %). A majority ofDCR clients maintain regular contact with the local drug help system, and in particular makeuse of low-threshold agencies (89 %), but also of outpatient drug counselling facilities (36 %).More than half of clients (55 %) report being in medical treatment, which may include opioidmaintenance treatment (Simmedinger and Vogt, 2008). Similar sociodemographic data arereported on 10 514 service users registered during the first seven years of operation at theMedically Supervised Injecting Centre (MSIC) in Sydney: their average age is 33 years, 74 %of service users are men, 61 % live mainly on social welfare benefits, and 24 % are homeless(van Beek, 2007). A comparison of socio-demographic profiles of DRC users in Zürichbetween 1997 and 2007 shows that current user populations are on average about adecade older, have an improved housing situation (6.7 % homeless in 2007, compared to13.8 % in 1997), and commit fewer crimes to generate income (9.4 % in 2007, compared to30 % in 1997) (Gautschi et al., 2008).Retention and attendance rates at the Vancouver DCR also indicate that the facility issuccessful in gaining acceptance by its target group and that regular users of DCRs tend tobe more marginalised, with various health and social problems, such as those related tounstable housing and public injecting (Wood et al., 2005b; Wood et al., 2006a). Clientsurveys conducted at several facilities also show high levels of satisfaction with staff and theservices provided, as well as criticism of aspects such as opening hours (Benninghoff andDubois-Arber, 2002; Poschadel et al., 2003; NCHECR, 2005, 2007b; Petrar et al., 2007).Objective 1b: gain acceptabilitySurveys and qualitative research on residents, local businesses, police and other key actorsshow mixed reactions to DCRs. On balance they are generally accepted by communities,albeit with reservations. Although some police tend to be more sceptical (Zurhold et al.,2003; Benninghoff et al., 2003; Zobel et al., 2003; BC Centre for Excellence in HIV/AIDS,2004), there is also evidence that police in some settings are accepting of DCRs and activelyrefer drug users to them (DeBeck et al., 2008).Objective 1c: establish conditions for safe, hygienic consumptionProcess evaluations indicate that DCRs provide hygienic facilities, sterile injecting equipment,professional staffing and supervision, entrance criteria, safety rules, emergency procedures,safer injecting instruction and health education (Ronco et al., 1996a, 1996b; Linssen et al.,2001; Zurhold et al., 2001; Wolf et al., 2003; and Zobel and Dubois-Arber, 2004; Kimber etal., 2005). Studies also indicate that hygiene and safety are important reasons why clientsuse the facilities (Poschadel et al., 2003; Benninghoff et al., 2003). Despite millions ofinjections occurring at DCRs over the past 20 years, there have been no reported overdosefatalities (Poschadel et al., 2003; NCHECR, 2007b; Milloy et al., 2008; Expert AdvisoryCommittee on Supervised Injection Site Research, 2008).311
Harm reduction: evidence, impacts and challenges
The Canadian research in particular shows that concerns that DCRs delay entry intotreatment or even promote drug use are not substantiated. There were no observableincreases nor decreases in drug use in the community, and no measurable increases in ratesof relapse into injection drug use or initiation into injection drug use (Kerr et al., 2007b),stopping injection drug use, or seeking treatment (Stoltz et al, 2007; Kerr et al., 2005,2006a; Wood et al., 2005a). Available evidence from Sydney (MSIC Evaluation Committee,2003; NCHECR, 2007b) and Europe (Ronco et al., 1996b; Poschadel et al., 2003;Benninghoff et al., 2003) points to the same ‘neutral’ effect.There are occasional reports of users making their first injection in a DCR (Benninghoff et al.,2003; Solai et al., 2005; Kerr et al., 2007b). Whether these would have occurred in theabsence of the DCR is not known.Conclusions on objective 1DCRs reach and are accepted by their target populations, including marginalised street usersand those at higher risk of infectious diseases or overdose (objective 1a). They are generallyaccepted by communities and key actors, or at least tolerated as the lesser of alternative evils(objective 1b). Further, they provide conditions, especially for regular clients, that improvehygiene and reduce exposure to health risks such as infectious diseases or overdoses(objective 1c). The risk that some users initiate injecting at DCRs is low and there is noevidence they increase levels of drug use or risky patterns of consumption. On the basis ofavailable evidence, consumption rooms achieve their immediate objective of providing anenvironment away from the streets where high-risk or public drug users can consume theirdrugs more safely and hygienically, and they don’t encourage drug use or injecting.
Impact on health outcomesObjective 2a: reduce risk behavioursThe European Report on DCRs (Hedrich, 2004) identified 12 studies and one review of the impactof DCRs in the Netherlands, Germany and Switzerland on risk behaviours. Although subject tovarious methodological limitations, all European studies indicated positive effects. Staff also reportpositive changes in many clients’ injecting hygiene. For example, several pre-post studies in theNetherlands showed increased knowledge of injecting hygiene and safer drug use among DCRusers (Meijer et al., 2001; Linssen et al., 2001); cross-sectional surveys in Germany and in theNetherlands showed self-reported improvements by large proportions of DCR clients in injecting-related risk behaviour, injecting practices and hygiene since using a DCR (Jacob et al., 1999;Poschadel et al., 2003; van der Poel et al., 2003; Zurhold et al., 2001). Serial cross-sectionalsurveys in Switzerland showed decreases in the proportion of DCR clients reporting syringesharing and sharing of other injecting equipment (Benninghoff et al., 2001, 2003; Benninghoffand Dubois-Arber, 2002; Solai et al., 2004) as well as increases in the proportion saying theywould never accept used injecting equipment (Minder Nejedly and Bürki, 1999; Reyes Fuentes,2003; Ronco et al., 1996a, 1996b). These earlier findings have been confirmed by Dubois-Arberet al., 2008b and by a more recent study from Spain that also reports reduced borrowing of usedsyringes among highly marginalised injecting drug users attending DCRs (Bravo et al., 2009).312
Chapter 11: Drug consumption facilities in Europe and beyond
Backstreet where public drug use takes place, Vancouver
Safer injecting facility, Vancouver
Source:M. J. Milloy for both photographs.
313
Harm reduction: evidence, impacts and challenges
Outside Europe, these results have been replicated by studies in Sydney, where DCR clientswere more likely than non-DCR clients to report using sterile syringes for all injections andless likely to report sharing injecting equipment, and where staff also reported improvedhygiene and reduced sharing among DCR clients (MISC Evaluation Committee, 2003;NCHECR 2007a, 2007b). Likewise in Vancouver, a prospective cohort study of injecting drugusers (IDUs) showed that syringe sharing decreased among DCR users but not among non-users of DCRs after the facility opened, and that the degree of reduction was associated withgreater use of the facility (Kerr et al., 2005; Wood et al, 2005a; Stoltz et al., 2007). A recentmeta-analysis shows highly similar effects of DCRs on the extent of syringe sharing acrosssites, with frequent DCR use being associated with a 70 % reduced likelihood of reportingsyringe sharing (Milloy and Wood, 2009).Collectively, these studies provide clear evidence that DCR use is associated with reducedself-reported and observed injecting risk behaviour, including the risk of overdose, andimprovements in reported and observed injecting hygiene, especially among those who usethe facilities consistently.
Objective 2b: reduce morbidityFew studies report on injection-related injuries, although such injuries may represent asignificant source of morbidity among people who inject drugs (Palepu et al., 2001;Salmon et al., 2009a). In Sydney, a small decrease in the frequency of injection-relatedproblems over time was observed among DCR clients, including less bruising, scarringand abscesses (NCHECR, 2007b). In Vancouver, the risk of injecting-related bacterialinfections decreased among DCR users, and the use of the facility was independentlyassociated with other safe injection practices, including decreased reuse of syringes,increased use of sterile water and increased cleaning of injection sites with alcoholswabs (Stoltz et al., 2007). There is further evidence from qualitative studies undertakenin Vancouver of the potential impact of DCRs on reducing the incidence of soft tissueinfections (Small et al., 2008; Krüsi et al., 2009) and of the advantages of nurse-delivered safer injection education in reaching IDUs most at risk for injection-relatedharm (Wood et al., 2008; Lloyd-Smith et al., 2009).No conclusions can be drawn about the direct impact of DCRs on infectious diseaseincidence, owing to a lack of studies as well as methodological problems, such as isolatingthe effect of DCRs from other interventions (substitution treatment, needle exchange,outreach), low rates of HIV/HCV incidence, or low coverage of the risk population. Forexample, in Sydney, health authorities were notified of fewer newly diagnosed HCV, HIV andHBV infections in the DCRs’ locality compared to other control localities (MSIC EvaluationCommittee, 2003). However, no evidence was found that any changes in the number ofnotified cases were attributable to the DCR. Furthermore, the low incidence of HCV and HIVamong IDUs in Australia made it unlikely that the number of cases would be sufficient todetect any statistically significant associations. Limited coverage of the facility was alsounlikely to produce a detectable community impact on incidence.314
Chapter 11: Drug consumption facilities in Europe and beyond
Objective 2c: reduce mortality (overdoses)There is some evidence of the impact of DCRs on mortality, but this evidence is mostly indirectand based on the outcome of emergencies occurring in the facilities (see box on p. 144). Themajority of emergencies among users of DCRs involve heroin injection-related overdoses,with smaller proportions involving cocaine use. Emergency rates vary from 0.5 to 7 per1 000 injections (see Hedrich, 2004, for Germany, Netherlands, Switzerland and Spain; Kerret al., 2006b, for Vancouver; NCHECR, 2007b, for Syndey; and Skretting and Olsen, 2008,for Norway). As rapid intervention is available at DCRs, these events are less severe thanoverdoses occurring elsewhere, and fewer ambulance attendances or hospitalisations areneeded (NCHCR, 2007b). In addition, DCRs located near open drug scenes may respond tooverdoses in the immediate vicinity (Hedrich, 2004). None of the overdoses recorded atDCRs have resulted in death (the only known death at a DCR involved anaphylactic shock).Furthermore, by providing immediate intervention following the first signs of overdose, otherimpacts of non-fatal overdose-related events, including irreversible damage to the brain andother vital organs due to hypoxia, can also be prevented (van Beek et al., 2004; Hämmigand van Beek, 2005; NCHECR, 2007b).Apart from potential fatalities prevented through supervised consumption among clients,there are several estimates of the impact of DCRs on drug deaths at population or citylevel. Based on utilisation data and expected mortality rates among the populationsreached by DCRs, it has been estimated that these facilities helped prevent 10 deaths peryear in Germany, and four per year in Sydney (Hedrich, 2004; MSIC EvaluationCommittee, 2003). In a comparison of overdose death trends in the vicinity of the DCR withthe rest of the region of New South Wales, no statistically significant impact of the Sydneyfacility on opioid-related deaths in Kings Cross was found. Due to an approximate 70 %decrease in overdose deaths following a heroin shortage in Australia, the researchersargue that the assessment of the impact may have been hampered by small sample sizes(NCHECR, 2007b, p. 29). In their simulation of the impact of the Vancouver DCR, Milloyand colleagues (2008) concluded that the facility may have prevented between 1.9 and11.7 overdose deaths per year.An ecologically based time-series analysis involving four German cities from 1990–2001concluded that statistically significantly reductions in overdose fatalities were observed inSaarbrücken and Hannover six months after the opening of the DCR, and in Hamburg andFrankfurt after the opening of the third and fourth rooms respectively (Poschadel et al.,2003).While it is impossible to ascertain how many emergencies would have occurred and beenfatal in the absence of DCRs, epidemiological and clinical data suggest that immediate staffinterventions at emergencies occurring at DCRs, where millions of drug consumptions havetaken place under supervision, has reduced the impact of overdose-related events, such asmorbidity and death. Where coverage and capacity are sufficient and opening hoursappropriate, DCRs may contribute to reducing drug-related deaths at a city level.315
Harm reduction: evidence, impacts and challenges
Objective 2d: improve access to healthcare and drug treatmentThere are large variations between countries regarding services offered on-site, which makecomparisons difficult. Different policies towards accepting clients who are already insubstitution treatment also affect treatment referral rates. Regarding referrals to treatment,only the Vancouver and Sydney studies measure actual uptake.In most European DCRs a range of other services are usually delivered on-site alongsidesupervision of drug consumption. Low-threshold medical care and psychosocial counsellingservices are especially well used and contribute to the stabilisation and improvement of thesomatic and psychological health of users (Linssen et al., 2001; Poschadel et al., 2003;Zurhold et al., 2001; van der Poel et al., 2003; Ronco et al., 1994). Clients are also referredto drug treatment or other care, though proportions vary and uptake rates are oftenunknown. For instance, in the survey of all German consumption rooms, over half of allclients reported having received a referral by DCR staff to other drug or social services atleast once (Poschadel et al., 2003).In both Vancouver and Sydney, use of the facility was associated with more exposure to safeinjecting education and access to healthcare (Wood et al., 2006a, 2007b; van Beek, 2003;Tyndall et al., 2006; NCHECR, 2007a, 2007b; Kimber et al., 2008b). In Vancouver, a 30 %increased uptake of detoxification and subsequent addiction treatment were noted. Forfrequent attenders in particular, DCRs act as a link to the wider system of healthcare andfacilitate entry to treatment: in Vancouver, entering a detoxification programme was morelikely among IDUs who visited the facility at least weekly and among those who had contactwith onsite addiction counsellors (Wood et al., 2007b).The above results suggest that DCRs complement rather than conflict with treatment goals. Infact, with the exception of the initial years of DCR operation, current typical client populationsat DCRs are in (or have successfully been brought into) contact with other harm reductionand treatment services, and many oscillate between those, or make parallel use of them. Thisreflects the complementary role of DCRs within a comprehensive drug policy approach, suchas in Switzerland, where long-term behavioural trends and health-related impacts aredocumented (see box on p. 317).Studies assessing the effectiveness of treatment consistently show that opioid maintenancetreatment reduces the level of illicit opiate use and the frequency of injecting. Drug use andinjecting may, however, still occur among clients in opioid maintenance, and clients intreatment may also use DCR facilities. For instance, during the first seven years of operationof the MSIC in Sydney, 13 % of all clients registering at the facility indicated that they were inmethadone treatment (van Beek, 2007). Data from the first year of operation of the DCR inGeneva (2002) show that a majority (61.1 %) of users declared at the time of enrolment thatthey were in substitution treatment (Dubois-Arber, 2008a).The question of whether clients in oral methadone treatment should use DCRs for injection isdealt with in different ways. In Germany, and Luxembourg, methadone clients are formallyexcluded from most consumption rooms. Elsewhere, however, the pragmatic view is taken
316
Chapter 11: Drug consumption facilities in Europe and beyond
that if methadone clients are going to inject anyway it is better that they do so in hygieniccircumstances where there is also the opportunity for staff to talk with them.
Long-term behavioural trends and health-related impact of harm reduction facilities,including DCRs (Switzerland)In 1993, 1994, 1996, 2000 and 2006 repeated national cross-sectional surveys wereconducted among IDUs attending facilities that offer needle and syringe programmes, inorder to measure trends in injecting behaviour (Dubois-Arber et al., 2008b). In 2006, half ofthese facilities (n=11) included a DCR.Between 1993 and 2006, current injecting — in the last six months — decreased among thosewho had ever injected from 95.1 % to 74.2 %. The median number of injections in the last weekalso decreased from 14 to 7. The proportion of new injectors (first injection in the last two years)decreased from 18.7 % to 3.3 %. In 2006, most injecting events took place at home (56.4 %) orin a DCR (32.8 %). The type of drugs consumed in the last month showed a reduction in heroin,from 60.5 % of users in 1993 to 43.1 % in 2006, but an increase in cocaine users, from 23.7 %to 63.5 %. This may partly be related to an increasing proportion of IDUs on methadone treatmentamong the clients: 37.2 % in 1993, and 59.1 % in 2006. In 2006, about 10 % of IDUs hadinjected with a borrowed syringe in the last six months. This proportion has been quite stable since1994, after a decrease between 1993 and 1994. Although more common, sharing of otherinjection equipment — spoons, filters and water — has decreased since 1996. Behavioural trendsdid not differ between IDUs recruited in facilities with or without a DCR.During the same period (1993–2006), the national monitoring of injecting equipment showeda decrease from 2.2 millions to 1.6 million in syringes delivered in NSPs. New cases of HIVreported among IDUs decreased from 498 to 61, and notified acute cases of hepatitis C from37 to 33. The number of IDUs receiving methadone treatment increased from around 12 000to around 17 000, and drug-related deaths decreased from 353 to 193 (Gervasoni andDubois-Arber, 2009).This overall evolution cannot be attributed exclusively to the availability of NSPs and DCRs.However, it is posited that DCRs have contributed to the improvement in IDUs’ health inSwitzerland.
Conclusions on objective 2DCRs help to improve the health status of the target population and contribute toreductions in high-risk injecting behaviour. There is evidence that when coverage andcapacity are adequate, DCRs help to reduce overdose deaths. Available evidence doesnot allow conclusions to be drawn on whether or not they have specific, attributableimpact on HIV and HCV infection rates, although fairly substantial reductions in HIV andHCV risk behaviour have been associated with DCR use. DCRs do increase access forspecific ‘hard-to reach’ target populations of drug users to health, welfare and drugtreatment services.317
Harm reduction: evidence, impacts and challenges
Impact on public order and crime outcomesObjective 3a: reduce public drug useDirect evidence of the impact of DCRs on levels of public drug use is limited and sometimesmixed. This is because of methodological limitations, restricted coverage, the difficulty ofknowing how many facility-based injections would otherwise have occurred in public, andbecause other factors, such as police activity or changes in the drug market, also affectpublic drug use.Studies in the Netherlands, Germany, Switzerland, Sydney and Vancouver showed lower levelsof self-reported public drug use among clients (van der Poel et al., 2003; Zurhold et al., 2001;Poschadel et al., 2003; Benninghoff and Dubois-Arber, 2002; Stoltz et al., 2007; NCHECR,2007b). However, it was not always possible to attribute this effect to DCRs (Zobel and Dubois-Arber, 2004). In Vancouver, the opening of the DCR was associated with a reduction of publicinjection, discarded syringes and drug-related litter (Wood et al., 2006a). In this instance, theseeffects were found independently of changes in police presence and weather patterns. InSydney there was a reduction in public drug use among regular clients and reduced communityvisibility of injecting drug use (NCHECR, 2007b; Kimber et al., 2008b).Among those who attended DCRs some report that they also continued to take their drugs inpublic places, when the DCR had insufficient space, was located away from drug purchasesites or when opening hours were restricted (Zurhold et al., 2001, 2003; Poschadel et al.,2003). Public injecting in some DCR localities may increase as a result of police actions toreduce drug markets in other areas (Benninghoff et al., 2003; Poschadel et al., 2003;Hedrich, 2004).Objective 3b: improve public perceptionsEvidence related to public perceptions is also mixed. Several German, Swiss and Dutchstudies have reported mostly acceptance of DCRs, at least as a preferable option to publicuse (Linssen et al., 2001; Zurhold et al., 2003; Zobel et al., 2003). In Vancouver, a surveyamong a random sample of 117 business owners located in the vicinity of the DCR found that54 (46 %) were in favour of having a DCR, 23 were undecided and 40 were opposed to it.Businesses located further away from the facility showed less support (BC Centre forExcellence in HIV/AIDS, 2004). A five-year evaluation of the community perceptions of drug-related amenity before (year 2000) and after the opening of the Sydney DCR (surveysconducted in 2002 and 2005) among local residents and businesses found a significantdecrease over time of those who reported recently witnessing public injection and improperlydiscarded syringes (Salmon et al., 2007) and that community attitudes tended to becomemore positive over time (Thein et al., 2005; MSIC Evaluation Committee, 2003). However,attributing these improvements to the DCR was complicated by a concurrent heroin shortageand rise in stimulant use. In Germany and Switzerland some DCRs have encountered strongopposition from local residents, which diminished with experience of the DCR in operation.Generally, fewer nuisance problems are reported in cities where a political consensus orcooperation between police and drugs services exists (Hedrich, 2004).318
Chapter 11: Drug consumption facilities in Europe and beyond
Effects on local crimeNo increase in acquisitive crime has been observed after the opening of DCRs in theNetherlands and Switzerland (Linssen et al., 2001; Meijer et al., 2001; Spreyermann andWillen, 2003; Benninghoff et al., 2003).The impact of the safer injecting facility in Vancouver on public disorder and drug-relatedcrime has been studied extensively, including through follow-up studies comparing thesituation before and after the opening of the facility (see box below). Furthermore, noevidence of negative impacts of the operation of the facility on community drug use patternshas been found (Kerr et al., 2006a).
The impact of the Vancouver DCR on crime, nuisance, safety and police referralsThe Vancouver DCR, known as ‘Insite’, is situated in a large open drug scene. The area isknown for high levels of public injecting, drug dealing, and its open sex work market. Insiteis open 18 hours a day, and includes 12 individual booths for injecting.Insite has been evaluated to assess its potential impact on public order, crime, and its potentialimpact on policing practices. An early mixed methods analysis employed field counts of thenumber of individuals injecting in public, discarded syringes and other injecting litter, over an18-week period (Wood et al., 2004c).In multivariate regression analyses, the opening of Insite was associated with reductions ineach measure of disorder after adjustment for police presence and rainfall. In two follow-up studies, use of Insite was also found to be associated with self-reported declines inpublic injecting (Stoltz et al., 2007; Petrar et al., 2007). Local crime statistics have beenused to assess a potential association between the opening of Insite and drug-relatedcrime (Wood et al., 2006c). In this before and after analysis, the opening of Insite was notassociated with increases in drug trafficking, robbery/assault, or vehicle break-in charges.A recent study also sought to assess whether local police were referring drug users to Insite(DeBeck et al., 2008). Among 1 090 DCR clients enrolled in a prospective cohort study,182 (16.7 %) individuals reported having ever been referred to the SIF by local police. Atbaseline, 22 (2.0 %) participants reported that they first learned of the SIF via police. Inmultivariate analyses, factors positively associated with being referred to the SIF by localpolice when injecting in public included engaging in sex work, daily cocaine injection,and unsafe syringe disposal. Collectively, these findings suggest that Insite has reducedpublic disorder, in particular public injecting, and has not exacerbated drug-related crime.Furthermore, Insite has provided a mechanism for police referral of individuals who engagein public injecting.
In Sydney, an evaluation of the crime statistics in the relevant neighbourhoodsdocumented that operation of the MSIC DCR did not lead to increases in crime or socialdisturbance in its immediate vicinity. There was no evidence of any positive or negativeimpact on rates of drug-related crime, drug-related loitering, and no increase in theproportion of supply offences following the opening of the MSIC (NCHECR, 2007b;Freeman et al., 2005).319
Harm reduction: evidence, impacts and challenges
Most European reports show a similar picture. However, there have been reports from a fewEuropean facilities of increases in drug dealing around the facility (Geense, 1997; Zurhold etal., 2001), as well as aggressive incidents outside the premises, increases in petty crime andresentment from local residents (Kimber et al., 2005).Conclusions on public order and crime outcomesConsumption rooms can reduce the level of drug use in public. The extent to which this isachieved depends on their accessibility, opening hours and capacity. There is no evidencethat the operation of consumption rooms leads to more acquisitive crime. There is small-scaledrug dealing in the vicinity of many services, which is not surprising given their location.Nuisance is more likely when capacity or location of the facility does not meet local needsand waiting times are long. In some instances, these problems can be addressed by anadjustment of service capacity, aided by police cooperation and the involvement of the DCRin local order maintenance. However, facilities near illicit drug markets are not able to solvewider nuisance problems that result from these markets. Consumption rooms have greaterimpact where there is a political consensus that they are part of a comprehensive localstrategy to respond to drug use-related problems that acknowledges public and individualhealth objectives as well as the need to maintain an acceptable situation with regard to orderand safety in the community.
ChallengesThe evidence reviewed in this chapter indicates that DCRs may contribute to reducing drug-related harms in settings where public drug use and injecting pose serious public health andsocial problems. For the future, these types of interventions face a number of challenges. Thefirst set of challenges arises from changing patterns of drug use and drug using contexts andthe new configurations of harms that these may imply. The second set of challenges concernscreating the environmental conditions that enable the reach and impact of existing DCRs andthe development of new projects where there is a demonstrated need.Targeting interventions in a changing world of drug useChanging drug use situations present challenges for harm reduction interventions, calling forthe capacity of responses to adapt rapidly to shifts in drug use, risks, target groups andneeds (see also Hartnoll et al., 2010). Such changes may impact on: the prevalence orfrequency of injecting; modes of drug administration (such as inhaling or smoking); patternsof drug use (for example, the injecting of crack cocaine, cocaine or amphetamine, or‘speedball’); and risk environments.Operational data collected at European DCRs shows that there is a cumulative ‘revolvingdoor’ client group of ageing injectors (Simmedinger and Vogt, 2008), but also that thereare new groups of service users, in some cases young, for whom differentiated responsesregarding safer use education are needed (Sozialdepartement der Stadt Zürich, 2008).320
Chapter 11: Drug consumption facilities in Europe and beyond
Additionally, increases in cocaine injecting observed in several European countries(EMCDDA, 2009) may imply increased frequency of injecting and associated healthharms, including vein damage, bacterial and viral infections (see also Grund et al., 2010).The use of DCRs by clients in opioid maintenance treatment may also point to ineffectivetreatment regimes or to clients for whom methadone is unsuitable. In one case, a smallsubgroup (4 % of DCR clients) who mainly injected cocaine, were among the mostfrequent users of the facility, accounting for almost two-fifths of all injections observed inthe year of study (2002) (Dubois-Arber et al., 2008a). Most of this group (65 %) were inmethadone treatment at the time they had registered at the facility. Differentiatedintervention emphasis should therefore be tailored to different and changing client needs,including through integrating referral and service delivery as part of a wider local systemresponse to drug treatment and care (Dubois-Arber et al., 2008a). Studies also show thatfrequent DCR users may use the room as a place of socialisation and support(Benninghoff et al., 2003).Most DCRs target drug injectors, with the exception of the Netherlands, where themajority of places are for smoking, reflecting the low proportion of injectors in theproblem drug use population. Limited facilities for smoking have been added to someDCRs in Germany and Switzerland, and a room has been opened specifically for crackusers in Frankfurt and for heroin smokers in Hamburg. Although smoking is generallyseen as less risky than injecting, there may still be health risks, for example of transmittingHCV through sharing crack smoking paraphernalia (Fischer et al., 2008; Macías et al.,2008; Neaigus et al., 2007; Grund et al., 2010), as well as problems associated withpublic drug use. The expected benefits of implementing facilities for smoking at DCRsinclude contact with recent or younger users with the possibility of facilitating earlytreatment and reducing the risk of HCV infection.Given the increased prevalence of both heroin smoking and the use of crack cocaine in anumber of EU countries, assessment of the advantages and disadvantages of providingfacilities for non-injectors, and the manner in which such services are best delivered meritsfurther research.The examples given above suggest that DCRs can play a wider and more proactive rolethan originally envisaged, in particular with regard to transmitting tailored healtheducation messages to individual clients and to developing realistic prevention and saferuse messages for the wider population of problem drug users. Because DCRs are for mostclients not the main place of drug use (Dubois-Arber et al., 2008a; MSIC EvaluationCommittee, 2003; Hedrich, 2004), learning to consume drugs safely in other contexts isan important individual outcome to be achieved. From this perspective, DCRs could be abasis from which to extend peer education and community-oriented projects to modifylocal risk environments (Pretil, 2007). In this regard, as frontline services, DCRs have thepotential to constitute a sensitive and timely early warning system about drug use trendsand effects of market changes (Degenhardt et al., 2008); they can help to gain in-depthknowledge of risky drug use practices and risk-increasing aspects of the local environment(Salmon et al., 2009a; 2009b).321
Harm reduction: evidence, impacts and challenges
Creating an enabling environment for interventionWhere DCRs are ‘normative’ as part of established harm reduction policy (Switzerland,Germany, the Netherlands, Luxembourg, Norway, parts of Spain), they are likely to continueand evolve. In this situation they face the challenges outlined above. In other countries, thesituation is different. In some, there is a polarisation of public debate leading to the rejectionof proposals, in others there is ambivalence resulting in a deadlock of new initiatives. Therole of DCRs in the future has to be seen in the context of developments regarding publicdrug use and accessibility, as well as quality of drug treatment, including the existence of realreintegration options, funding and sustained political commitment.If DCRs are to have an impact at community level it is necessary to provide sufficientcapacity relative to the estimated size of the target population, to locate rooms on sites thatare easily accessible, and to ensure that opening hours are long enough to meet demand,especially in the evenings and on weekends. Staffing and modus operandi are alsoimportant. Assessing the cost-effectiveness and impact of different service models atdifferent levels of population coverage in different epidemiological settings is a keyresearch question for the future.In settings where there is a demonstrable need for DCRs, their development and the extent towhich they can achieve their objectives is tempered by the broader social and policy context.A qualitative assessment of the literature suggests that DCRs can only be effective if they are:• ntegrated into a wider public policy framework as part of a network of services aiming to ireduce individual and social harms arising from problem drug use;• ased on consensus, support and active cooperation among key local actors, especially bhealth, police, local authorities, local communities and consumers themselves;• een for what they are — specific services aiming to reduce problems of health and social sharm involving particular high-risk populations of problematic drug users and addressingneeds that other responses have failed to meet.
ConclusionThis chapter has focused on scientific evidence regarding whether DCRs, as a specificintervention, have achieved their stated objectives. Despite some limitations of the availableevidence, the broad conclusion is that DCRs do bring benefits on specific aspects ofindividual and public health and social order without incurring serious risks. To achievethis, adequate coverage is essential, as is political support and consensus between keyactors.Expectations towards DCRs thus need to be realistic, as they cannot address all the keyvariables of drug-related harms. They do not change the fact that users buy their drugsin illicit markets, nor can they aim to change the drug market itself. They are, however,an effective public health intervention providing a ‘safer environment’ to reduce risksinherent in public drug use; they are unique in their capacity to develop individually322
Chapter 11: Drug consumption facilities in Europe and beyond
tailored health education that achieves sustainable behavioural change among the mostvulnerable populations; and the facilities provide clear benefits by increasing drug users’access to health and social care, and in reducing public drug use and associatednuisance.
DCRs — implications for practiceDrug consumption rooms can only be effective if they are:• ntegrated into a wider public policy framework as part of a network of services aiming to ireduce individual and social harms arising from problem drug use;• ased on consensus, support and active cooperation among key local actors, especially bhealth, police, local authorities, local communities and consumers themselves;• een for what they are — specific services aiming to reduce problems of health and social sharm involving particular high-risk populations of problematic drug users and addressingneeds that other responses have failed to meet.
ReferencesAshcroft, R. E., Chadwick, D. W., Clark, S. R. L., et al. (1997), ‘Implications of socio-cultural contexts for theethics of clinical trials’,Health Technology AssessmentI (9). Available at http://www.hta.ac.uk/project/htapubs.asp (accessed 23 October 2009).BC Centre for Excellence in HIV/AIDS (2004),Evaluation of the supervised injection site: year one summary,BCCentre for Excellence in HIV/AIDS, Vancouver. Available at http://www.vch.ca/sis/docs/sis_year_one_sept16.pdf (accessed 3 June 2009).Benninghoff, F. and Dubois-Arber, F. (2002),Résultats de l’étude de la clientèle du Cactus BIEL/BIENNE 2001,Institutuniversitaire de médecine sociale et préventive, Lausanne.Benninghoff, F., Geense, R. and Dubois-Arber, F. (2001),Resultats de l’étude ‘La clientèle des structures à bas seuild’accessibilité en Suisse’,Institut universitaire de médecine sociale et préventive, Lausanne.Benninghoff, F., Solai, S., Huissoud, T. and Dubois-Arber, F. (2003),Evaluation de Quai 9 ‘Espace d’acceuil etd’injection’ à Genéve: période 12/2001–12/2000, Raisons de santé 103,Institut universitaire de médecine sociale etpréventive, Lausanne.Bland, M. (2001),An introduction to medical statistics,3rd edition, Oxford University Press, Oxford.Bravo, M. J., Royuela, L., De la Fuente, L., et al. (2009), ‘Use of supervised injection facilities and injection riskbehaviours among young drug injectors’,Addiction104 (4), pp. 6124–9.Corneil, T. A., Kuyper L. M., Shoveller, J., et al. (2006), ‘Unstable housing, associated risk behaviour, andincreased risk for HIV among injection drug users’,Health Place12, pp. 79–85.
323
Harm reduction: evidence, impacts and challenges
DeBeck, K., Wood, E., Zhang, R., Tyndall, M., Montaner, J. and Kerr, T. (2008), ‘Police and public healthpartnerships: evidence from the evaluation of Vancouver’s supervised injection facility’,Substance AbuseTreatment Prevention Policy7 May, 3, p. 11 (DOI:10.1186/1747-597X-3-11).Degenhardt, L., Roxburgh, A., van Beek, I., et al. (2008), ‘The effects of the market withdrawal of temazepam gelcapsules on benzodiazepine injecting in Sydney, Australia’,Drug and Alcohol Review27 (2), pp. 145–51.Dolan, K., Kimber, J., Fry, C., et al. (2000), ‘Drug consumption facilities in Europe and the establishment ofsupervised injecting centers in Australia’,Drug and Alcohol Review — Harm Reduction Digest10 (19), pp. 337–46.Dubois-Arber, F., Benninghoff, F. and Jeannin, A. (2008a), ‘Typology of injection profiles of clients of asupervised drug consumption facility in Geneva, Switzerland’,European Addiction Research14, pp. 1–10.Dubois-Arber, F., Balthasar, H., Huissoud, T., et al. (2008b), ‘Trends in drug consumption and risk of transmissionof HIV and hepatitis C virus among injecting drug users in Switzerland, 1993–2006’,Eurosurveillance22 May,13 (21).Eastus, C. (2000), ‘Die Entwicklung von Gesundheitsräumen in der Schweiz’,Akzeptanz -Zeitschrift fürakzeptierende Drogenarbeit und humane Drogenpolitik8 (1), pp. 10–12.EMCDDA (2009),Annual report on the state of the drugs problem in the European Union, 2009,EuropeanMonitoring Centre for Drugs and Drug Addiction, Lisbon.Expert Advisory Committee on Supervised Injection Site Research (2008),Vancouver’s Insite service and othersupervised injection sites: what has been learned from the research? Final report, 31 March 2008,Health Canada,Ottawa, Ontario. Available at http://www.hc-sc.gc.ca/ahc-asc/pubs/_sites-lieux/insite/index-eng.php (accessed3 June 2009).Fischer, B. and Allard, C. (2007),Feasibility study on ‘supervised drug consumption’ options in the City of Victoria,Centre for Addictions Research of British Columbia (CARBC), University of Victoria, Victoria. Available at http://www.viha.ca/NR/rdonlyres/9C3846B7-4836-4F1C-8CE2-952273E3A439/0/carbc_feasibility_study.pdf(accessed 15 January 2010).Fischer, B., Rehm, J., Kim, G. and Robins, A. (2002), ‘Safer injecting facilities (SIFs) for injection drug users (IDUs)in Canada: a review and call for an evidence-focused pilot trial’,Canadian Journal of Public Health93 (5), pp.336–8.Fischer, B., Powis, J., Firestone Cruz, M., Rudzinski, K. and Rehm, J. (2008), ‘Hepatitis C virus transmission amongoral crack users: viral detection on crack paraphernalia’,European Journal of Gastroenterology & HepatologyJanuary, 20 (1), pp. 29–32.Freeman, K., Jones, C. G., Weatherburn, D. J., et al. (2005), ‘The impact of the Sydney MSIC on crime’,Drug andAlcohol Review24 (2), pp. 173–84.Galea, S. and Vlahov, D. (2002), ‘Social determinants and the health of drug users: socioeconomic status,homelessness, and incarceration’,Public Health Reports117 (Supplement 1), pp. S135–S145.Gautschi, T., Hangartner, D. and Magnin, C. (2008), ‚Kontakt- und Anlaufstellen der Stadt Zürich. Eine Analyseder Bedürfnisse Ihrer Benützerinnen und Benützer‘, in Stadt Zürich — Sozialdepartement (ed.),„Ein Ort wo mansein kann“. Die Zukunft der „Harm Reduction“ am Beispiel der Kontakt- und Anlaufstellen der Stadt Zürich,EditionSozialpraxis Nr.3, Zürich, pp. 13–57.Geense, R. (1997), ‘Evaluation of the federal measures to reduce problems related to drug use. To have or havenot: that’s the question. A qualitative study on four low-threshold needle exchange services for drug users inSwitzerland’,Cah Rech Doc IUMSP,no. 111.11, University of Social and Preventive Medicine, PreventionProgrammes Evaluation Unit, Lausanne.
324
Chapter 11: Drug consumption facilities in Europe and beyond
Gervasoni, J-P. and Dubois-Arber, F. (2009),Indicateurs de résultats du Promedro III, situation en 2008 : rapportfinal,Raisons de santé 147, Institut universitaire de médecine sociale et préventive, Lausanne.Grund, J-P., Coffin, P., Jauffret-Roustide, M., et al. (2010), ‘The fast and furious: cocaine, amphetamines and harmreduction’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence,impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, PublicationsOffice of the European Union, Luxembourg.Hämmig, R.B. (1992), ‘The streetcorner agency with shooting room (Fixerstübli)’, in O’Hare, P. A., Newcombe, R.,Matthews, A., Buning E. C., and Drucker, E. (eds),The reduction of drug related harm,Routledge, London, pp.181–5.Hämmig, R. and van Beek, I. (2005), ‘Supervised injecting rooms’, in Pates, R., McBride, A. and Arnold, K. (eds),Injecting illicit drugs,Wiley-Blackwell, Chichester.Hall, W. and Kimber, J. (2005), ‘Being realistic about benefits of supervised injecting facilities’,Lancet23–29July, 366 (9482), pp. 271–2.Hartnoll, R., Gyarmarthy, A. and Zabransky, T. (2010), ‘Variations in problem drug use patterns and theirimplications for harm reduction’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harmreduction: evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No.10, Publications Office of the European Union, Luxembourg.Health Canada (2002), ‘Application for an exemption under section 56 of the Controlled Drugs and SubstancesAct for a scientific purpose for a pilot supervised injection site research project: interim guidance document’, DrugStrategy and Controlled Substances Programme, Healthy Environments and Consumer Safety Branch, HealthCanada, Ottawa.Hedrich, D. (2004),European report on drug consumption rooms,EMCDDA, Lisbon.INCB (International Narcotics Control Board) (2008),Report of the International Narcotics Control Board for 2007,E/INCB/2007/1, United Nations, New York. Available at http://www.incb.org/incb/en/annual-report-2007.html(accessed 11 January 2010).Independent Working Group (2006),The report of the Independent Working Group on Drug Consumption Rooms,Joseph Rowntree Foundation, York. Available at http://www.jrf.org.uk/publications/drug-consumption-rooms-summary-report-independent-working-group (accessed 3 June 2009).Jacob, J., Rottmann, J. and Stöver, H. (1999),Entstehung und Praxis eines Gesundheitsraumangebotes fürDrogenkonsumierende. Abschlußbericht der einjährigen Evaluation des ‘drop-in Fixpunkt’ in Hannover,SchriftenreiheSucht- und Drogenforschung, Vol. 2., BIS-Verlag, Universität Oldenburg, Oldenburg.Kemmesies, U. (1995), Szenebefragung 1995.Die offene Drogenszene und das Gesundheitsraumangebot inFrankfurt am Main – ein erster Erfahrungsbericht,Indro, Münster (English version: Kemmesies, U. (1999),The opendrug scene and the safe injection room offers in Frankfurt am Main 1995,Indro, Münster). Available at http://www.indro-online.de/injection_room.htm (accessed 27 August 2009).Kerr, T., Tyndall, M., Li, K., Montaner, J. and Wood, E. (2005), ‘Safer injecting facility use and syringe sharing inIDUs’,Lancet23–29 July, 366 (9482), pp. 316–18.Kerr, T., Stoltz, J. A., Tyndall, M., et al. (2006a), ‘Impact of a medically supervised safer injection facility oncommunity drug use patterns: a before and after study’,BMJ28 January, 332 (7535), pp. 220–2.Kerr, T., Tyndall, M., Lai, C., Montaner, J. and Wood, E. (2006b), ‘Drug-related overdoses within a medicallysupervised safer injection facility’,International Journal of Drug Policy17 (5), pp. 436–41.
325
Harm reduction: evidence, impacts and challenges
Kerr, T., Kimber, J., Debeck, K. and Wood, E. (2007a), ‘The role of safer injection facilities in the response to HIV/AIDS among injection drug users’,Current HIV/AIDS Reports4 (4), pp. 158–64.Kerr, T., Tyndall, M. W., Zhang, R., et al. (2007b), ‘Circumstances of first injection among illicit drug usersaccessing a medically supervised safer injection facility’,American Journal of Public Health97 (7), pp. 1228–30.Kimber, J., Dolan, K., van Beek, I., Hedrich, D. and Zurhold, H. (2003a), ‘Drug consumption facilities: an updatesince 2000’,Drug and Alcohol Review/Harm Reduction Digest21, 22 (2), pp. 227–33.Kimber, J., MacDonald, M., van Beek, I., et al. (2003b), ‘The Sydney Medically Supervised Injecting Centre:client characteristics and predictors of frequent attendance during the first 12 months of operation’,Journal ofDrug Issues33, pp. 639–48.Kimber, J., Dolan, K. and Wodak, A. (2005), ‘Survey of drug consumption rooms: service delivery and perceivedpublic health and amenity impact’,Drug and Alcohol Review24, pp. 21–4.Kimber, J., Hickman, M., Degenhardt, L., Coulson, T., and van Beek, I. (2008a), ‘Estimating the size anddynamics of an injecting drug user population and implications for health service coverage: comparison ofindirect prevalence estimation methods’,Addiction103 (10), pp. 1604–13.Kimber, J., Mattick, R. P., Kaldor, J., et al. (2008b), ‘Process and predictors of treatment referral and uptake’,Drugand Alcohol Review27, pp. 602–12.Kimber, J., Palmateer, N., Hutchinson, S., Hickman, M., Goldberg, D. and Rhodes, T. (2010), ‘Harm reductionamong injecting drug users: Evidence of effectiveness’, in European Monitoring Centre for Drugs and DrugAddiction (EMCDDA)Harm reduction: evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds),Scientific Monograph Series No. 10, Publications Office of the European Union, Luxembourg.Klee, J. (ed.) (1991),Akzeptanzorientierte Angebote in der Drogen- und AIDS-Selbsthilfe: Gesundheitsräume in deraktuellen Debatte,Deutsche Aidshilfe (DAH), Berlin.Klee, H. and Morris, J. (1995), ‘Factors that characterize street injectors’,Addiction90 (6), pp. 837–41.Krüsi, A., Small, W., Wood, E. and Kerr, T. (2009), ‘An integrated supervised injecting program within a carefacility for HIV-positive individuals: a qualitative evaluation’,AIDS Care21 (5), pp. 638–44.Latkin C., Mandell, W, Vlahov, D., et al. (1994), ‘My place, your place and no place: behaviour settings as a riskfactor for HIV-related injection practices of drug users in Baltimore, Maryland’,American Journal of CommunityPsychology22, pp. 415–30.Linssen, L., de Jong, W. and Wolf, J. (2001),Gebruiksruimten. Een systematisch overzicht van de voorziening en deeffecten ervan.Series: Resultaten Scoren, Trimbos Instituut, Utrecht. Available at www.ggznederland.nl/scrivo/asset.php?id=306955 (accessed 3 June 2009).Lloyd, C. and Hunt, N. (2007), ‘Drug consumption rooms: an overdue extension to harm reduction policy in theUK?’,International Journal of Drug Policy18, pp. 5–7.Lloyd-Smith, E., Wood, E., Zhang, R., et al. (2009), ‘Determinants of cutaneous injection-related care at asupervised injecting facility’,Annals of Epidemiology19, pp. 404–09.Maher, L. and Dixon, D. (1999), ‘Policing and public health: harm minimization and law enforcement in a street-level drug market’,British Journal of Criminology39, pp. 488–512.Maher, L. and Salmon, A. (2007), ‘Supervised injecting facilities: how much evidence is enough?’,Drug andAlcohol ReviewJuly 26 (4), pp. 351–3.
326
Chapter 11: Drug consumption facilities in Europe and beyond
Macías, J., Palacios, R. B., Claro, E., et al. (2008), ‘High prevalence of hepatitis C virus infection amongnoninjecting drug users: association with sharing the inhalation implements of crack,Liver InternationalJuly, 28(6), pp. 781–6.McKnight, I., Maas, B., Wood, E., et al. (2007), ‘Factors associated with public injecting among users ofVancouver’s supervised injection facility’,American Journal of Drug and Alcohol Abuse33 (2), pp. 319–25.Meijer, G., de Jong, A., Koeter, M. and Bieleman, B. (2001),Gebruik van de straat. Evaluatie gebruiksruimnteBinnenstad-Zuid Groningen,Amsterdam Institute for Addiction Research (AIAR)/Intraval, Amsterdam/Groningen.Abstract in Dutch available at http://blowkwartet.nl/default4597.html?back=1 (accessed 15 January 2010).Milloy, M. J. and Wood, E. (2009), ‘Emerging role of supervised injecting facilities in human immunodeficiencyvirus prevention’,Addiction104 (4), pp. 620–1.Milloy, M. J., Kerr, T., Tyndall, M., Montaner, J. and Wood, E. (2008), ‘Estimated drug overdose deaths avertedby North America’s first medically-supervised safer injection facility’,PLoS ONE3 (10), p. e3351.Minder Nejedly, M and Bürki, C. M. (1999), ‘Monitoring HIV risk behaviours in a street agency with injectionroom in Switzerland’, dissertation, Medical Faculty of the University in Berne, Berne.MSIC Evaluation Committee (2001),Evaluation Protocol for the trial of a Medically Supervised Injecting Centre inKings Cross,NSW Parliament, Standing Committee on Social Issues, Sydney. Available at http://www.worldcat.org/oclc/223407460&referer=brief_results (accessed 23 October 2009).MSIC Evaluation Committee (2003),Final report of the evaluation of the Sydney Medically Supervised InjectingCentre,Authors, Sydney. Available at http://www.druginfo.nsw.gov.au/__data/page/1229/NDARC_final_evaluation_report4.pdf (accessed 3 June 2009).Navarro, C. and Leonard, L. (2004), ‘Prevalence and factors related to public injecting in Ottawa, Canada:implications for the development of a trial safer injecting facility’,International Journal of Drug Policy,15, pp.275–84.NCHECR (National Centre in HIV Epidemiology and Clinical Research) (ed.) (2005),Sydney Medically SupervisedInjecting Centre evaluation report no. 1: operations and service delivery (November 2002 to December 2004),University of New South Wales, Sydney. Available at http://www.nchecr.unsw.edu.au/NCHECRweb.nsf/resources/Interim_eval_Rep1/$file/INT_EVAL_REP_+1_SYD_+MSIC.pdf (accessed 3 June 2009).NCHECR (ed.) (2006),Sydney Medically Supervised Injecting Centre evaluation report no. 2: evaluation ofcommunity attitudes towards the Sydney MSIC,University of New South Wales, Sydney. Available at http://www.nchecr.unsw.edu.au/NCHECRweb.nsf/resources/Interim_eval_Rep1/$file/IntRep2SurveyMSICJul06.pdf(accessed 3 June 2009).NCHECR (ed.) (2007a),Sydney Medically Supervised Injecting Centre evaluation report no. 3: evaluation of clientreferral and health issues,University of New South Wales, Sydney. Available at http://www.nchecr.unsw.edu.au/NCHECRweb.nsf/resources/Interim_eval_rep_2/$file/EvalRep4SMSIC.pdf (accessed 3 June 2009).NCHECR (ed.) (2007b),Sydney Medically Supervised Injecting Centre evaluation report no. 4: evaluation of serviceoperation and overdose-related events,National Centre in HIV Epidemiology and Clinical Research, University ofNew South Wales, Sydney. Available at http://www.nchecr.unsw.edu.au/NCHECRweb.nsf/resources/Interim_eval_rep_2/$file/EvalRep4SMSIC.pdf (accessed 3 June 2009).Neaigus, A., Gyarmathy, V. A., Miller, M., et al. (2007), ‘Sexual and other noninjecting risks for HBV and HCVseroconversions among noninjecting heroin users’,Journal of Infectious Diseases195 (7), pp. 1052–61.Palepu, A., Tyndall, M. W., Leon, H., et al. (2001), ‘Hospital utilization and costs in a cohort of injection drugusers’,Canadian Medical Association Journal165, pp. 415–20.
327
Harm reduction: evidence, impacts and challenges
Parliament of New South Wales (1998),Joint Select Committee into Safe Injecting Rooms report on the establishmentor trial of safe injecting rooms,Parliament of New South Wales, Sydney. Available at http://www.parliament.nsw.gov.au/safeinjectingrooms (accessed 3 June 2009).Petrar, S., Kerr, T., Tyndall, M. W., et al. (2007), ‘Injection drug users’ perceptions regarding use of a medicallysupervised safer injecting facility’,Addictive Behaviours32 (5), pp. 1088–93.Pretil, X. S. (2007), ‘En qué sentido deberían evolucionar las salas de consumo supervisado?’Mesa redonda, ddzcdd,October 2007, 144, p. 10.Poschadel, S., Höger, R., Schnitzler, J. and Schreckenberger, J. (2003),Evaluation der Arbeit derDrogenkonsumräume in der Bundesrepublik Deutschland: Endbericht im Auftrag des Bundesministeriums fürGesundheit,Das Bundesministerium für Gesundheit und Soziale Sicherung (Schriftenreihe Bd 149), Nomos-Verlags-Gesellschaft, Baden-Baden.Reyes Fuentes, V. C. (2003), ‘15 Jahre Fixerraum Bern. Auswirkungen auf soziale und medizinische Aspekte beiDrogenabhängigen’, dissertation at the Medical Faculty of the University of Berne.Rhodes, T. (2002), ‘The “risk environment”: a framework for understanding and reducing drug-related harm’,International Journal of Drug Policy13, pp. 85–94.Rhodes, T., Lilly, R., Fernández, C., et al. (2003), ‘Risk factors associated with drug use: importance of “riskenvironment”’,Drugs: education, prevention, and policy,10 (4), pp. 303–29.Rhodes, T., Kimber, J., Small, W., et al. (2006), ‘Public injecting and the need for “safer environmentinterventions” in the reduction of drug-related harm’,Addiction101, pp. 1384–93.Rhodes, T., Watts, L., Davies, S., et al. (2007), ‘Risk, shame and the public injector’,Social Science and Medicine65, pp. 572–85.Ronco, C., Spuler, G., Coda, P. and Schöpfer, R. (1994),Evaluation der Gassenzimmer I, II und III in Basel (fullreport),Institut für Sozial- und Präventivmedizin der Universität Basel, Basel.Ronco, C., Spuler, G., Coda, P. and Schöpfer, R. (1996a), ‘Evaluation der Gassenzimmer I, II und III in Basel[Evaluation of street facilities I, II and III in Basel]’,Sozial- und Präventivmedizin,41 (Supplement 1), pp. S58–S68.Abstract in English available at http://www.ncbi.nlm.nih.gov/pubmed/8693818.Ronco, C., Spuhler, G. and Kaiser, R. (1996b), ‘Evaluation des “Aufenthalts- und Betreuungsraums fürDrogenabhängige” in Luzern [Evaluation of a stay and care center for drug addicts in Lucerne]’,Sozial- undPräventivmedizin,41 (Supplement 1), pp. S45–S57. Abstract in English available at http://www.ncbi.nlm.nih.gov/pubmed/8693816.Salmon, A., Thein, R., Kimber, J., Kaldor, J. and Maher, L. (2007), ‘Five years on: what are the communityperceptions of drug-related public amenity following the establishment of the Sydney Medically SupervisedInjecting Centre?’,International Journal of Drug Policy18 (1), pp. 46–53.Salmon, A. M., Dwyer, R., Jauncey, M., et al. (2009a), ‘Injecting-related injury and disease among clients of asupervised injecting facility’,Drug Alcohol Dependence101 (1–2), pp. 132–6.Salmon, A. M., van Beek, I., Amin, J., Grulich, A. and Maher, L. (2009b), ‘High HIV testing and low HIVprevalence among injecting drug users attending the Sydney Medically Supervised Injecting Centre’,Australianand New Zealand Journal of Public Health33 (3), pp. 280–3.Schechter, M. T., Strathdee, S. A., Cornelisse, P. G., et al. (1999), ‘Do needle exchange programmes increase thespread of HIV among injection drug users? An investigation of the Vancouver outbreak’,AIDS16 April, 13 (6),pp. F45–F51.
328
Chapter 11: Drug consumption facilities in Europe and beyond
Scherbaum, N., Specka, M., Bombeck, J. and Marziniak, B. (2009), ‘Drug consumption facility as part of aprimary health care centre for problem drug users: which clients are attracted?’,International Journal of DrugPolicy20 (5), pp. 447–9.Simmedinger, R. and Vogt, I. (2008),Auswertung der Frankfurter Konsumraumdokumentation 2007. Endbericht,ISFF, Frankfurt am Main.Skretting, A. and Olsen H. (2008), ‘The Norwegian injection room trial: politics and controversies’,Nordic Studieson Alcohol and Drugs25 (4), pp. 269–83.Small, W., Rhodes, T., Wood, E. and Kerr, T. (2007), ‘Public injecting settings in Vancouver: physicalenvironment, social context and risk’,International Journal of Drug Policy18, pp. 27–36.Small, W., Wood, E., Lloyd-Smith, E., Tyndall, M. and Kerr, T. (2008), ‘Accessing care for injection-relatedinfections through a medically supervised injecting facility: a qualitative study’,Drug and Alcohol Dependence98(1–2), pp. 159–62.Solai, S., Benninghoff, B., Meystre-Agustoni, G., Jeannin, A. and Dubois-Arber, F. (2004), ‘Evaluation de l’espaced’accueil et d’injection “Quai 9” à Genève: deuxième phase 2003’,Raisons de santé,102, Institut universitaire demédecine sociale et préventive, Lausanne. Available at http://www.iumsp.ch/Unites/uepp/files/Quai9GE_2.pdf(accessed 3 June 2009).Solai, S., Dubois-Arber, F., Benninghoff, F. and Benaroyo, L. (2006), ‘Ethical reflections emerging during theactivity of a low threshold facility with supervised drug consumption room in Geneva, Switzerland’,InternationalJournal of Drug Policy17 (1), pp. 17–22.Sozialdepartement der Stadt Zürich (ed.) (2008),„Ein Ort wo man sein kann“. Die Zukunft der „Harm Reduction“am Beispiel der Kontakt- und Anlaufstellen der Stadt Zürich,Edition Sozialpraxis Nr. 3, Zürich.Spreyermann, C. and Willen, C. (2003),Evaluationsbericht Öffnung der Kontakt- und Anlaufstellen für risikoärmereKonsumformen. Evaluation der Inhalationsräume der Kontakt- und Anlaufstellen Selnau und Seilergraben derAmbulanten Drogenhilfe Zürich,Sfinx, Berne. Available at http://www.sfinx.ch/siteman/file/innovation/Evaluationsbericht.pdf (accessed 3 June 2009).Springer, A. (2003),Konsumräume. Expertise im Auftrag des Fonds Soziales Wien,Ludwig-Boltzmann-Institut fürSuchtforschung, Anton-Proksch-Institut, Wien. Available at http://www.api.or.at/lbi/pdf/040622_expertise_konsumraeume.pdf (accessed 3 June 2009).Stoltz, J. A., Wood, E., Small, W., et al. (2007), ‘Changes in injecting practices associated with the use of amedically supervised safer injection facility’,Journal of Public Health29 (1), pp. 35–9.Stöver, H. (ed.) (1991),Der tolerierte intravenöse Drogengebrauch in den Angeboten der Drogen- und AIDS-Hilfe.Ein Sammelband,AIDS-Forum der Deutschen AIDS-Hilfe, Vol. VI, DAH, Berlin.Stöver, H. (2000), ‘Konsumräume als professionelles Angebot der Suchtkrankenhilfe - Internationale Konferenzzur Erarbeitung von Leitlinien’,Bundesgesundheitsblatt — Gesundheitsforschung — Gesundheitsschutz,43, pp.290–2.Stöver, H. (2002), ‘Consumption rooms: a middle ground between health and public order concerns’,Journal ofDrug Issues32 (2), pp. 597–606.Thein, H. H., Kimber, J., Maher, L., MacDonald, M. and Kaldor, J. M. (2005), ‘Public opinion towards supervisedinjecting centres and the Sydney Medically Supervised Injecting Centre’,International Journal of Drug Policy16(4), pp. 275–80.Tyndall, M. (2003), ‘Impact of supervised injection facilities on community HIV levels: a public healthperspective’,Expert Review of Anti-Infective Therapy1 (4), pp. 543–9.
329
Harm reduction: evidence, impacts and challenges
Tyndall, M., Kerr, T., Zhang, R., et al. (2006), ‘Attendance, drug use patterns and referrals made from NorthAmerica’s first supervised injection facility’,Drug and Alcohol Dependence83, pp. 193–8.van Beek, I. (2003), ‘The Sydney Medically Supervised Injecting Centre: a clinical model’,Journal of Drug Issues33, pp. 625–38.van Beek, I. (2007),The Medically Supervised Injecting Centre: the first 7 years,Clinical Activity Data. Available atwww.sydneymsic.com (MSIC_NDARC_07.ppt) (accessed 27 August 2009).van Beek, I., Kimber, J., Dakin, A and Gilmour, S. (2004), ‘The Sydney Medically Supervised Injecting Centre:reducing harm associated with heroin overdose’,Critical Public Health14 (4), pp. 391–406.van der Poel, A., Barendregt, C. and van de Mheen, D. (2003), ‘Drug consumption rooms in Rotterdam: anexplorative description’,European Addiction Research,9, pp. 94–100.Willen, C. (2002),Evaluation Inhalationsraum. Pilotprojekt der Anlaufstelle Rötzmatt, Suchthilfe Region Olten (SHO),Sfinx, Berne. Available at http://www.sfinx.ch/html/portfolio_act.html (accessed 3 June 2009).Wolf, J., Linssen, L. and de Graaf, I., assisted by van Dam, T. (2003), ‘Drug consumption facilities in theNetherlands’,Journal of Drug Issues33, pp. 649–61.Wood, E., Kerr, T., Spittal, P. M., et al. (2003), ‘The potential public health and community impacts of saferinjecting facilities: evidence from a cohort of injecting drug users’,Journal of Acquired Immune DeficiencySyndrome32 (1), pp. 2–8.Wood, E., Kerr, T., Lloyd-Smith, E., et al. (2004a), ‘Methodology for evaluating Insite: Canada’s first medicallysupervised safer injection facility for injection drug users’,Harm Reduction Journal1 (1), p. 9. Available at http://www.harmreductionjournal.com/content/1/1/9 (accessed 3 June 2009).Wood, E., Kerr, T., Montaner, J. S., et al. (2004b), ‘Rationale for evaluating North America’s first medicallysupervised safer-injecting facility’,Lancet Infectious Diseases4, pp. 301–06.Wood, E., Kerr, T., Small, W., et al. (2004c), ‘Changes in public order after the opening of a medicallysupervised safer injecting facility for illicit injection drug users’,Canadian Medical Association Journal,171 (7),pp. 731–4.Wood, E., Tyndall, M. W., Stoltz J. A., et al. (2005a), ‘Factors associated with syringe sharing among users of amedically supervised safer injecting facility’,American Journal of Infectious Diseases1 (1), pp. 50–4.Wood, E., Tyndall, M.W., Li, K., et al. (2005b), ‘Do supervised injecting facilities attract higher-risk injection drugusers?’,American Journal of Preventive Medicine,29 (2), pp. 126–30.Wood, E., Tyndall, M. W., Qui, Z., et al. (2006a), ‘Service uptake and characteristics of injection drug usersutilizing North America’s first medically supervised safer injecting facility’,American Journal of Public Health,96,pp. 770–3.Wood, E., Tyndall, M. W., Montaner, J. S. and Kerr, T. (2006b), ‘Summary of findings from the evaluation of apilot medically supervised safer injecting facility’,Canadian Medical Association Journal,175 (11), pp. 1399–404.Wood, E., Tyndall, M. W., Lai, C., Montaner, J. S. and Kerr, T. (2006c), ‘Impact of a medically supervised saferinjecting facility on drug dealing and other drug-related crime’,Substance Abuse Treatment, Prevention, and Policy,1 (13). Published online 8 May 2006. DOI: 10.1186/1747-597X-1-13.Wood, E., Lloyd-Smith, E., Li, K., et al. (2007a), ‘Frequent needle exchange use and HIV incidence in Vancouver,Canada’,American Journal of Medicine120 (2), pp. 172–9.
330
Chapter 11: Drug consumption facilities in Europe and beyond
Wood, E., Tyndall, M. W., Zhang, R., Montaner, J. S. and Kerr, T. (2007b), ‘Rate of detoxification service useand its impact among a cohort of supervised injecting facility users’,Addiction102 (6), pp. 916–19.Wood, R. A., Wood, E., Lai, C., et al. (2008), ‘Nurse-delivered safer injection education among a cohort ofinjection drug users: evidence from the evaluation of Vancouver’s supervised injection facility’,InternationalJournal of Drug Policy19 (3), pp. 183–8.Zobel, F. and Dubois-Arber, F. (2004),Short appraisal of the role and usefulness of drug consumption facilities (DCF)in the reduction of drug-related problems in Switzerland: produced at the request of the Swiss Federal Office of PublicHealth,Institut universitaire de médecine sociale et préventive, Lausanne. Available at http://www.bag.admin.ch/evaluation/01759/02066/02343/index.html?lang=en (accessed 3 June 2009).Zobel, F., Thomas, R., Arnaud, S., et al. (2003),Global evaluation of the Confederation’s measures to reduce drug-related problems (ProMeDro): fourth synthesis report 1999–200,Institut universitaire de médecine sociale etpréventive, Lausanne. Available at http://www.iumsp.ch/Unites/uepp/files/tox4_en.pdf (accessed 3 June 2009).Zurhold, H., Kreuzfeld, N., Degkwitz, P. and Verthein, U. (2001),Drogenkonsumräume. Gesundheitsförderung undMinderung öffentlicher Belastungen in europäischen Grossstädten,Lambertus, Freiburg.Zurhold, H., Degkwitz, P., Verthein, U. and Haasen, C. (2003), ‘Drug consumption rooms in Hamburg, Germany:evaluation of the effects on harm reduction and the reduction of public nuisance’,Journal of Drug Issues33, pp.663–88.
331
Chapter 12User involvement and user organising in harm reductionNeil Hunt, Eliot Albert and Virginia Montañés Sánchez
AbstractWithin Europe, the active involvement of drug users in services and activities that affect theirlives can be traced back to the Netherlands in the 1970s, pre-dating the development ofharm reduction in response to HIV/AIDS. This chapter distinguishes involvement approaches,which typically focus on improving treatment and care, from user-led initiatives, whereobjectives are determined more autonomously. The chapter describes differences in userinvolvement and organising with respect to the preferred drugs of different populations(heroin and cocaine, ‘party drugs’ and cannabis). We also highlight the different aims andmethods of user involvement and user organising initiatives. These also illustrate differencesthat are shaped by: the drugs used; the context of their use; and national contrasts in patternsof use and harm. In addition to noting some of the practical challenges linked to userinvolvement/organising, we also note potential tensions, most notably regarding disputesabout the extent to which drug prohibition is construed as a cause of harm, and its reformseen as a legitimate target for drug users’ activism. Finally, we summarise available evidenceof the impact of user involvement and organising. We conclude that harms can best bereduced where affected people participate meaningfully in decisions concerning the systemsand services that shape their lives. This requires clear commitment at every level and willfrequently need corresponding resources, if its full potential is to be realised.Keywords:harm reduction, user involvement, user organising, user-led, empowerment.
IntroductionAcross Europe, patterns of drug use and their corresponding burden of harms differconsiderably (EMCDDA, 2008). Such variations in drug use have implications for harmreduction responses. Variations in patterns of drug use are shaped by geographical factors,such as the suitability of the climate for drug production, or trafficking and transit routes. Butthey are also shaped by social factors, as are harm reduction responses. These include: thecultural and ethnic context; national legislation; the policies of the prevailing government; theinfluence of organised religion; national traditions concerning the role of civil society; and theeconomic situation. Social contexts thus shape patterns of drug use and harm, as well as itsreduction, including the role of user involvement and user organising. As Friedman hascommented, ‘the structures of drug scenes affect what users’ groups can do and how theycan function’ (Friedman, 1996, p. 212).Harm reduction is grounded within a public health model, which primarily aims to improvethe health and well-being of drug users alongside reducing community and societal levelharms (Newcombe, 1992). As such, a desire to make the services user-friendly (i.e. providing333
Harm reduction: evidence, impacts and challenges
services that welcome and include drug users) and involving drug users is evident withinformal definitions of harm reduction (Hunt et al., 2003) as well as within harm reductionpractice. Yet the way that harm reduction is understood and translated into practice isvariable, and this is reflected within drug user involvement and organising.The geographical focus of this chapter is Europe. Nevertheless, some of the more relevantfeatures of the international context are described. The main goal of the chapter is todescribe and explain drug users’ contributions to harm reduction, alongside the contrastingmethods that comprise user involvement and organising. The constraints of a single, shortchapter mean it is impossible to provide a comprehensive history of the drug usermovement’s contribution to harm reduction. Likewise, it is not feasible to provide a detailed,country-by-country account of all user involvement and organising. Some important featuresof this history are, nevertheless, included.Within the drug user movement, there is ongoing debate about the language that should beused to refer to its participants. For example, some people readily describe themselves as‘addicts’ or ‘patients’, whereas others resist such terms because of their implications regardingthe legitimacy of medical power to shape their drug-using choices and the applicability of adisease model. Questions also arise as to who is a drug user and the role of non-drug-usingsupporters of drug user activists (Balian and White, 1998). While acknowledging the disputessurrounding these terms, we will largely use the terms ‘user’ or ‘drug user’, although eventhese terms are not without their critics.
HistoryThe AIDS pandemic has clearly been a critical factor in the development of both the harmreduction movement and drug user organising (Crofts and Herkt, 1995; Zibbell, 2004).However, it is important to note that drug user activism does not relate purely to injecting,and it pre-dates the AIDS era. Theo van Dam credits Nico Adriaans as the founder andchairman of the first advocacy/activist group Rotterdam Junkie Union (RJB) in theNetherlands in 1977 (van Dam, 2008, p. 58). Around this time, van Dam and Daan van derGouwe also started Landelijk Steunpunt Druggebruikers (LSD) to try to get the Dutchgovernment to support users and user groups, reduce stigma and shape opinion aroundlegalisation (Jezek, 2000; Tops, 2006; Museummouse, 2008). Initially, harm reduction wasan offshoot of the drug users’ movement, notably Dutch activists who established the world’sfirst needle exchange programme, set up by the MDHG Belangenvereniging Druggebruikers(Interest Association for Drug Users) in 1984 (Tops, 2006).Montañés Sánchez and Oomen define drug users’ organisations as ‘Organisations of usersof prohibited drugs or organisations in which these people play an important role’, andidentify three types of organisations according to the profile of the users and the scene inwhich they use drugs: cannabis users; party drug users; and users of street drugs such asopiates and cocaine (Montañés Sánchez and Oomen, 2009, p. 213). Although our emphasishere is on user organising within the third group, we also include examples relating tocannabis users and ‘party drugs’.334
Chapter 12: User involvement and user organising in harm reduction
Drug user organising in EuropeAlthough there are publications that describe aspects of European drug users’ activism, suchas that of the Correlation Network (Bröring and Schatz 2008), accurately mapping the extentof drug users’ organisations and their work is problematic. No survey has yet beenundertaken across the whole of Europe using a consistent methodology. Any survey is alsocomplicated because: activities are not necessarily publicly or well documented; someorganisations have a short lifespan; and, stigma and the oppression of drug users mean thatthere are good reasons for organisations to avoid being too visible (Friedman, 1998). Inaddition, the work of some drug users is sometimes obscured, such as when drug useridentities are not declared within services (Robbins, 2004). At the time of writing, theInternational Harm Reduction Association (IHRA) and the International Network of Peoplewho Use Drugs (INPUD) are developing a report describing the ‘global state of drug useractivism’. In time, this should provide a useful addition to what is currently known about theextent of drug user organisations.Dolf Tops estimates that, at any one time, there are between 15 and 30 drug users’organisations in the Netherlands (Tops, 2006, p. 65). By 1994, such organisations existed inat least 11 European countries (Germany, the Netherlands, the United Kingdom, Norway,Denmark, Slovenia, France, Belgium, Italy, Lithuania and Spain) (Jürgens, 2008, p. 15).In the Nordic countries, the first organisations for active drug users were formed duringthe 1990s in Denmark and Norway, and in Sweden in the early 2000s. In Finland, thefirst user-driven organisation was established in 2004. These drug user organisationswere founded by heroin users, they are run by heroin users and users in maintenancetreatment, and they also cater for active drug users, mainly heroin users (Anker et al.,2008, p. 18).In France and Spain the first drug users’ organisations started in the 1990s. Auto-supportparmi les Usagers de Drogues (ASUD) was created in France in 1992 (Jürgens, 2008, p.24). In 1996, the Spanish National Coordination for the Normalisation of Cannabis wasborn, largely comprising associations of cannabis users (Barriuso, 2003, p. 103); thisdeveloped into the Spanish Federation of Cannabis Associations (FAC, in Spanish)(Barriuso, 2007), and in 2003 the first national network of injecting drug users’organisations was created in Spain — the Spanish Nationwide Network of People Affectedby Drugs and HIV (FAUDAS) (Pretel, 2007).During 2003/4 the Central and Eastern European Harm Reduction Network (CEEHRN)assessed the needs of drug users’ organisations across Central and Eastern Europe andCentral Asia. Respondents came from 16 countries: Armenia, Belarus, Bulgaria, Croatia,Estonia, Georgia, Kazakhstan, Kyrgyzstan, Latvia, Lithuania, former Yugoslav Republic ofMacedonia, Moldova, Poland, Romania, Russia, and Ukraine. They identified 41organisations, of which 15 were for drug users in general, 19 were for people living withHIV/AIDS (PLWHA), and six were for HIV positive drug users (CEEHRN, 2004; CanadianHIV/AIDS Legal Network, 2008).335
Harm reduction: evidence, impacts and challenges
Contribution of international networks to promoting user involvementDevelopments in Europe need to be understood in the context of global networks. These havebeen important for enabling drug users to share ideas, knowledge and skills internationally— both into and out of Europe — and to provide structures within which drug users havebegun to work internationally to identify and address common concerns.The IHRA is a global organisation that promotes harm reduction. It seeks to involve drugusers in its meetings and processes and has provided opportunities for drug users tonetwork internationally, which has facilitated the development of international drug usernetworks.The International Drug Users Network (IDUN) was initiated in 1992 at IHRA’s Melbourneconference and was, arguably, the first network of its kind. Representatives from Germany,the Netherlands and the United Kingdom were among the seven countries represented at theinaugural meeting (Byrne, 2000). IDUN aimed to support injecting drug users to exchangeideas, develop drug user groups, and set up needle exchanges. However, a lack of fundingand competing national and local demands for members’ time meant that the networkproved hard to sustain.The Internet has enabled an electronic network for international drug user organising tobe created, and after the IHRA conference in Geneva in 1998 a network of activistsbegan an international discussion list hosted by the American Drug Policy Foundation,called Drug Policy Foundation — Users (DPFU) (Efthimiou-Mordaunt, 2005). Thisfunctions as a loose network of activists and facilitates ongoing discussion between drugusers internationally.In 2005, frustration at the poor facilities for drug users at IHRA’s Belfast conference wasa catalyst for an invigorated international network and led to the inception of INPUD.This formed around a statement that was endorsed at IHRA’s 2006 conference — ‘TheVancouver declaration’ (INPUD, 2006). Although this was the product of many activists’efforts, the initial process of transforming INPUD into a legal entity was undertaken by aworking group including representatives from Asia, Europe, Latin America, NorthAmerica and Oceania. This was initially facilitated by Grant McNally (United Kingdom)with technical assistance from Stijn Goossens (Belgium), who subsequently becameINPUD’s director. Financial support was provided from the United Kingdom’s Departmentfor International Development (DfID) through IHRA. INPUD’s early phase was marked byproblems concerning who was/was not a member and associated constitutionalproblems. A subsequent crisis meeting was held at IHRA’s Barcelona conference in 2008,which led to a successful re-foundation General Meeting held in Copenhagen at the endof October 2008, where a Consensus Statement and a clearer infrastructure were bothagreed. Since then, a representative from INPUD was invited to give a formal address aspart of the United Kingdom delegation to the United Nations’ Commission on NarcoticDrugs (CND) in April 2009 and several other members attended as part of various NGOdelegations.336
Chapter 12: User involvement and user organising in harm reduction
International drug user activists, Vienna 2009
The networks and structures described so far are global and have clear, historical connections tothe harm reduction movement and some emphasis on injecting drug use. By contrast, theENCOD (1) (the European Coalition for Just and Effective Drug Policies) is a European network of175 organisations and citizens affected by current drug policies, which also incorporatesmembers with a more diverse range of concerns including all kinds of prohibited drugs. Createdin 1994 by a group of European NGOs to work on drugs and development issues, it has becomea drug policy reform network whose membership includes: drug users’ organisations; harmreduction organisations; research groups; advocacy groups; and, individual members. Since itscreation, ENCOD has advocated for drug policy changes at the European and UN level and forthe participation of organisations and people affected by drugs/drug policies within the UN, theEuropean Union and each country’s government (ENCOD, 2006).In 1998, a corresponding International Coalition of NGOs for Just and Effective Drug Policies(ICN) was founded by more than 200 organisations based on a ‘Manifesto for just and effectivedrug policies’, presented at that year’s UN General Assembly Special Session on Drugs. Althoughless active than its European section (ENCOD), it appears to be the only formal international bodywhere producers’ and users’ organisations can work together and pursue, among other things,the ‘non-prosecution of drugs consumption while looking for means of regulation which aresocially and culturally acceptable to those local populations involved, and the implementation ofbroad measures, including harm reduction, to prevent and treat the problematic consumption ofdrugs’ (ICN, 1998). In 2004, ENCOD’s General Assembly decided to adopt the title of theManifesto in ENCOD’s name, and signing it is one of the conditions of becoming a member.(1)The acronym ENCOD stood initially for European NGO Council on Drugs.
337
Harm reduction: evidence, impacts and challenges
In 2005, the network Correlation: European Network Social Inclusion and Health was initiatedto address health inequalities among marginalised groups. It has an extensive number ofpartners and receives financial support from the European Commission and the Dutch Ministryof Health. Within their work, HIV and Hepatitis C are specific concerns; drug users are one oftheir priorities and harm reduction and peer support are among the areas where they aim topromote effective practice. Their website provides extensive access to publications and otherresources relevant to user involvement and organising (Correlation, 2009).
Forms of drug user involvement and organisingActively involving people in decisions about their personal treatment and service provision isprobably the most basic way by which user involvement can be said to take place. Theliterature shows that ‘user involvement’ is sometimes used to refer to the extent to whichsomeone is involved in determining their own treatment or care from a service (Fischer andJenkins, 2007). There are also other relatively passive ways of ‘involving’ drug users, such asthe use of suggestion boxes or asking people to rate their satisfaction with the service.Whatever the merits of those activities, the focus of this chapter is on more active forms ofdrug user involvement and organisation within harm reduction. At the outset, we draw adistinction between involvement and organising.User involvementSome groups are keen to involve drug users within the systems and structures that affect theirlives. In practice, involvement typically means giving a degree of power to drug users in waysthat are managed and circumscribed, for example some form of consultation with individualsor groups who are deemed to represent the drug using population. Including service userswithin staff recruitment would be an example of user involvement that can directly benefitboth the drug user and the organisation (Foster et al., 2007). Organisations in the drugs fieldoften attempt to motivate their service users to set up user groups — a process that theAustralian drug user activist Jude Byrne has termed ‘contrived spontaneity’ (Byrne, 2000).Results seem highly variable; many fail or flounder, others thrive and may occasionally layfoundations for more autonomous organisations to develop.User organisingOrganising implies more autonomous organisation by drug users to work across self-determined agendas affecting their interests. It is more directly linked to the ‘empowerment’of the affected population. The term ‘user-led’ denotes this principle, yet allows a role forprofessionals too. In Canada, the term ‘user-driven’ is used (personal correspondence, WalterCavalieri, 2009). Bröring and Schatz use the term ‘self-organisations of drug users’ (Bröringand Schatz, 2008). Again, this suggests the central importance of independence andautonomy. For brevity, we will use the term ‘user-led’ to refer to organisations of this type.User-led organisations often differ from treatment or care services, within which involvementis encouraged. Although interests frequently coincide regarding threats to health, user-led338
Chapter 12: User involvement and user organising in harm reduction
organisations may engage more actively with wider issues such as discrimination regardingtheir civil rights and the impact of legislation on their personal consumption choices. Methodsmay also differ; groups with more independence may be more prepared to use direct actionto highlight an issue or effect change (Kerr et al., 2006).In practice, these categories are often blurred. A drug user group that has been nurturedwithin a service as part of a process of involvement might reconstitute itself or progressivelypursue a more independent, user-led agenda. Nevertheless, the distinction between systemsthat seek to consult or involve drug users in services, and those where power is asserted moredirectly in accordance with the concerns of drug users is an important one.The ‘JES network’ — an example of user involvement in Germany (DirkSchäffer)Since its establishment in 1989, the JES network (Junkies, Ehemalige, Substituierte — Junkies,ex-users, substitution clients) users have been involved in its harm reduction initiatives atdifferent levels.An interesting and effective collaboration has existed for the past ten years between the ‘AIDSHilfe’ NGO in Oldenburg and the local JES group, whose members provide safer use andsafer sex education to prison inmates.In some cities, such as Cologne, Bonn, Osnabrück, Braunschweig and Stuttgart, JES groupshave become an integral part of the local network of drugs services and carry out importanttasks, such as needle and syringe exchange.The project ‘JES-Seminars’ is characterised by combining knowledge from self-help andacquired expertise. To promote the professionalism of activists in JES groups, the networkconducts self-organised training sessions for users, in order to increase and expand thecompetencies of drug using people.An impressive form of collaboration and cooperation between professional drugs serviceproviders and user groups is in the preparation and implementation of a ‘remembrance day’for deceased drug users, which has been held for over 10 years on 21 July in more than 40cities in Germany. The event represents a great opportunity for users to discuss amongthemselves and with other citizens their vision for a progressive and liberal drug policy.Of course, cooperation with the local drug services network is not always without problems. Therole of JES as a component and at the same time critical counterpart of the drug system sometimeschallenges the interests of aid agencies. However, in many cities successful collaboration betweenJES groups and the professional drugs help system has grown through mastering this challenge.The particular strength of the JES self-help network lies in a specific approach to the problemsof drug users, which has developed from personal experience, is orientated towardsempowerment and aims at improving the skills of those seeking help. By developing andstrengthening informal networks, new and qualitatively different resources and possibilities— beyond those accessible through the professional help system — can be opened up.JES sees its offers of help and support, therefore, as a supplement to professional assistanceand hence as increasing the effectiveness of such services. In this sense, JES offers of assistanceare complementary rather than competing with the professional system of assistance.Further reading: Schäffer and Hentschel (2004).
339
Harm reduction: evidence, impacts and challenges
Aims and methods of interventionIn summarising the aims of user involvement and organising, several complications arise.Groups sometimes comprise loose associations, rather than being legally constitutedorganisations with a written statement of their aims. In some cases, aims also overlap orinteract; for example, an aim of reducing stigma may affect an aim to improve treatment, orvice versa. This makes the production of any definitive list of aims problematic.Aims relating to harm reduction that are readily identifiable within user involvement andorganising include: responding to public health threats; improving the accessibility andquality of drug services; improving the accessibility and quality of other services to drugusers; shaping and reforming drug policy; reducing stigma and increasing publicunderstanding; improving the quality of life for drug users, their families and localcommunities; knowledge production; and drug law reform.A recent typology of the methods used to achieve such aims derives from the categorisationof activities reported from an online, international survey of drug users’ organisations,conducted in 2007 by the International Network of People Who Use Drugs (INPUD) incooperation with the European Correlation Network (Goossens, 2008). Based on a sampleof 38 organisations from 21 countries, Goossens grouped the activities into eleven majorcategories:1. Advocacy and health/drug policymaking.2. Peer support for people living with HIV/AIDS (PLWHA).3. Peer support for drug users.4. HIV and other blood-borne disease (BBD) education and prevention.5. Issue/publish electronic and printed magazines and newsletters.6. Producing other types of informational material.7. Organise, conduct, moderate training, workshops, seminars, peer meetings.8. Educational and peer support work in the party scene.9. Run accommodation projects.10. Drop-in centres with various services.11. Raise public awareness about the main problems in the drug using community.As with the classification of aims, some of these categories could easily be merged orsubdivided, while others might be added. The review undertaken for this chapter suggeststhat additional categories of ‘research’ and ‘user-driven market interventions’ might also beadded.With the same reservations that apply to classifying aims, this list of methods is bestviewed as provisional. It nevertheless provides a framework for some illustrativeexamples from the work of different organisations and activists across Europe. Thecriteria used to select the examples we provide included: geographical diversity;340
Chapter 12: User involvement and user organising in harm reduction
innovative or leading practice; high quality; impact; and, inevitably, our greater personalknowledge of some examples.Advocacy and health/drug policymakingAt the European level, ENCOD is the network with the longest experience of participating inconsultation and dialogue, including: the Civil Society Forum on Drugs; conferences of theEuropean Commission and its sections; hearings and conferences with the EuropeanParliament; and submitting proposals to the European Commission (ENCOD, 2006). In 2007INPUD also began to participate actively in the Civil Society Forum on Drugs, which wasmade possible through the allocation of seats for drug user representatives by IHRA and theCentral and Eastern European Harm Reduction Network (CEEHRN). These are the only twoparticipating organisations with drug users as open members.An ENCOD study of drug users’ organisations and drug policy dialogue found that mostorganisations had experience of dialogue and consultation with local and nationalauthorities. These included one-off or time-limited formal meetings and, in some cases, morestructured, ongoing participation (Montañés Sánchez and Oomen, 2009).In Russia, where the context of drug user activism includes some of Europe’s harshest policiesand laws, drug users’ advocacy contributed to the amendment of more than 200 articles ofthe Penal Code that had effects such as: decriminalising some possession offences;distinguishing manufacture for personal use and commercial distribution (unlike WesternEurope, home production is common among drug users in Russia); and, abolishedcompulsory detention and treatment for the treatment of alcoholism and drug addiction(Canadian HIV/AIDS Legal Network, 2008).The Alliance (originally the Methadone Alliance) is a user-led organisation in the UnitedKingdom, founded in 1998 by Bill Nelles and other supportive professionals. TheAlliance provides advocacy for people receiving drug treatment with an aim to improvethe quality and availability of treatment in the United Kingdom. It has trained advocatesacross most of England who mediate between services and drug users. The Alliance alsotrains other advocates and has contributed extensively to conferences, nationalconsultations, guideline and policy development and other activities, such as steeringgroups for research projects.Aupa’m (Spain) is an informal group of active/ex-drug users and professionals who meet ata weekly assembly to plan work focusing on increasing injecting drug users’ inclusion ascitizens in their community. It has an allied, NGO partner, Asaupam, whose members alsoincludes active/ex-users and which manages the agreed projects. Asaupam has participatedin the design and implementation of local community programmes in two cities of Catalonia,and manages and coordinates the local plans on drugs (including harm reduction,prevention and socio-labour incorporation) in three cities. Asaupam is one of many membersof FAUDAS, a state federation of people affected by drugs or HIV/AIDS (personalcommunication, Carmen Romera and Xavier Pretel, 2009; FAUDAS, 2003).341
Harm reduction: evidence, impacts and challenges
Peer support for people living with HIV/AIDSIn Ukraine, the All Ukrainian Network of People Living with HIV is an umbrella organisation foreight Ukraine-based organisations with drug user members, within which peer support is oneimportant activity (CEEHRN, 2004). It is also illustrative of the way organisations often pursue arange of aims using different methods, as they have also: made prominent national andinternational contributions to combating stigma and discrimination; campaigned for morehumane and effective HIV/AIDS policies/treatment; and been influential in campaigns to pilotmethadone and buprenorphine programmes and their subsequent expansion (Canadian HIV/AIDS Legal Network, 2008). In these respects they have also contributed to the areas of health/drug policymaking, discussed earlier, and to raising public awareness (discussed below).Peer support for drug usersPeer support can be interpreted in numerous ways. Local support groups for specificconcerns other than HIV, such as hepatitis C, are now common, as are Internet-based supportgroups. The impact of peer-driven interventions and peer-based groups has been noted withreference to Europe and Australia (Crofts and Herkt, 1995; Grund and de Bruin, 2007).Within residential rehabilitation programmes that typically operate on some form of‘therapeutic community’ model there is a tradition of involving ex-users to deliver programmesbecause they can sometimes relate to drug users in a way that professional staff cannot, andtheir presence demonstrates that a drug-free life can be achieved (Mold and Berridge, 2008).In Italy, Pazienti Impazienti Cannabis (PIC — Cannabis Impatient Patients) provides acontrasting example (Barriuso, 2001). Starting in 2001, as a group for mutual self-help, itsmembers include people who experience legal or economic problems associated with theiruse of cannabis as a medicine. Beyond providing mutual self-help its aims are to claim therights of patients, and to promote cannabis as part of the botanical heritage of mankindalong with other prohibited plants. As part of its pursuit of practical solutions for access tocannabis as medicine, they use methods including information provision and advocacy. Theirwork has included the clarification of procedures which patients have to follow regarding theimportation of medicinal cannabis and cannabis-derived medicines (2), such as thoseproduced by the Dutch Health Ministry, and their provision through pharmacies, subject tomedical prescription. Under specific circumstances this is paid for by the local health system(Personal communication, Alessandra Viazzi, 2009).HIV and other blood-borne diseases (BBD) education and preventionAccording to Tops (Tops, 2006), the world’s first needle exchange programme was started inAmsterdam in 1984 by the MDHG Belangenvereniging Druggebruikers (Interest Association(2) The legal framework is Article 72 of DPR 309/90, Decree of the Ministry of Health 11/2/1997, Modalita’ diimportazione di specialita’ medicinali registrate all’estero, (G.U. Serie Generale n. 72 del 27 marzo 1997), http://www.normativasanitaria.it/jsp/dettaglio.jsp?attoCompleto=si&id=20747 and D.Lgs 24 April 2006 n 72 paragraph 6.
342
Chapter 12: User involvement and user organising in harm reduction
for Drug Users). Many users’ organisations across Europe now distribute syringes, otherparaphernalia for sterile injecting, and condoms. These include most of the associationsinvolved in the Spanish federation FAUDAS, some Akzept members in Germany, the DanishDrug User Union (BrugerForeningen or BF), and Blue Point in Budapest. Details varyconsiderably in the specific roles, extent and formality of these arrangements and whetherorganisations receive payment.Issue/publish electronic and printed magazines and newslettersDrug users’ organisations produce publications in print and, increasingly, on the Internet.There are numerous examples, some very local and others that address national andinternational issues. Production standards, editorial quality, style and tone also varyconsiderably. Whereas some have a more mainstream harm reduction emphasis, focusing onrisks, harms and their avoidance, others are more overtly politicised and celebrate positivefeatures of a drug-using lifestyle. At IHRA’s conference in 2008, a new international networkwas announced that aims to support drug user organisations with their own publishingprojects — the Drum Alliance (IHRA, 2008).Publications often operate on multiple levels: support; information provision; initiating orpublicising campaigns to change policy, etc. In France, ASUD, a national drug users’organisation that has existed for 15 years, has published 39 editions of its magazine at thetime of writing (Olivet, 2009). The magazine has a distinctly political edge, focusing on themarginalisation, discrimination and lack of rights faced by the majority of French drug users.ASUD has branches in most major French cities and regularly participates in or organisesforms of direct action, such as the recent construction of a symbolic safe consumption room inits Paris office.In England,Black Poppy(O’Mara, 2008) is a widely distributed ‘drug users’ health andlifestyle’ magazine, founded and edited by Erin O’Mara. It includes health and harmreduction information alongside articles on cultural and historical aspects of drug use, useractivism, personal stories and information about services. Individuals and many treatmentagencies subscribe to the magazine and distribute it among their service users. Itsprominence has also enabled its editor to present drug users’ perspectives at parliamentaryadvisory committees and national radio, television and the press.Producing other types of informational materialsBeyond harm reduction’s early focus on HIV prevention among IDUs, users’ organisationshave produced a wide variety of information on: the effects, risks and reduction of harmsfrom specific drugs; the prevention and management of specific hazards, such as overdose orhepatitis C; sexual risks and protection strategies for drug users in general, commercial sexworkers or targeting gay drug users; legal rights if arrested; gaining access to welfarebenefits; and the presence of contaminated batches of drugs. In addition to leaflets orposters, these are disseminated in a range of ways that overlap with the other activities wedescribe elsewhere.343
Harm reduction: evidence, impacts and challenges
Organising, conducting and moderating training, workshops and peer meetingsActivities in this area span highly structured training provision through to informal educationwithin peer meetings. Training was one of the main activities reported among the 16 countriessurveyed by the Central and East European Harm Reduction Network in 2004 (CEEHRN,2004), and training, workshops, seminars and peer meetings with an educational componentof some sort are an almost universal feature of groups’ activity. Content is diverse, reflectingpeople’s needs and concerns, such as: health, harm reduction and treatment information;explanation and skills development to increases users’ capacity to influence local and nationalpolicy processes; and topics such as fund-raising and organisational management.The Spanish Nationwide Network of People Affected by Drugs and HIV (FAUDAS) illustratesthis work. Periodical seminars and formative courses for and, in some cases, by its memberassociations address topics such as computer skills, communication skills, fundraising, harmreduction or the development of harm reduction materials by and for users. There is also apermanent working group on gender and drugs focusing on the situation of female drugusers and most member organisations implement local training for drug users on assortedharm reduction topics (Pretel, 2004).Educational and peer support work in the party sceneThe impact of ecstasy, alongside the wide range of other legal and illegal drugs used byparty-goers, has triggered numerous peer-based initiatives across Europe that focus on theconstantly evolving, free-party, festival and club-based electronic music scenes. Harmreduction activities include: creating and distributing information; providing or assisting inchill out areas; conducting drug checking; and, crisis intervention and support. A usefulguide to peer-based work in this area comes from the Basics Network, which provides anonline guide to organisations across Europe and an extensive downloadable library ofinformation. At the time of writing, they list 22 organisations from 10 countries acrossEurope (BASICS, 2009).Running accommodation projectsIn Spain, Anydes and Comité Ciudadano Antisida de Ourense, both members of the SpanishNationwide Network of People Affected by Drugs and HIV (FAUDAS), run what have beentermed ‘casa de acogida’ (shelters), which are places where people who use drugs can stayfor a certain time and get access to services.Drop-in centres with various servicesDrug users’ organisations have been extensively involved in initiating, developing anddelivering interventions at many levels. Goossens’ (2008) category of ‘drop-in centres withvarious services’ reflects some of these but does not fully indicate the breadth of work that isundertaken.344
Chapter 12: User involvement and user organising in harm reduction
Naloxone distributionIn Catalonia (Spain), Asaupam provide training courses for drug users on how to usenaloxone to as part of efforts to reduce overdose deaths. As part of this, they distributenaloxone to the users participating in the training courses.Methadone distribution‘Guerrilla’ methadone distribution by users’ organisations can be traced back to work in the1980s by the Rotterdam Junkiebond, which led to improved formal methadone maintenance(Grund, n.d.). Today, various users’ organisations within FAUDAS participate in the distributionof methadone at the local level (La Calle, Comité antisida de Ourense). This is done informallyas, legally, the formal dispensing of methadone is only possible through health centres. Inpractice, one person from the association collects the drug in the health centre, and takesresponsibility for dispensing it to the registered clients in their own premises.Drug consumption roomsIn the role of ‘experience experts’, members of drug users’ organisations have contributedto policies that underpin ‘using rooms’ (safer injecting rooms/drug consumption rooms) inthe Netherlands (Tops, 2006). Elsewhere, users’ groups have sometimes implementedclandestine and less formal users’ rooms to provide their community with a more hygienicand safer place.Drug dealing controls on quality and value for moneyIn the Netherlands, a users’ group identified an inconsistency between providing hygienicequipment and space to users when the quality and purity of the substance they are usingvaried, with a potential for harm to arise. This led to the introduction of an ‘in-house dealer’initiative to guarantee the availability and quality of the drug sold and ensure fair prices(Tops, 2006). In the United Kingdom, a peer-led group — The Crack Squad — introduced a‘dealer’s charter’ with similar aims (Carty, 2002).Community reintegrationIn Spain, almost all users’ organisations have programmes assisting drug users in treatmentprogrammes to access the labour market. One example is Engánchate al trabajo (Gethooked by work), run by two FAUDAS member organisations (Asaupam and Arpa ONG).Active drug users engage in community work such as repairing and maintaining urbanspaces or taking care of public gardens. The programme’s goals are to provide workexperience, improve active users’ quality of life and promote more responsible use of drugs.Participants set their own rules to organise and fulfil the work and solve the conflicts that canarise during the implementation. The programme is now in the process of external evaluationand a pilot programme will be implemented in other Spanish cities.345
Harm reduction: evidence, impacts and challenges
Raising public awareness about the main problems in the drug using communitySome of the earliest work in the Netherlands during the late 1970s was concerned withraising public awareness of problems experienced by drug users (Jezek, 2000), and from1982 the Rotterdam Junkiebond presented an hour-long radio show on a popular nationalradio station every Friday evening (Grund, n.d.). We noted above the media work of ErinO’Mara (O’Mara, 2008), and in 2001 Mat Southwell produced a television programme‘Chemical Britannia’, which was broadcast nationally by the BBC (Browne, 2001).Such examples are numerous, but one further example seems especially worthy of mention.In a growing number of countries, users’ groups hold an annual remembrance or memorialday for deceased drug users on 21 July (see also box on p. 339). This originated in Germanymore than ten years ago when the mother of a heroin user who had recently died wanted todraw attention to the poor condition in which many drug users live. In Copenhagen,Denmark a similar event has been held for the last seven years and the United Kingdom alsofollowed suit in 2008. In Australia, similar events are organised to coincide with ‘InternationalDrug Users’ Day’ on 1 November.Often, remembrance events draw attention to issues that contribute to ‘drug-related deaths’,such as deficiencies in service provision, but also the impacts of drug prohibition. They alsoprovide an opportunity for drug users to mark the deaths of friends; this is especiallyimportant as so often drug users die alone and their drug using friends are excluded fromfamily burial services. In this respect the day can serve to raise the consciousness of the drugusing community as a group. As an example, in Copenhagen, after many years ofnegotiations, the city council gave the Danish Drug Users’ Union (BrugerForeningen)permission to install a permanent stone inscribed with the words ‘In memory of dead drugusers’ beside a paradise apple tree. This site acts as a permanent place for users toremember lost friends. As drug policies have sometimes been described as a ‘war on drugs’,many in the user community regard these memorials as remembering those who have diedas the unintended casualties of policies that have exacerbated rather than reduced harm.User-driven market interventionsThe Italian group PIC has already been discussed as a form of peer support for medicalcannabis users, addressing availability and distribution. Initiatives to influence quality and valuefor money of drug purchases through dealers have also been mentioned. Since 2003, ENCODand the Spanish Federation of Cannabis Associations (FAC) have proposed a much wider user-driven, market-level approach: a model for the production and distribution of cannabis foradults’ personal use (ENCOD, 2007; Barriuso, 2007). ENCOD uses the Cannabis Social Club(CSC) model within the wider campaign ‘Freedom to Farm’, which seeks the decriminalisationof the three forbidden plants (opium poppy, coca leaves and cannabis). Originating in Spain,CSCs are non-profit associations whose members are adult cannabis users, most of whom use itrecreationally but with others who do so medicinally. People who enter the club have to fulfilcertain conditions in order to avoid the risk of selling or passing on to third persons or tominors. The CSC members organise a professional, collective cultivation of limited quantities of346
Chapter 12: User involvement and user organising in harm reduction
cannabis to cover the personal needs of their club members and the system is regulated bysecurity and quality checks (Barriuso, 2003, 2005a, 2005b, 2007).The first CSC started in Barcelona, Spain in 2001 (Barriuso, 2005a, p. 163), followed byothers in Catalonia and Basque Country. Further clubs now operate in Spain and another inBelgium. According to Martin Barriuso, president of FAC, this system contributes to thereduction of both risk and harm, since:the uncertainty is often about the quality and possible adulteration of the product purchased onthe black market. In a production system in closed circuit, the partner/s know the quality of whatthey consume, to which variety it belongs, how it has been cultivated, and so on. Furthermore, theassociation can serve as a point of advice and exchange of information, helping to create a newculture of use, which … is essential for true normalization.(Barriuso, 2005a, p. 165)
He also claims that this system prevents minors from accessing the substance and avoids thepossibility of so-called ‘cannabis tourism’ (personal communication, 2009).ResearchKnowledge production, and its use, is often an explicit or implied aim of drug users’organisations. This production of knowledge on and by drug users reflects the approach takenby many other groups seeking civil liberties and human rights historically; notably, women’sstudies, black history, and queer studies. Much research is conducted on drug users. Anincreasing amount takes place with drug users. Research by drug users, who shape or decidethe questions and methods used and are involved at every stage, is the most empoweredposition possible. Internationally, work by the Australian Injecting and Illicit Drug Users League(AIVL) has been at the forefront of discussions about the terms on which drug users are involvedin research and their guidance is a valuable point of reference (AIVL, 2003).ENCOD has made submissions and undertaken surveys that support drug users’ roles, asmembers of civil society, to be participants in all aspects of policymaking that affects their lives— including research. The reportGreen Pepperwas submitted as a response to the EuropeanCommission Green Paper on the Role of Civil Society in Drugs Policy in the European Union, withan historical analysis of the participation of drug users and their role in the drug policy debate atthe European Union level (ENCOD, 2006). A recent survey on the participation of drug userorganisations in the design of drug policies at local and European Level recommended ways toimprove drugs users’ participation and a proposal on how to structure the Civil Society Forum onDrugs of the European Commission (Montañés Sánchez and Oomen, 2009).In the United Kingdom, a number of user activists with academic and other backgrounds haveeither initiated or been invited to be directly involved in research including: the causes anddefinitions of drug related deaths; the Randomised Injectable Opiate Treatment Trial (RIOTT);factors that promote and hinder successful user involvement in drug misuse treatment services;and user involvement in efforts to improve the quality of drug misuse services. There is also a347
Harm reduction: evidence, impacts and challenges
drug user-run research and training company that only employs ex- or current drug users toundertake research on, and of benefit to, the drug using community (led by Mat Southwell).
DiscussionAlthough drug user involvement and organising seems increasingly widespread, we have notedsome of the obstacles facing attempts to document it. Stigma, and the consequences of thecriminalisation of drug use means that many drug users have reason to remain invisible (Robsonand Bruce, 1997). The scarcity of resources to support activism itself means that archiving andpreserving its history is often a subordinate concern, at best. Many key participants, such asNico Adriaans, have died prematurely, taking personal knowledge of this history with them(Grund, n.d.). Nevertheless, one of the clearest messages is that drug users’ organisations havemultiple aims, and use many methods to engage with harm reduction; spanning mainstreampublic health work, through to efforts to amend drug control systems. Although there is ongoingdebate about the place of drug law reform within harm reduction (see Reinarman, 2004), formany drug users’ organisations drug prohibition is without doubt seen as a cause of drug-related harms. The pursuit of drug law reform with the aim of achieving some form of regulateddrug market is therefore perceived as a legitimate harm reduction activity.Besides bringing benefits, user involvement and organising are not without their challenges,including internal conflict (Kerr et al., 2006; Osborn and Small, 2006). Marginalised groupsdo not necessarily possess good knowledge of the way that systems they seek to influencework or the skills needed for establishing and operating their own organisations, especiallyearly in the process. Expectations can also greatly exceed what is deliverable, althoughCrofts and Herkt suggest that these problems are no greater than those found withincommunity development work with other disenfranchised groups (Crofts and Herkt, 1995).Resources commonly fall short of needs, and in many countries funding for drug users’organising is not readily available. One indication of this comes from the CEEHRN needsassessment where drug user groups had noticeably less funding and had access to a smallerrange of donors than people living with HIV/AIDS (CEEHRN, 2004).The extent and nature of state support differs considerably across Europe. For example,England has seen a serious commitment to develop ‘user involvement’ through its NationalTreatment Agency (NTA). User involvement is expected at all levels within treatment systemsand resources are provided to support it. Yet, this has produced tensions that have beennoted elsewhere. For example, critics of the English system, such as the (now defunct)National Drug Users Development Agency (NDUDA), received little support. In just the sameway, Crofts and Herkt have commented on the ‘tension between the funding agencies (stateand federal health departments) for AIDS prevention activities, and the communitydevelopment agenda of the funded groups, which often includes criticism of the policies ofthe funding agencies, especially in relation to drug policy and enforcement’ (Crofts andHerkt, 1995), and Byrne has referred to the problems that can follow groups that developthrough ‘contrived spontaneity’ (Byrne, 2000).348
Chapter 12: User involvement and user organising in harm reduction
ImpactsSetting aside any values-based arguments for thinking it right to properly include affectedpopulations in the decisions and processes that shape their lives, policymakers or others mayask, what is the impact, outcome or benefit of involving drug users and their organisations inthe reduction of drug-related harm? In an analysis of impacts within Europe, Grosso (Grosso, 2008) concludes that drug users’ organisations have produced impacts through peer supportin three areas:• ersonal change, such as more prudent consumption and risk reduction;p• he social normalisation of drug use, by which they mean ‘treating the phenomenon of tdrug use as any other socio-sanitary problem that society takes care of’, and avoiding‘rigid and dichotomous interpretive categories that adopt binaries such as on/off,dependency/abstinence (where) drug use becomes identified totally with “hell” andabstinence with “salvation”’, because ‘scientific evidence has difficulty making headwaywith public opinion and consequently with the institutions that should support it and whichinstead remain paralysed by the generalized opinions of the people they represent’; and• he modification of services, where drug users’ organisations have ‘managed to influence tservices and to make them — at least in part — closer to the needs of their clients, morereceptive to their requirements and more contractual.’The ENCOD survey on the participation of drug user organisations in the design of drugpolicies at local and European level also appraises the impacts of drug users’ organisationson harm reduction as follows:Drug user organisations have contributed with methods to reduce harms and risks from theirorigin. Many of the programmes that are currently carried out by official state programmes (likedrug testing, syringe exchange, opiate prescription, user rooms etc.), form part of claims thathave surged from these organisations themselves, and in some cases, these programmes arebeing elaborated by drug user organisations, who have become more professional by convertingthemselves in service providers. This professionalization has helped to get rid of the stigma ondrug users, demonstrating the fact that they can represent themselves.(Montañés Sánches and Oomen, 2009, p. 220)
In Canada, Thomas Kerr and his colleagues have described the development and impact ofthe Vancouver Area Network of Drug Users (VANDU), and concluded that:Through years of activism, advocacy, and public education, VANDU has repeatedly voiced theconcerns of drugs users in public and political arenas. VANDU has also performed a criticalpublic health function by providing care and support programmes that are responsive toimmediate needs of their peers. This study indicates that greater efforts should be made topromote the formation of drug user organizations, and that health authorities and policy makersshould explore novel methods for incorporating the activities of drug user organizations withinexisting public health, education, and policy making frameworks.(Kerr et al., 2006, p. 61)
349
Harm reduction: evidence, impacts and challenges
In Australia, Crofts and Herkts’ analysis of peer-based groups concluded that:IDUs have organized and, from that, they now successfully run a wide variety of programmesthemselves. IDUs have had a real and often dominant influence on the development of policy inrelation to harm reduction. User groups have run needle distribution and exchange programsthat are among the best in the country; they have produced the most imaginative and appropriateeducational material in this field; they have initiated and actively participated in research; theyhave provided structured access to informants for policy and program development; and havebeen active partners in this development. In general, this has been done with minimal fundingand support, and often in an unsympathetic if not hostile environment. User groups have beenagents of social change who have altered the landscape in relation to every aspect of ourperception of injecting drug use in Australia.(Crofts and Herkt, 1995, p. 614)
Finally, in the reportNothing about us without us(Canadian HIV/AIDS Legal Network,2008), which focuses on the meaningful involvement of people who use illegal drugs inpublic health, the authors conclude:People living with HIV and people who use illegal drugs are central to the response to HIV/AIDSand HCV. There are ethical and human rights imperatives for involvement, but involvement is alsorequired because it ensures a more effective public health response.(Jürgens, 2008, p. 56)
ConclusionKey messages• he way that harm reduction is translated into practice is variable, and so is user involvement Tand user organising.• ser organising implies more autonomous organisation by drug users to work to self-Udetermined agendas affecting their interests, whereas user involvement implies lessautonomy.• n Western Europe, the first drug user advocacy/activist group was the Rotterdam Junkie IUnion, founded in 1977 by Nico Adriaans.• he aims and methods of user-led initiations are multiple and variable, and include: Tpeer support; advocacy and lobbying for improved services and policies; provision ofhelping services; health promotion and user representation; and raising publicawareness.• ser organising occurs in a climate of limited support and resources, yet has had a Usignificant role in generating and sustaining harm reduction responses.• esearch and evaluation on the impacts of user involvement and organising is in its infancy, Rbut is much needed, including through user-led research projects.
350
Chapter 12: User involvement and user organising in harm reduction
We have described the aims and methods evident within drug users’ involvement andorganising, and some evidence of its impact (see box on p. 339). For current and formerdrug users to make their full contribution to harm reduction an enabling environment isrequired, in which their capacity to contribute can develop. The challenges of achieving thisin a context where having a drug user identity is, in effect, criminalised and certainly highlystigmatised, are hard to overstate. Nevertheless, there are two clear ways by which this canbe directly helped.First, any authority that is making decisions or shaping services that affect drug users’ livescan introduce policies that promote or require the meaningful involvement of drug users at allrelevant points, that is, from the very beginning of planning, through to monitoring andevaluation. This has implications at all levels of society, ranging from central government tolocal services. Most obviously, it relates to the planning and delivery of harm reduction anddrug treatment services, but it also relates to the likes of research bodies, housing services,criminal justice services and so forth.The second requirement is for the resources to support this and a corresponding readiness toalter systems in ways that enable drug users’ participation. Becoming ‘involved’ oftengenerates direct costs to the drug user, such as time and travel. It also implies the provision ofthe drug user’s hard-won expertise. These costs should be fairly met. Likewise, systems needto be sensitive to ways they may need to adapt for this to occur successfully. At the sametime, drug users need to recognise that accepting state or other official forms of funding/support may have a real impact on what they can or can’t do, and the way that priorities foraction may be affected.In conclusion, we have tried to illustrate the need for a more nuanced appreciation of thecontribution of drug user involvement and organising to harm reduction and its greaterpotential. In setting out many of its assorted aims and methods, we have alsoacknowledged that there are areas where consensus does not exist among drug users andwithin the harm reduction movement. Finally, we have highlighted ways that userinvolvement and organising can be nurtured, with an expectation that this will supportwider efforts to reduce drug-related harms across Europe.
AcknowledgementsWe would like to express our gratitude to all the people who have assisted us in differentways: Martín Barriuso (FAC, Spain), Jamie Bridge (IHRA, United Kingdom), Walter Cavalieri(Canada), Theo van Dam (Netherlands), Victor Feijoo (FAUDAS), Astrid Forschner (ENCOD/INPUD, Germany), Vito Georgievski (INPUD, Former Yugoslav Republic of Macedonia), Jean-Paul Grund (Netherlands), Joergen Kjaer (BFK, Denmark), Joaquín Laínez (FAUDAS, Spain),Willemijn Loss (MDHG, Netherlands), Joep Oomen (ENCOD), Xavier Pretel and CarmenRomera (FAUDAS, Spain), Jorge Roque (ENCOD, Portugal), Pepe Sánchez and AntonioEscobar (Federación ENLACE, Spain), Anya Sarang (Russia), Dirk Schäffer (JES, Germany),Iker Val (FAC, Spain) and Alessandra Viazzi (PIC, Italy). Any mistakes, omissions or errorsare, nevertheless, entirely the responsibility of the authors.351
Harm reduction: evidence, impacts and challenges
ReferencesAIVL (Australian Injecting and Illicit Drug Users League) (2003),A national statement on ethical issues for researchinvolving injecting/illicit drug users,Australian Injecting and Illicit Drug Users League, Canberra.Anker, J., Asmussen, V., Kouvonen, P. and Tops, D. (2008), ‘Drug users and spaces for legitimate action’, inBröring, G. and Schatz, E. (eds),Empowerment and self-organisations of drug users: experiences and lessons learnt,Foundation Regenboog AMOC, Amsterdam.Balian, R. and White, C. (1998), ‘Defining the drug user’,International Journal of Drug Policy9, pp. 391–6.Barriuso, M. (2001), ‘La visión del movimiento asociativo cannábico’, in Grup Igia (ed.),Gestionando las drogas,Publicaciones del Grup Igia, Barcelona, pp. 81–9.Barriuso, M. (2003), ‘La prohibición de drogas, el tabú moral a la desobediencia civil’, in Arana, X., Husak, D.and Scheerer, S. (eds),Globalización y drogas. Políticas sobre drogas, derechos humanos y reducción de riesgos,Dykinson, Instituto Internacional de Sociología Jurídica de Oñati, Madrid, pp. 83–117.Barriuso, M. (2005a) ‘Propuesta de modelo legal para el cannabis en el Estado español’, Eguzkilore.Cuadernodel Instituto Vasco de Criminología19, pp. 151–68.Barriuso, M. (2005b), ‘Adiós al guetto: el discreto encanto de la normalidad’,Revista Española dedrogodependencias30 (1–2), pp. 206–12.Barriuso, M. (2007), ‘Más allá de las excusas: hacia una regulación legal no prohibicionista para el cannabis’,in Pantoja, L. (ed.),Hablemos del cannabis. Avances en drogodependencias,Universidad de Deusto, Bilbao, pp.107–32.BASICS (2009), ‘Basics Network’. Available at http://www.basics-network.org/ (accessed 7 September 2009).Bröring, G. and Schatz, E. (eds) (2008),Empowerment and self-organisations of drug users: experiences and lessonslearnt,Foundation Regenboog AMOC, Amsterdam.Browne, A. (2001), ‘Heroin is safe and fun, says shock BBC show’,Guardian25 March. Available at http://www.guardian.co.uk/uk/2001/mar/25/drugsandalcohol.anthonybrowne (accessed 12 June 2009).Byrne, J. (2000), ‘Done to, done over, doing it for ourselves: the history of the drug users movement’,Black Poppy.Available at http://www.blackpoppy.org.uk/blackpoppy/highlights_ourselves.htm (accessed 8 September2009).Canadian HIV/AIDS Legal Network, (2008),‘Nothing about us without us’ — greater, meaningful involvement ofpeople who use illegal drugs: a public health, ethical, and human rights imperative, Eastern Europe and Central AsiaEdition.Available at http://www.aidslaw.ca/publications/interfaces/downloadFile.php?ref=1351 (accessed 16June 2009).Carty, P. (2002), ‘Caned and able’,Guardian,30 May 2002. Available at http://www.guardian.co.uk/lifeandstyle/2002/may/30/healthandwellbeing.health1 (accessed 12 June 2009).CEEHRN (Central and Eastern European Harm Reduction Network) (2004),Self-organization of drug users andpeople living with HIV/AIDS in Central and Eastern Europe and Central Asia: needs assessment report,Central andEastern European Harm Reduction Network, Vilnius.Correlation (2009), ‘Correlation: European network social inclusion and health’. Available at http://www.correlation-net.org (accessed 7 September 2009).Crofts, N. and Herkt, D. (1995), ‘A history of peer-based drug-user groups in Australia’,Journal of Drug Issues25,pp. 599–616.
352
Chapter 12: User involvement and user organising in harm reduction
Efthimiou-Mordaunt, A. (2005), ‘Junkies in the house of the Lord’, Masters Dissertation, Department of SocialPolicy and Planning, London School of Economics, London. Available at http://www.canadianharmreduction.com/readmore/Andrias+MSc+Dissertation.pdf (accessed 12 June 2009).EMCDDA (2008),Annual report 2008: the state of the drugs problem in Europe,European Monitoring Centre forDrugs and Drug Addiction, Lisbon.ENCOD (European Coalition for Just and Effective Drug Policies) (2006),Green pepper: on the role of civil societyin drug policy in the European Union,European Commission, Antwerpen.ENCOD (2007),Cannabis social clubs,Draft to the Project, ENCOD. Available at http://www.encod.org/info/test.html (accessed 26 November 2009).FAUDAS (2003) Website available at http://www.faudas.org (accessed 7 September 2009).Fischer, J. and Jenkins, N. (2007),Drug user involvement in treatment decisions,Joseph Rowntree Foundation, York.Foster, J., Tyrell, K., Cropper, V. and Hunt, N. (2007), ‘Two case studies of user involvement in the recruitment ofstaff for drug services’,Drugs: Education, Prevention and Policy14, pp. 89–94.Friedman, S. (1996), ‘Theoretical bases for understanding drugs users’ organizations’,International Journal ofDrug Policy7, pp. 212–19.Friedman, S. (1998), ‘The political economy of drug-user scapegoating and the philosophy and politics ofresistance’,Drugs: Education, Prevention, and Policy5, pp. 15–32.Goossens, S. (2008), ‘Drug user activism: an overview’, in Bröring, G. and Schatz, E. (eds),Empowerment andself-organisations of drug users: experiences and lessons learnt,Foundation Regenboog AMOC, Amsterdam, pp.117–24.Grosso, L. (2008), ‘Empowerment — models of good practice: heroin use and peer support. What lessons havebeen learnt?’ in Bröring, G. and Schatz, E. (eds),Empowerment and self-organisations of drug users: experiencesand lessons learnt,Foundation Regenboog AMOC, Amsterdam, pp. 41–55.Grund, J. P. (n.d.), ‘Letter for Nico’. Available at http://www.ibogaine.desk.nl/adriaans.html (accessed 30 May2009).Grund, J. P. and Bruin D. de (2007), ‘BeyondHIV: the peer driven intervention and empowerment of vulnerablepopulations’,Plenary presentation at Correlation Conference, Social Inclusion and Health – Crossing the Borders,Sofia, Bulgaria, 27–29 September.Hunt, N., Ashton, M., Lenton, S., et al. (2003), ‘A review of the evidence-base for harm reduction approaches todrug use’, Forward Thinking on Drugs/Release, London. Available at http://www.ihra.net/Assets/23/1/HIVTop50Documents11.pdf (accessed 12 June 2009).ICN (1998), ‘Manifesto for just and effective drug policies’. Available at http://www.encod.org/info/MANIFESTO-FOR-JUST-AND-EFFECTIVE.html (accessed 13 January 2010).IHRA (International Harm Reduction Association) (2008), ‘19th International Harm reduction Conference,Barcelona 2008. Daily update: 14th May 2008.’ Available at http://www.ihra.net/Assets/134/1/2008_DailyUpdate_Wednesday14thThursday15th.pdf (accessed 27 January 2010).INPUD (International Network of People who Use Drugs) (2006) ‘Why the world needs an international networkof activists who use drugs’, INPUD. Available at http://hardcoreharmreducer.be/VancouverDeclaration.html(accessed 27 January 2010).Jezek, R. (2000),Right to use: drug users and their representatives,René de Milliano/LSD, Alkmaar.
353
Harm reduction: evidence, impacts and challenges
Jürgens, R. (2008),‘Nothing about us without us’ — greater, meaningful involvement of people who use illegal drugs:a public health, ethical, and human rights imperative, international edition,Canadian HIV/AIDS Legal Network,International HIV/AIDS Alliance, Open Society Institute, Toronto.Kerr, T., Small, W., Peeace, W., et al. (2006), ‘Harm reduction by a “user-run” organization: a case study of theVancouver Area Network of Drug Users (VANDU)’,International Journal of Drug Policy17, pp. 61–9.Mold, A. and Berridge, V. (2008), ‘The rise of the user? Voluntary organizations, the state and illegal drugs inEngland since the 1960s’,Drugs: Education, Prevention and Policy15, 451–61.Montañés Sánchez, V. and Oomen, J. (2009),Use of drugs and advocacy: a research into the participation of druguser organisations in the design of drug policies on a local and European level,Servicio Central de Publicacionesdel Gobierno Vasco, Vitoria-Gasteiz.Museummouse (2008), ‘Harm reduction. Oh yea, it’s history!’, Cannabis Culture Forums. Available at http://forums.cannabisculture.com/forums/ubbthreads.php?ubb=showflat&Number=1436231 (accessed 12 June2009).Newcombe, R. (1992), ‘The reduction of drug related harm: a conceptual framework for theory, practice andresearch’, in O’Hare, P. (ed.),The reduction of drug related harm,Routledge, London.O’Mara, E. (2008),Black Poppy.Available http://www.blackpoppy.org.uk/ (accessed 16 June 2009).Olivet, F. (2009), ASUD website. Available at http://www.asud.org (accessed 16 June 2009).Osborn, B. and Small, W. (2006), ‘Speaking truth to power: the role of drug users in influencing municipalpolicy’,International Journal of Drug Policy17, pp. 70–2.Pretel, X. (2004), ‘FAUDAS, Federación Estatal de Asociaciones de Usuarios y grupos afines’,XV JornadasAndaluzas de Asociaciones de Drogodependencia y Sida.Federación Andaluza de Drogodependencias y Sida(ENLACE), Chiclana.Pretel, X. (2007), ‘FAUDAS: a process to develop formative, participation and advocacy skills in the communityof people affected by drugs’, Antiretroviral Treatment for Injecting Drug Users (ARV4IDUs) Seminar, Vilnius,Lithuania.Reinarman, C. (2004), ‘Public health and human rights: the virtues of ambiguity’,International Journal of DrugPolicy15, 239–41.Robbins, C. (2004), ‘Secrets in the work place’, MSc Dissertation, Imperial College, London.Robson, P. and Bruce, M. (1997), ‘A comparison of “visible” and “invisible” users of amphetamine, cocaine andheroin: two distinct populations?’Addiction92 (12), pp. 1729–36.Schäffer, D. and Hentschel, A. (2004), ‘Förderung der Drogenselbsthilfe’, in Klee, J. and Stöver, H. (eds),Drogen— HIV/AIDS — Hepatitis. Ein Handbuch,Deutsche AIDS-Hilfe, Berlin, pp. 40–52.Tops, D. (2006), ‘Stretching the limits of drug policies: an uneasy balancing act’, in Anker, J., Asmussen, V.,Kouvonen, P. and Tops , D. (eds),Drug users and spaces for legitimate action,Nordic Centre for Alcohol and DrugResearch, Helsingfors.van Dam, T. (2008), ‘Users unite: a brief overview about the drug user movement’, in Bröring, G. and Schatz E.(eds),Empowerment and self-organisations of drug users: experiences and lessons learnt,Foundation RegenboogAMOC, Amsterdam.Zibbell, J. E. (2004), ‘Can the lunatics actually take over the asylum? Reconfiguring subjectivity and neo-liberalgovernance in contemporary British drug treatment policy’,International Journal of Drug Policy15, pp. 56–65.
354
Chapter 13Young people, recreational drug use and harm reductionAdam Fletcher, Amador Calafat, Alessandro Pirona and Deborah Olszewski
AbstractThis chapter begins by reviewing the prevalence of recreational drug use and relatedadverse health outcomes among young people in European countries. It then employs atypological approach to review and discuss the current range of responses that aim to reducethe harms associated with young people’s recreational drug use in Europe. These responsesinclude: individually focused and group-based interventions (school-based drugs educationand prevention, mass media campaigns, motivational interviewing, and youth developmentprogrammes) and ‘settings-based approaches’, which make changes to recreational settings,such as nightclubs, or institutional settings, such as schools, to address the social andenvironmental background of young people’s drug use.Keywords:young people, drug use, prevalence, harm, intervention, Europe.
IntroductionThis chapter focuses primarily on young people’s use of illegal drugs (rather than alcohol andtobacco use). However, the potential for harm is likely to be greatest when young people useboth drugs and alcohol, and many of the interventions reviewed in this chapter areconsidered to be appropriate for reducing the harms associated with both drug and alcoholuse. The chapter will begin by reviewing the prevalence of drug use among young people inEurope and the related adverse health and other harms. The appropriateness and likelyeffectiveness of different types of interventions that aim to reduce the harms associated withyoung people’s recreational drug are then discussed. Harm reduction has traditionallyfocused on adult ‘problem’ drug users, particularly injecting drug users (see, for example,Ball, 2007, and Kimber et al., 2010), and neglected not only the harms associated with youngpeople’s recreational drug use but also how to reduce these harms.This chapter considers young people’s recreational drug use to be drug use that occurs forpleasure, typically with friends, in either formal recreational settings, such as nightclubs, and/or informal settings, such as on the streets and in the home. This is thus a broader definitionthan the one applied in other EMCDDA publications, which often focus specifically on youngpeople’s drug use within a ‘nightlife context’ (e.g. EMCDDA, 2002). This chapter is primarilyfocused on young people aged 14–19, although some studies report on other age ranges(e.g. 14–24) and therefore at times it has been necessary to define ‘young people’ morebroadly. Furthermore, data on prevalence and trends of drug use among young people oftenaim to provide an indication of overall levels of use and therefore do not always distinguishbetween recreational drug use and more problematic patterns of use.357
Harm reduction: evidence, impacts and challenges
Trends in young people’s recreational drug use in EuropeThe European School Survey Project on Alcohol and Other Drugs (ESPAD) and recentgeneral population surveys have revealed lower prevalence of use of cannabis and otherillicit drugs for European youth compared to youth in the United States (Hibell et al., 2004;Hibell et al., 2009; EMCDDA, 2009). However, these overall European-level data maskdiversity within the EU in terms of young people’s use of cannabis, ‘club drugs’, such asecstasy and amphetamines, and cocaine.CannabisThe 2007 ESPAD data revealed that the highest lifetime prevalence of cannabis use among15- to 16-year-old school students is in the Czech Republic (45 %), while Estonia, France, theNetherlands, Slovakia and the United Kingdom reported prevalence levels ranging from26 % to 32 % (Hibell et al., 2009). Lifetime prevalence levels of cannabis use of between 13 %and 25 % are reported in 15 other countries. Less than 10 % of 15- to 16-year-old schoolstudents report cannabis use in Greece, Cyprus, Romania, Finland, Sweden and Norway.Early onset of cannabis use has been associated with the development of more intensive andproblematic forms of drug consumption later in life. In most of the 10 EU countries withrelatively high prevalence of frequent use, between 5 % and 9 % of school students hadinitiated cannabis use at age 13 or younger. In addition, compared to the general populationof students, cannabis users are more likely to use alcohol, tobacco and other illicit drugs(EMCDDA, 2009).National survey data reported to the EMCDDA shows that in almost all EU countriescannabis use increased markedly during the 1990s, in particular among school students. By2003, between 30–40 % of 15- to 34-year-olds reported ‘lifetime use’ of cannabis in sevencountries, and more than 40 % of this age group reported ever having used cannabis in twoother countries. However, data from the 2007 ESPAD surveys suggests that cannabis use isstabilising — and in some cases declining — among young people in Europe: of the 11 EUcountries for which it is possible to analyse trends between 2002 and 2007, four countriesshowed overall decreases of 15 % or more in the proportion of 15- to 16-year-olds reportingcannabis use in the last year, and in four other countries the situation appears stable (Hibellet al., 2009; EMCDDA, 2009).Ecstasy and amphetaminesIt is estimated that 7.5 million young Europeans aged 15 to 34 (5.6 %) have ever triedecstasy, with around 2 million (1.6 %) using it during the last year (EMCDDA, 2009).Estimates of prevalence are generally even higher among the subgroup of 15- to 24-year-olds, for whom lifetime prevalence ranges between 0.4–18.7 % in European countries(estimates fall between 2.1 % and 6.8 % in most European countries). Among 15- to 16-year-old students lifetime prevalence of ecstasy use ranges between 1 % and 7 % in countriessurveyed in 2007 (EMCDDA, 2009).358
Chapter 13: Young people, recreational drug use and harm reduction
Studies of recreational settings that are associated with drug use, such as dance events ormusic festivals, provide further evidence regarding young people’s ecstasy andamphetamine use. Estimates of young people’s drug use in these settings are typically high.However, comparisons between surveys can only be made with the utmost caution, as theage and gender distribution of survey respondents as well as variations in the setting maylead to observed differences. Studies conducted in recreational settings in 2007 in five EUcountries (Belgium, Czech Republic, Latvia, Lithuania, Austria) reveal lifetime prevalenceestimates of 15–71 % for ecstasy use and 17–68 % for amphetamines (EMCDDA, 2009).Much of party-going young people’s drug use occurs on weekends and during holidayperiods (EMCDDA, 2006b).Figure 13.1:Proportion of 16- to 24-year-olds reporting use of the most prevalent drugs in the lastyear by frequency of nightclub visits
40
No visits to a nightclub in the last monthOne to three visits to a nightclub in the last month
30
Four or more visits to a nightclub in the last monthAll aged 16–24
20
%
10
0
Cannabis
Any cocaine
Amyl nitrite
Ecstasy
Source:Hoare and Flatley, 2008.
A further indication of the extent to which the use of these drugs may be concentratedamong the young, club-going population can found in the 2007/8 British Crime Survey(Hoare and Flatley, 2008). The study found that those 16- to 24-year-olds who reportedvisiting a nightclub four or more times in the last month were more than three times aslikely to have used ecstasy in the last year than those not attending nightclubs (2 % vs.8 %) (Figure 13.1). In a French study that was carried out in 2004 and 2005 among 1 496young people at ‘electronic’ music venues, 32 % of respondents reported ecstasy use and13 % reported amphetamine use in the past month (Reynaud-Maurupt et al., 2007).Among specific sub-populations that self-identified as ‘alternative’, prevalence estimatesfor ecstasy and amphetamines were as high as 54 % and 29 %, respectively (Reynaud-Maurupt, 2007).359
Harm reduction: evidence, impacts and challenges
CocaineAlthough cocaine is the second most commonly used illicit drug in Europe after cannabis(EMCDDA, 2007), estimates of the prevalence of cocaine use among school students are verylow. Lifetime prevalence of cocaine use among 15- to 16-year-old students in the ESPADsurvey is between 1 % and 2 % in half of the 28 reporting countries, and in the rest it rangesbetween 3 % and 5 % (Hibell et al., 2009; EMCDDA, 2009).of the data
Table 13.1:Prevalence of cocaine use in the young adult population — summaryTime frame of useAge group15–34 yearsEstimated number ofusers in EuropeEuropean averageRangeLowest-prevalencecountries7.5 million5.6 %0.1–12.0 %Romania (0.1 %)Lithuania (0.7 %)Malta (0.9 %)Greece (1.0 %)United Kingdom(12.0 %)Spain (11.8 %)Denmark (9.5 %)Ireland (8.2 %)3 million4.4 %0.1–9.9 %Romania (0.1 %)Greece (0.6 %)Lithuania (0.7 %)Malta, Poland (1.1 %)United Kingdom(9.9 %)Spain (9.3 %)Denmark (9.2 %)Ireland (7.0 %)3 million2.2 %0.1–5.5 %Romania (0.1 %)Greece (0.2 %)Poland (0.3 %)Hungary, CzechRepublic (0.4 %)Spain (5.5 %)United Kingdom(4.5 %)Denmark (3.4 %)Ireland, Italy (3.1 %)1.5 million2.2 %0.1–5.6 %Romania (0.1 %)Greece (0.2 %)Poland (0.3 %)Czech Republic(0.4 %)Denmark (5.6 %)Spain (5.4 %)United Kingdom(5.0 %)Ireland (3.8 %)1 million0.8 %0.0–2.1 %Estonia, Romania(0.0 %)Czech Republic,Greece, Poland(0.1 %)United Kingdom(2.1 %)Spain (1.9 %)Italy (1.2 %)Ireland (1.0 %)0.6 million0.9 %0.0–2.5 %Estonia, Romania(0.0 %)Greece (0.1 %)Czech Republic, Poland,Portugal (0.2 %)United Kingdom(2.5 %)Spain (1.7 %)Italy (1.2 %)Ireland (1.1 %)
Lifetime
Last year
Last month
Highest-prevalencecountries
15–24 yearsEstimated number ofusers in EuropeEuropean averageRangeLowest-prevalencecountries
Highest-prevalencecountries
Note: European prevalence estimates are based on weighted averages from the most recent national surveys conductedfrom 2001 to 2008 (mainly 2004–08), therefore they cannot be attached to a single year. The average prevalence forEurope was computed by a weighted average according to the population of the relevant age group in each country. Incountries for which no information was available, the average EU prevalence was imputed. Population base is 133 million.The data summarised here are available under ‘General population surveys’ in the EMCDDA 2009 statistical bulletin.Source:EMCDDA, 2009.
360
Chapter 13: Young people, recreational drug use and harm reduction
Of the 4 million Europeans who used cocaine in the past year, around 3 million were youngpeople and young adults (EMCDDA, 2009). The prevalence of past-year cocaine use among15- to 24-year-olds is estimated to be 2.2 %, which translates to about 1.5 million cocaineusers. In contrast to the prevalence estimates for cannabis or ecstasy use, which are highestamong the 15 to 24 age group, measures of more recent cocaine use (last year and lastmonth) are similar among the 15 to 24 and 25 to 34 age groups (see Table 13.1). Of the 11countries for which it is possible to analyse trends in cocaine use between 2002 and 2007,the proportion of 15- to 34-year-olds reporting cocaine use in the last year increased by15 % or more in five countries (Ireland, Italy, Latvia, Portugal, United Kingdom), remainedstable in four (Germany, Spain, Slovakia, Finland) and only decreased in two countries(Hungary, Poland).Cocaine use is also strongly associated with alcohol use. For example, the British CrimeSurvey 2007–08 found that among 16- to 24-year-olds who made nine or more visits to apub in the last month, 13.5 % reported using cocaine in the last year, compared to 1.7 %among those who had not visited a pub (Hoare and Flatley, 2008). Visiting nightclubs wasalso associated with higher cocaine use, as nearly 10 % of the 16- to 24-year-olds whovisited a club on four or more occasions during the last month reported using cocaine in thelast year, compared to 3.3 % among those who had not visited a club (Hoare and Flatley,2008). Studies conducted in nightlife settings also report higher prevalence of cocaine useamong club-goers than among the general population (EMCDDA, 2007).It is worth noting that alcohol is almost always the first drug with strong psychoactive andmind-altering effects used by young people, and its widespread availability makes it themain drug connected to poly-drug use among young adults, particularly in recreationalsettings. Other psychoactive substances commonly referred to as ‘legal highs’ areincreasingly sold as alternatives to controlled drugs. In 2009, a snapshot study of 115online shops located in 17 European countries showed that a range of herbal smokingproducts and ‘party pills’ containing legal alternatives to controlled drugs were being sold(EMCDDA, 2009).
Health and other harmsIt is now widely acknowledged that recreational drug use can be an important source ofstatus and recreation for young people (Henderson et al., 2007); it can not only facilitate ashared sense of group belonging and security (Fletcher et al., 2009a), but also a sense ofbeing different from other groups of young people (Shildrick, 2002). However, asrecreational drug use has increased among different sections of the youth population, so hasevidence of drug-related harm and concerns about the consequences of adolescent drug use.Although the vast majority of this increase in drug use among young people has beenattributed to the use of ‘soft’ drugs (e.g. cannabis and ecstasy), these substances still havehealth risks, especially for frequent users who are most at risk of harm.Cannabis can cause short- and long-term health problems, such as nausea, anxiety, memorydeficits, depression and respiratory problems (Hall and Solowij, 1998; MacLeod et al., 2004;361
Harm reduction: evidence, impacts and challenges
Solowij and Battisti, 2008; Hall and Fischer, 2010). Although more research is needed on thelong-term effects of adolescent cannabis use on mental health, cannabis use is also thoughtto increase the risk of mental health problems, particularly among frequent users (Hall, 2006;Moore et al., 2007) and those with a predisposition for psychosis (Henquet et al., 2005).Regular cannabis users can also become dependent (Melrose et al., 2007).The true extent of future mental health problems due to adolescent ecstasy use is unclear, butyoung ecstasy users may be at risk of depression in later life and there is evidence thatecstasy use may also impair cognitive functions relevant to learning (Parrott et al., 1998;Schilt et al., 2007). Dehydration, a more immediate risk for ecstasy users, can cause loss ofconsciousness, coma and even death. Furthermore, evidence from cohort studies suggeststhat early initiation and frequent use of ‘soft’ drugs may be a potential pathway to moreproblematic drug use in later life (Yamaguchi and Kandel, 1984; Lynskey et al., 2003;Ferguson et al., 2006).Cocaine use can result in dependence and/or serious mental and physical health problems,such as depression, paranoia, and heart and respiratory problems (Emmett and Nice, 2006).Hence, although only a small minority of young people use cocaine (NatCen and NFER,2007; Hibell et al., 2009), their numbers are increasing in some countries in Europe, posingan increasing public health issue.In addition to presenting direct health risks, adolescent drug use is also associated withaccidental injury, self-harm, suicide (Charlton et al., 1993; Beautrais et al., 1999; Thomas etal., 2007) and other ‘problem’ behaviours, such as unprotected sex, youth offending andtraffic risk behaviours (Jessor et al., 1991; Home Office, 2002; Jayakody et al., 2005; Calafatet al., 2009). For example, a recent report by the United Kingdom Independent AdvisoryGroup on Sexual Health and HIV (2007) has suggested that there are strong links betweendrug use, ‘binge’ drinking and sexual health risk, with similar trends in these risk behaviours.Furthermore, although the links between crime and heroin or cocaine dependence are wellknown, there is increasing evidence of links between teenage cannabis use and youthoffending (e.g. Boreham et al., 2006). This is not to say that there is necessarily a directcausal relationship between adolescent drug use and social problems, but there is clearevidence that they cluster together among certain groups of young people.
A typology of interventionsThere have been surprisingly few attempts to synthesise the evidence relating to interventionsin European countries addressing young people’s recreational drug use. Here we adopt atypological approach to describe and discuss responses that aim to reduce the harmsassociated with young people’s recreational drug use. These include: (1) individually focusedand group-based interventions — school-based drugs education and prevention, massmedia campaigns, motivational interviewing and youth development programmes — and (2)‘settings-based approaches’ which make changes to recreational settings, such as nightclubs,or institutional settings, such as schools, to address the social and environmental backgroundof young people’s drug use.362
Chapter 13: Young people, recreational drug use and harm reduction
This is not an exhaustive list of interventions in Europe that target young people’s recreationaldrug use. For example, we do not discuss interventions that are directed primarily at youngpeople’s parents rather than young people themselves (see Petrie et al., 2007 for a review ofthe evidence relating to current parenting programmes). Social policies that may impact onmacro-social — or ‘structural’ — factors, such as youth cultures, poverty or social exclusion,that are also associated with young people’s drug use, are also not discussed, because theyrarely aim to specifically reduce the harms associated with recreational drug use. Thedecriminalisation of drugs, drug classification policies, and policies and enforcement toreduce the supply of illicit drugs and illicit sales of prescription drugs are also beyond thescope of this chapter.Individual and group-based approachesSchool-based drugs education and preventionIn Europe, schools provide universal access to young people under 16 and are widelyrecognised as a key site for drugs education and prevention interventions that aim to preventor delay drug use and reduce the frequency of drug use during adolescence (Evans-Whippet al., 2004). However, evidence from randomised controlled trials (RCTs) of classroom-baseddrugs education interventions aiming to improve knowledge, develop skills and modify peernorms suggest that the effect of these interventions on young people’s drug-use behaviour arelimited: a recent systematic review found that they can have positive effects but concludedthat these are small, inconsistent and generally not sustained (Faggiano et al., 2005). In otherwords, drugs education may promote students’ ‘health literacy’ but is not sufficient on its ownfor changing young people’s behaviour or reducing drug-related harms.Faggiano and colleagues (2005) found that school-based drugs education programmesbased on a ‘comprehensive social influence approach’ and those that are delivered by otherstudents (rather than teachers) appear to have the most positive effects — programmecharacteristics that were also associated with more positive effects in systematic reviews ofalcohol education and smoking prevention interventions in schools (Foxcroft et al., 2002;Thomas and Perera, 2006). However, in reviewing the evidence for drug educationprogrammes in schools, Cahill (2007) has highlighted the difficulties of implementingcomplex interventions such as peer-led programmes in school settings and suggested thatcaution is also required with normative education to ensure that adolescents receiveappropriate messages.A key challenge in Europe and elsewhere is therefore to pilot and further evaluate evidence-based school-based drugs education and prevention interventions (Faggiano and Vigna-Taglianti, 2008; Ringwalt et al., 2008). ‘Unplugged’ is an example of a European school-based programme that employs a comprehensive social influence model. It aims to reduceyoung people’s substance use via 12 interactive sessions addressing topics such as decision-making, ‘creative thinking’, effective communication, relationship skills, self-awareness,empathy, coping skills and the risks associated with specific drugs (Van Der Kreeft et al.,2009). A recent cluster RCT of the ‘Unplugged’ programme in 170 schools across seven363
Harm reduction: evidence, impacts and challenges
European countries suggested that curricula based on such a comprehensive social-influencemodel are not only feasible to implement in schools in Europe, they may also reduce regularcannabis use and delay progression to daily smoking and episodes of drunkenness(Faggiano et al., 2008).The ASSIST (A Stop Smoking in Schools Trial) programme in the United Kingdom provides anexample of an effective peer-led health promotion intervention that is feasible to deliver inschools: a cluster RCT of the ASSIST programme involving 59 schools in Wales found asignificant reduction in smoking among the intervention group, including among the most‘high risk’ groups of students (Campbell et al., 2008). The programme uses network analysisto identify influential students and train them as peer supporters to ‘diffuse’ positive healthmessages throughout the school. Researchers at the Centre for Drug Misuse Research inGlasgow have recently piloted a peer-led drugs prevention programme based on the ASSISTprogramme in two secondary schools in Scotland; this study suggested that it is feasible todeliver cannabis and smoking education (CASE) together using this approach (Professor MickBloor, personal communication). However, further research is needed to examine the effectsof this intervention on students’ drug use and drug-related harms.Mass media campaignsMass media campaigns have become a popular tool among health promoters seeking toinform young people about the risks associated with recreational drug use and/or seeking toencourage current users to reduce their use and minimise the risk of harm. Theseinterventions, such as the recent United Kingdom FRANK advertising campaigns on themental health problems associated with recreational cannabis use (http://www.talktofrank.com/cannabis.aspx), aim to increase the information available to young people and reframeissues relating to young people’s recreational drug use on public health terms. These massmedia campaigns to raise awareness about the effects of drug use in the United Kingdomhave also been integrated with a ‘credible, non-judgemental and reliable’ online andtelephone drugs advice and information service for young people and their parents (HomeOffice et al., 2006).However, mass media campaigns that aim to reduce the harms associated with youngpeople’s recreational drug have rarely been evaluated to examine their effects on youngpeople’s behaviour, attitudes or intention to use drugs — and where they have, the findingshave not always been positive. A national survey to evaluate the United States Anti-DrugMedia Campaign suggested that mass media campaigns have little or no effect on changingattitudes once young people have initiated drug use (Orwin et al., 2006), and may evenhave harmful effects as those young people who were exposed to the adverts were morelikely to report cannabis use or an intention to use cannabis (Hornik et al., 2008). Similarnegative outcomes were reported in another large-scale evaluation of the Scottish cocainecampaign ‘Know the score’: two-fifths (41 %) of respondents said that the campaign madethem more likely to find out more about cocaine and 12 % felt that the campaign had madethem more likely to experiment with cocaine (Phillips and Kinver, 2007). A meta-analysis ofevaluations of mass media campaigns to reduce smoking, drinking or drug use by Derzon364
Chapter 13: Young people, recreational drug use and harm reduction
and Lipsey (2002) found that campaigns featuring messages about resistance skills appearedto have the most harmful effects and were associated with significantly higher extent ofsubstance use than observed in control communities.Flay and colleagues (1980) have suggested that the key factors to change behaviour viamass media health promotion campaigns include: repetition of information over long timeperiods, via multiple sources and at different times (including ‘prime’ or high-exposure times).Mass media interventions also provide the opportunity to reach specific target groups withina short timeframe (HDA, 2004). However, population-level mass media campaigns require asignificant financial investment (Hornik, 2002) and are competing in an increasingly crowdedmarket with a range of other information available to young people (Randolph andViswanath, 2004).Brief interventionsApproaches based on early screening of young people’s drug use and brief behaviour changeinterventions, such as motivational interviewing, have been rigorously evaluated in the UnitedKingdom and elsewhere (Tait and Hulse, 2003; Tevyaw and Monti, 2004). Developed by Millerand Rollnick, motivational interviewing has been defined as a ‘client-centred, directive methodfor enhancing intrinsic motivation to change by exploring and resolving ambivalence’ (Millerand Rollnick, 2002). Evidence suggests that it is feasible to deliver brief one-to-one interventionssuch as motivational interviewing to young drug-users in a wide range of settings, such asyouth centres, further education colleges, general practitioners’ surgeries and ‘emergencyrooms’ (Gray et al., 2005; Martin et al., 2005; McCambridge et al., 2008), and where briefinterventions employ motivational interviewing principles they have been found to be effectivein reducing young people’s drug use (Tait and Hulse, 2003; McCambridge and Strang, 2004;Tevyaw and Monti, 2004; Grenard et al., 2006).Reviewing the evidence from trials of brief motivational interviewing interventions, Tevyawand Monti (2004) found consistent evidence that this approach can ‘result in decreases insubstance-related negative consequences and problems, decrements in substance use andincreased treatment engagement’, and these effects appear to be greatest among youngpeople who report the heaviest patterns of drug use and the least motivation to change priorto intervention. Researchers have also found evidence that as little as a ‘single session’ ofmotivational interviewing can significantly reduce cannabis use among heavy users andamong those young people considered to be at ‘high risk’ of progressing to moreproblematic drug use (McCambridge and Strang, 2004).However, the existing evidence suggests that, although brief interventions based onmotivational interviewing can encourage young people to moderate their drug use in theshort term, this approach is unlikely to have long-term effects on its own (McCambridge andStrang, 2005) and may therefore need to form part of a more holistic approach to harmreduction. Further research is also needed to examine the essential elements of motivationalinterviewing interventions and their effects on developmental transitions during adolescence(McCambridge and Strang, 2004; McCambridge et al., 2008). Furthermore, motivational365
Harm reduction: evidence, impacts and challenges
interviewing is complex and requires practitioners to develop skills and experiences over timein order to deliver it proficiently. As such, it is likely to be difficult to replicate and evaluateexisting intervention more widely across Europe at present while is there is limited capacity todeliver such interventions.Youth developmentYouth development programmes work with groups of teenagers and aim to promote theirpersonal development, self-esteem, positive aspirations and good relationships with adults inorder to reduce potentially harmful behaviours, such as drug use (Quinn, 1999). As well asenhancing young people’s interests, skills and abilities, youth projects also have the potentialto divert young people away from drug use through engaging them in more positive sourcesof recreation, and youth workers can provide credible health messages and signpost healthservices. There has been considerable interest from policymakers in youth developmentinterventions as an alternative means of reducing young people’s drug use. For example, inthe United Kingdom youth work programmes targeted at socially disadvantaged and‘excluded’ young people and other ‘at-risk’ groups have been supported by the Government,including new community-based youth development projects such as the Positive Futuresinitiative and the Young People’s Development Programme (Department for Education andSkills, 2005).Evaluations of youth development interventions targeted at vulnerable young people haveshown mixed results: although some studies report that youth development interventions havehad positive effects (Philliber et al., 2001; Michelsen et al., 2002), others suggest theseinterventions may be ineffective (Grossman and Sipe, 1992) or even harmful (Palinkas et al.,1996; Cho et al., 2005; Wiggins et al., 2009). It appears that involvement in such programmesmay result in an increase in drug use where: young people are stigmatised (or ‘labelled’) viatargeting, which further reduces their self-esteem and aspirations; and/or harmful socialnetwork effects arise through aggregating ‘high risk’ young people together, thus introducingyoung people to new drug-using peers (Bonell and Fletcher, 2008). For example, in a studyexamining an intervention for high-risk high school students (Cho et al., 2005), greaterexposure to the programme predicted greater ‘high-risk peer bonding’ and more negativeoutcomes, including higher prevalence of cannabis and alcohol use (Sanchez et al., 2007).Youth development approaches are therefore likely to be most appropriate and effective wherethey are delivered in universal settings to avoid the harmful ‘labelling’ and social networkeffects associated with targeting ‘high risk’ youth. In the United States, after-school andcommunity-based youth development programmes promoting civic engagement and learningthrough the principle of ‘serve and learn’ — which involves voluntary service, reflection on thisvoluntary service though discussion groups, social development classes and learning support— have been found to be effective in reducing a wide range of risky behaviours includinginvolvement with drugs and teenage pregnancy (Michelsen et al., 2002; Harden et al., 2009).Where youth workers aim to target ‘high risk’ groups of young people, ‘detached’, street-basedservices may be more appropriate in order to avoid the potentially harmful social networkeffects associated with aggregating these young people together in youth centres, although this366
Chapter 13: Young people, recreational drug use and harm reduction
needs further evaluation (Fletcher and Bonell, 2008). Examples of street-based youth projectsinclude the Conversas de Rua programme in Lisbon (http://www.conversasderua.org/) and the‘Off the Streets’ community youth initiative in Derry, Northern Ireland.Settings-based approachesSettings-based approaches to health promotion have their roots in the World HealthOrganization’s (WHO) Health for All initiative and the Ottawa Charter for Health Promotion(WHO, 1986). The Ottawa Charter argued that health is influenced by where people ‘learn,work, play and love’, integrated new thinking about health promotion, and heralded the startof this new approach (Young, 2005). Key principles regarded as necessary to achieve thestatus of a ‘health promoting setting’ are the creation of a healthy environment and theintegration of health promotion into the routine activities of the setting (Baric, 1993). Since thelate 1980s, health promotion interventions have been widely established, which makechanges to recreational ‘settings’, such as nightclubs, or institutional ‘settings’, such as schools,to address the social and environmental determinants of harmful drug use.Interventions in recreational settingsStudies of young people in Europe who attend dance music events consistently report muchhigher prevalence of drug use than found in surveys of the general population (EMCDDA,2006a). A ‘Hegemonic Recreational Nightlife Model’ has been used to understand howrecreational drug use and the settings where this takes place now govern many young people’sweekend entertainment and social networks, and can give ‘meaning’ to their lives throughintensive participation (Calafat et al., 2003). The recreation industry thus not only suppliesservices but also contributes to defining entertainment and creating the conditions in whichrecreational drug use takes place. In turn, there is a wide range of risk behaviours associatedwith recreational drug use in this context (e.g. violence, sexual risk, traffic risk), and these havebeen found to be influenced by factors such as a ‘permissive atmosphere’ (Homel and Clark,1994; Graham et al., 2006), overcrowding (Macintyre and Homel, 1997), overt sexual activity(Homel et al., 2004; Graham et al., 2006) and transport habits (Calafat et al., 2009).A wide range of interventions now aim to change the physical context and/or the social andcultural norms of recreational settings to address the conditions and influences associatedwith the most ‘habitual’ contexts for young people’s recreational drug use, such as nightlifesettings and music festivals, and the potential harms arising from use in such contexts. Forexample, several organisations in Europe have launched safer nightlife guidelines. ‘Saferdancing’ guidelines, developed in the United Kingdom, have now become an important toolin this field. Other examples are the Safe Nightlife initiative in Holstebro, Denmark, and theLondon Drug Policy Forum’s ‘Dance Till Dawn Safely’ initiative.Safe-clubbing guidelines aim to reduce opportunities for drug-related problems to occur inthese settings and include promoting the accessibility of free water, the immediate availabilityof first aid and outreach prevention work with young clubbers. Reports on the availability ofsuch measures, in nightclubs with sufficiently large target populations for the intervention to367
Harm reduction: evidence, impacts and challenges
be implemented, were collated by the EMCDDA in 2008 (EMCDDA, 2009). These reportshighlighted the limited availability of simple measures to prevent or reduce health risks anddrug use in European nightlife settings. For example, it was found that outreach preventionwork was provided in the majority of dance clubs in only two out of 20 European countries(Slovenia and Lithuania), while free water was still not routinely available in nine of the 20countries. Furthermore, while 12 countries now report having developed guidelines fornightlife venues, only the Netherlands, Slovenia, Sweden and the United Kingdom report thatthey are monitored and implemented.The most widely implemented intervention in recreational settings is the responsible beverageservice (RBS) guidelines to support staff and managers in harm reduction strategies. A recentsystematic review, however, concluded that there is no reliable evidence that these interventionsare effective in preventing injuries or other harms (Ker and Chinnock, 2008; see also Herring etal., 2010). Community-based approaches to responsible service may produce the largest andmost significant effects. For example, Stockholm Prevents Alcohol and Drug Problems (STAD) isa community-based prevention programme that started in 1996 in Stockholm to promotecommunity mobilisation, the training of bar staff in RBS and stricter enforcement of existingalcohol licensing and drug laws: an evaluation found a decrease in alcohol-related problems,increased refusal to serve minors and a 29 % reduction in assaults (Wallin and Andréasson,2005). However, large-scale community-based interventions are likely to be expensive andneed political commitment. Other factors may also limit compliance to responsible service, suchas low pay, high staff turnover and a stressful working environment, and the efficacy of suchinterventions is therefore likely be greater when enforced as a statutory intervention (Ker andChinnok, 2008; Wallin and Andréasson, 2005).Promising interventions that need further evaluation are glassware bans in recreationalsettings (Forsyth, 2008) and the creation of collaborating guidelines between licensedpremises and accident and emergency services (Wood et al., 2008). Some nightclubs inEurope have now incorporated a first aid service inside the premises, but we are not awareof any evaluations of their effectiveness. Further research and effective collaboration betweenhealth promoters, nightlife settings and the alcohol industry are likely to be crucial inreducing the harms associated with young people’s recreational drug use. However, buildingrelationships across these sectors is not straightforward. ‘Codes of practice’ with the potentialof enforcement may be the most appropriate means to facilitate engagement across thesectors (Graham, 2000). At present, there seems to be a reluctance to enforce greateraccountability through law enforcement. The Tackling Alcohol Related Street Crime (TASC)intervention in Cardiff provides an example of a broad and multifaceted interventionimplemented largely by the police that produced reductions in violence at the relevantpremises, although further research is needed to examine the feasibility of introducing police-led approaches in nightlife settings more generally (Maguire et al., 2003).Finally, on-site pill testing in recreational settings has been a controversial issue for severalyears and appears to be steadily less common in Europe. The main arguments against pilltesting are the limited capacity of on-site tests to accurately detect harmful substances andthat, by permitting on-site pill testing, contradictory messages are being sent out about therisks related to both use and possession of controlled substances (EMCDDA, 2006b).368
Chapter 13: Young people, recreational drug use and harm reduction
Whole-school interventionsFollowing the emergence of ‘settings-based approaches’ to health promotion, traditionalclassroom-based drugs education programmes have gradually been accompanied byadditional strategies in schools that address more ‘upstream’ environmental, social andcultural determinants of young people’s drug use, such as student disengagement andtruancy. The origin of this new ‘settings’ approach to health promotion in schools is attributedto a WHO conference in 1989 which led to the publication ofThe Healthy School(Youngand Williams, 1989). Following this report, ‘whole-school’ approaches have receivedcontinued support from international networks, such as the WHO, the European Network ofHealth Promoting Schools (ENHPS) and the International School Health Network (ISHN)(WHO, 1998; McCall et al., 2005).Using cross-sectional survey data from 10 European countries, Canada and Australia,Nutbeam and colleagues (1993) found a consistent relationship between ‘alienation’ atsecondary school and ‘abusive behaviours’, such as smoking, drinking and drug use, andwarned that ‘schools can damage your health’. Further analysis of this data suggested thatstudents’ perceptions of being treated fairly, school safety and teacher support were relatedto substance use (Samdal et al., 1998). Three recent systematic reviews of experimentalstudies of ‘whole-school health promotion interventions’, which make changes to schools’physical environment, governance and management, policies, and/or educational andpastoral practices, have found that these approaches appear to be ‘promising’ for reducinga wide range of ‘risky’ health behaviours among young people (Lister-Sharpe et al., 1999;Mukoma and Flisher, 2004; Fletcher et al., 2008). The review by Fletcher and colleaguesfound that changes to the school social environment that increase student participation,improve teacher–student relationships, promote a positive school ethos and reducedisengagement are associated with reduced drug use. The Gatehouse Project in Australia isone of the best-known examples (http://www.rch.org.au/gatehouseproject/).Although various pathways may plausibly underlie school effects on drug use and drug-related harms, three potential pathways via which school effects on drug use may occur havebeen identified: peer-group sorting and drug use as a source of identity and bonding amongstudents who are disconnected from the main institutional markers of status; students’ desireto ‘fit in’ at schools perceived to be unsafe, and drug use facilitating this; and/or drug use asa strategy to manage anxieties about schoolwork and escape unhappiness at schools lackingeffective social support systems (Fletcher et al., 2009b). This evidence further supports ‘whole-school’ interventions to reduce drug use through: recognising students’ varied achievementsand promoting a sense of belonging; reducing bullying and aggression; and providingadditional social support for students.
DiscussionThere is considerable data on the prevalence of recreational drug use among young peoplein European countries, and the related adverse health and other harms. However, much ofthis evidence regarding overall prevalence of young people’s drug use is gained through369
Harm reduction: evidence, impacts and challenges
school-based surveys and we cannot assume that patterns of drug use among young peoplewho have low school attendance and young people who have been excluded from schoolwill therefore be accurately captured in these surveys; there are also practical problems withcollecting reliable self-report data about students’ use of drugs in school-based surveys(McCambridge and Strang, 2006). Street-based surveys of young people, such as theVancouver Youth Drug Reporting System (VCH, 2007), could therefore complement existingmonitoring systems in Europe. Nonetheless, current European surveys that monitorprevalence and trends are well established and allow cross-national comparisons to be maderegarding young people’s drug use.In response to public and political concerns about the harmful consequences of young people’sdrug use, a wide range of interventions have been implemented throughout Europe andelsewhere. There is no ‘magic bullet’, and harm reduction strategies in this context will need toencompass both universal and targeted strategies that seek to prevent or delay drug use,reduce the frequency of drug use during adolescence, and make changes to risk environments.Mass media campaigns may be politically important but appear to be largely ineffective (andoccasionally counter-productive). If they are to continue to play a role in informing youngpeople about the risks associated with recreational drug use, health promoters should designmass media campaigns in conjunction with young people and — although it is difficult toattribute changes in behaviour to mass media interventions — these campaigns should besubjected to pilot trials prior to ‘roll-out’. Future mass media campaigns should also pay closeattention to providing easy access to information via the Internet and telephone advice lines.Based on the current evidence, school-based programmes show greater promise forpreventing young people initiating drug use at a young age than mass media interventions.Comprehensive social influence models and peer-led programmes based on the ‘diffusion ofinnovations’ approach are the most promising approaches for drugs education andprevention in schools, and thus should be piloted and evaluated more widely in Europe.Interventions that promote a positive school ethos and reduce student disaffection andtruancy are likely to be an effective complement to these drugs education and preventioninterventions in schools. These school-level ‘settings’ interventions focusing on the more‘upstream’ determinants of risk should also now be piloted and evaluated in Europe toexamine their potential for harm reduction.Motivational interviewing shows considerable promise in a wide range of settings, includingamong those young people with the heaviest patterns of drug use. However, motivationalinterviewing is resource-intensive and where there is insufficient investment this will impact onits potential for harm reduction. New training programmes in motivational interviewingshould therefore be considered a priority in European countries, initially to build capacity forgreater intervention in recreational contexts and among professionals working with high-riskyoung people.Youth development approaches appear to be most appropriate and effective in addition to,rather than as an alternative to, school, such as after-school and school-holiday programmespromoting self-esteem, positive aspirations, supportive relationships and learning through theprinciple of ‘serve and learn’, which is based on volunteering in the local community. In370
Chapter 13: Young people, recreational drug use and harm reduction
addition, because of its focus on working with existing peer groups (and thus its ability to avoidthe potentially harmful effects associated with centre-based youth projects), as well as itsgreater reach and flexibility, detached, street-based youth work may be the most appropriateand effective approach for targeting those young people deemed at ‘high risk’ of harm. Theseapproaches should be the subject of further evaluation in Europe with high-risk groups.Perhaps of greatest concern at present is the lack of agreement and guidance about what todo in recreational settings in Europe to reduce drug-related harm. There are few statutorypolicies governing the most ‘habitual’ contexts for young people’s recreational drug use, suchas nightlife settings and music festivals, or rigorous evaluations of interventions in suchsettings in Europe. Guidelines promoting the accessibility of free water, immediate availabilityof first aid and outreach services have been implemented with promising effects in some (butby no means all) European countries. These should be enforced through changing them intolaws where possible and be accompanied by additional efforts to encourage responsiblealcohol service and reduce other risky behaviours.
ReferencesBall, A. (2007), ‘HIV, injecting drug use and harm reduction: a public health response’,Addiction102, pp. 684–90.Baric, L. (1993), ‘The settings approach: implications for policy and strategy’,Journal of the Institute of HealthEducation31, pp. 17–24.Beautrais, A. L., Joyce, P. R. and Mulder, R. T. (1999), ‘Cannabis abuse and serious suicide attempts’,Addiction,94, pp. 1155–64.Bonell, C. and Fletcher, A. (2008), ‘Addressing the wider determinants of problematic drug use: advantages ofwhole-population over targeted interventions’,International Journal of Drug Policy19, pp. 267–9.Boreham, R., Fuller, E., Hills, A. and Pudney, S. (2006),The arrestee survey annual report: Oct. 2003–Sept. 2004,England and Wales,Home Office, London.Cahill, H. W. (2007), ‘Challenges in adopting evidence-based school drug education programmes’,Drug andAlcohol Review26, pp. 673–9.Calafat, A., Fernandez, C., Juan, M., et al. (2003),Enjoying nightlife in Europe: the role of moderation,Irefrea,Palma de Mallorca.Calafat, A., Blay, N., Juan, M., et al. (2009), ‘Traffic risk behaviors at nightlife: drinking, taking drugs, driving,and use of public transport by young people’,Traffic Injury Prevention10, pp. 162–9.Campbell, R., Starkey, F., Holliday, J., et al. (2008), ‘An informal school-based peer-led intervention for smokingprevention in adolescence (ASSIST): a cluster randomised trial’,Lancet371, pp. 1595–602.Charlton, J., Kelly, S. and Dunnell, K. (1993), ‘Suicide deaths in England and Wales: trends in factors associatedwith suicide deaths’,Population Trends7, pp. 34–42.Cho, H., Hallfors, D. D. and Sanchez, V. (2005), ‘Evaluation of a high school peer group intervention for at-riskyouth’,Journal of Abnormal Child Psychology33, pp. 363–74.Department for Education and Skills (2005),Every child matters: change for children, young people and drugs,HerMajesty’s Stationery Office, London.
371
Harm reduction: evidence, impacts and challenges
Derzon, J. H. and Lipsey, M. W. (2002), ‘A meta-analysis of the effectiveness of mass-communication for changingsubstance-use knowledge, attitudes and behaviour’, in Crano, W. D. and Burgoon, M. (eds),Mass media and drugprevention: classic and contemporary theories and research,Lawrence Erlbaum Associates, Matwah.Emmett, D. and Nice, G. (2006),Understanding street drugs,Jessica Kingsley Publishers, London.EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2002),Recreational drug use: a key EUchallenge,Drugs in focus, European Monitoring Centre for Drugs and Drug Addiction, Lisbon.EMCDDA (2006a),Annual report 2006: the state of the drugs problem in Europe,European Monitoring Centre forDrugs and Drug Addiction, Lisbon.EMCDDA (2006b),Developments in drug use within recreational settings,European Monitoring Centre for Drugsand Drug Addiction, Lisbon.EMCDDA (2007),Cocaine and crack cocaine: a growing public health issue,European Monitoring Centre forDrugs and Drug Addiction, Lisbon.EMCDDA (2009),Annual report 2009: the state of the drugs problem in Europe,European Monitoring Centre forDrugs and Drug Addiction, Lisbon.Evans-Whipp, T., Beyers, J. M., Lloyd, S., et al. (2004), ‘A review of school drug polices and their impact onyouth substance use’,Health Promotion International19, pp. 227–34.Faggiano, F. and Vigna-Taglianti, F. D. (2008), ‘Drugs, illicit — primary prevention strategies’,InternationalEncyclopaedia of Public Health 2,pp. 249–65.Faggiano, F., Vigna-Taglianti, F. D., Versino, E., et al. (2005), ‘School-based prevention for illegal drugs use’,Cochrane Database of Systematic Reviews2, Art. No. CD003020.Faggiano, F., Galanti, M. R., Bohrn, K., et al. (2008), ‘The effectiveness of a school-based substance abuseprevention program: EU–Dap cluster randomised controlled trial’,Preventive Medicine47, pp. 537–43.Ferguson, D. M., Boden, J. M. and Horwood, L. J. (2006), ‘Cannabis use and other illicit drug use: testing thecannabis gateway hypothesis’,Addiction101, pp. 556–69.Flay, B. R., DiTecco, D. and Schlegel, R. P. (1980), ‘Mass media in health promotion: an analysis extendedinformation-processing model’,Health Education and Behavior7, pp. 127–47.Fletcher, A. and Bonell, C. (2008), ‘Detaching youth work to reduce drug and alcohol-related harm’,Public PolicyResearch15, pp. 217–23.Fletcher, A., Bonell, C. and Hargreaves, J. (2008), ‘School effects on young people’s drug use: a systematicreview of intervention and observational studies’,Journal of Adolescent Health42, pp. 209–20.Fletcher, A., Bonell, C., Sorhaindo, A. and Rhodes, T. (2009a), ‘Cannabis use and “safe” identities in an inner-city school risk environment’,International Journal of Drug Policy20, pp. 244–50.Fletcher, A., Bonell, C., Sorhaindo, A. and Strange, V. (2009b), ‘How might schools influence young people’s druguse? Development of theory from qualitative case-study research’,Journal of Adolescent Health45, pp. 126–32.Forsyth, A. J. M. (2008), ‘Banning glassware from nightclubs in Glasgow (Scotland): observed impacts,compliance and patrons views’,Alcohol and Alcoholism43, pp. 111–17.Foxcroft, D. R., Ireland, D., Lowe, G. and Breen, R. (2002), ‘Primary prevention for alcohol misuse in youngpeople’,Cochrane Database of Systematic Reviews3, Art. No. CD003024.
372
Chapter 13: Young people, recreational drug use and harm reduction
Graham, K. (2000), ‘Preventive interventions for on-premise drinking: a promising but under researched area ofprevention’,Contemporary Drug Problems27, pp. 593–668.Graham, K., Bernards, S., Osgood, D. W. and Wells, S. (2006), ‘Bad nights or bad bars? Multi-level analysis ofenvironmental predictors of aggression in late-night large-capacity bars and clubs’,Addiction101, pp. 1569–80.Gray, E., McCambridge, J. and Strang, J. (2005), ‘The effectiveness of motivational interviewing delivered byyouth workers in reducing drinking, cigarette and cannabis smoking among young people: quasi-experimentalpilot study’,Alcohol and Alcoholism40, pp. 535–9.Grenard, J. L., Ames, S. L., Pentz, M. A. and Sussman, S. (2006), ‘Motivational interviewing with adolescents andyoung adults for drug-related problems’,International Journal of Adolescent Medicine and Health18, pp. 53–67.Grossman, J. B. and Sipe, C. L. (1992),Report on the long-term impacts (STEP program),Public/Private Ventures,Philadelphia.Hall, W. (2006), ‘The mental health risks of adolescent cannabis use’,PLoS Medicine3, p. e39.Hall, W. and Fischer, B. (2010), ‘Harm reduction policies for cannabis’, in European Monitoring Centre for Drugsand Drug Addiction (EMCDDA),Harm reduction: evidence, impacts and challenges,Rhodes, T. and Hedrich, D.(eds), Scientific Monograph Series No. 10, Publications Office of the European Union, Luxembourg.Hall, W. and Solowij, N. (1998), ‘Adverse effects of cannabis’,Lancet352, pp. 1611–16.Harden, A., Brunton, G., Fletcher, A. and Oakley, A. (2009), ‘Teenage pregnancy and social disadvantage:systematic review integrating controlled trials and qualitative studies’,BMJ339, b4254.HDA (Health Development Agency) (2004),The effectiveness of public health campaigns,Health DevelopmentAgency, London.Henderson, S., Holland, J., McGrellis, S., Sharpe, S. and Thompson, R. (2007),Inventing adulthoods: abiographical approach to youth transitions,SAGE, London.Henquet, C., Krabbendam, L., Spauwen, J., et al. (2005), ‘Prospective cohort study of cannabis use,predisposition for psychosis, and psychotic symptoms in young people’,BMJ330, pp. 11–16.Herring, R., Thom, B., Beccaria, F., Kolind, T. and Moskalewicz, J. (2010), ‘Alcohol harm reduction in Europe’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Hibell, B., Anderson, B., Bjarnsson, T., et al. (2004),The ESPAD report 2003: alcohol and other drug use amongstudents in 35 countries,The Swedish Council for Information on Alcohol and Other Drugs, Stockholm.Hibell, B., Guttormsson, U., Ahlström, S., et al. (2009),The 2007 ESPAD report: substance use among students in 35European countries,The Swedish Council for Information on Alcohol and Other Drugs, Stockholm.Hoare, J. and Flatley, J. (2008),Drug misuse declared: findings from the 2007/08 British Crime Survey,HerMajesty’s Stationery Office, London.Home Office (2002),Updated national drugs strategy,Her Majesty’s Stationery Office, London.Home Office, Department of Health, Department for Education and Skills (2006),FRANK review,Her Majesty’sStationery Office, London.Homel, R. and Clark, J. (1994), ‘The prediction and prevention of violence in pubs and clubs’,Crime PreventionStudies3, pp. 1–46.
373
Harm reduction: evidence, impacts and challenges
Homel, R., Carvolth, R., Hauritz, M., McIlwain, G. and Teague, R. (2004), ‘Making licensed venues safer forpatrons: what environmental factors should be the focus of interventions?’,Drug and Alcohol Review23, pp. 19–29.Hornik, R. (2002), ‘Public health communication: making sense of contradictory evidence’, in Hornik, R.,Publichealth communication: evidence for behavior change,Erlbaum, Mahwah.Hornik, R., Jacobsohn, L., Orwin, R., Piesse, A., and Kalton, G. (2008), ‘Effects of the National Youth Anti-DrugMedia Campaign on youths’,American Journal of Public Health98, pp. 2229–36.Independent Advisory Group on Sexual Health and HIV (2007),Sex, drugs, alcohol and young people: a review ofthe impact drugs and alcohol has on the sexual behaviour of young people,Department of Health, London.Jayakody, A., Sinha, S., Curtis, K., et al. (2005),Smoking, drinking, drug use, mental health and sexual behaviourin young people in East London,Department of Health/Teenage Pregnancy Unit, London.Jessor, R., Donovan, J. E. and Costa, F. M. (1991),Beyond adolescence: problem behaviour and young adultdevelopment,Cambridge University Press, Cambridge.Ker, K. and Chinnock, P. (2008), ‘Interventions in the alcohol server setting for preventing injuries’,CochraneDatabase of Systematic Reviews3, Art. No. CD005244.Kimber, J., Palmateer, N., Hutchinson, S., et al. (2010), ‘Harm reduction among injecting drug users: evidence ofeffectiveness’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction:evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10,Publications Office of the European Union, Luxembourg.Lister-Sharp, D., Chapman, S., Stewart-Brown, S. and Sowden, A. (1999), ‘Health promoting schools and healthpromotion in schools: two systematic reviews’,Health Technology Assessment3 (22), pp. 1–207.Lynskey, M. T., Heath, A. C., Bucholz, K. K., et al. (2003), ‘Escalation of drug use in early onset cannabis users vsco-twin controls’,JAMA289, pp. 427–33.McCall, D. S., Rootman, I. and Bayley, D. (2005), ‘International school health network: an informal network foradvocacy and knowledge exchange’,Promotion and Exchange12, pp. 173–7.McCambridge, J. and Strang, J. (2004), ‘The efficacy of single-session motivational interviewing in reducing drugconsumption and perceptions of drug-related risk and harm among young people’,Addiction99, pp. 39–52.McCambridge, J. and Strang, J. (2005), ‘Deterioration over time in effect of motivational interviewing in reducingdrug consumption and related risk among young people’,Addiction100, pp. 470–8.McCambridge, J. and Strang, J. (2006), ‘The reliability of drug use collected in the classroom: what is theproblem, why does it matter and how should it be approached?’,Drug and Alcohol Review25, pp. 413–18.McCambridge, J., Slym, R. L. and Strang, J. (2008), ‘Randomized controlled trial of motivational interviewingcompared with drug information and advice for early information among young cannabis users’,Addiction103,pp. 1819–20.Macintyre, S. and Homel, R. (1997), ‘Danger on the dance floor: a study of interior design, crowding andaggression in nightclubs’, in Homel, R. (ed.)Policing for prevention: reducing crime, public intoxication and injury,Criminal Justice Press, New York.MacLeod, J., Oakes, R., Oppenkowski, T., et al. (2004), ‘How strong is the evidence that illicit drug use by youngpeople is an important cause of psychological or social harm? Methodological and policy implications of asystematic review of longitudinal, general population studies’,Lancet363, pp. 1579–88.
374
Chapter 13: Young people, recreational drug use and harm reduction
Maguire, M., Morgan, R. and Nettleton, H. (2003),Reducing alcohol-related violence and disorder: an evaluationof the ‘TASC’ project,Home Office, London.Martin, G., Copeland, J. and Swift, W. (2005), ‘The adolescent cannabis check-up: feasibility of a briefintervention for cannabis users’,Journal of Substance Abuse Treatment29, pp. 207–13.Melrose, M., Turner, P., Pitts, J. and Barrett, D. (2007),The impact of heavy cannabis use on young people:vulnerability and youth transitions,Joseph Rowntree Foundation, York.Michelsen, E., Zaff, J. F. and Hair, E. C. (2002),A civic engagement program and youth development: a synthesis,Child Trends, Edna McConnell Clark Foundation, New York.Miller, W. R. and Rollnick, S. (2002),Motivational interviewing: preparing people for change,Guildford Press, London.Moore, T. H. M., Zammit, S., Lingford-Hughes, A., et al. (2007), ‘Cannabis use and risk of psychotic or affectivemental health outcomes: a systematic review’,Lancet370, pp. 319–28.Mukoma, W. and Flisher, A. J. (2004), ‘Evaluations of health promoting schools: a review of nine studies’,HealthPromotion International19, pp. 357–68.NatCen and NFER (2007),Smoking, drinking and drug use among young people in England in 2006: headlinefigure,NHS Information Centre, London.Nutbeam, D., Smith, C., Moore, L. and Bauman, A. (1993), ‘Warning! Schools can damage your health: alienationfrom school and its impact on health behaviour’,Journal of Paediatric and Child Health29, pp. S25–S30.Orwin, R., Cadell, D., Chu, A., et al. (2006),Evaluation of the National Youth Anti-Drug Media Campaign,NIDA,Rockville.Palinkas, L. A., Atkins, C. J., Miller, C. and Ferreira, D. (1996), ‘Social skills training for drug prevention in high-risk female adolescents’,Preventive Medicine25, pp. 692–701.Parrott, A. C., Lees, A., Garnham, N. J., Jones, M. and Wesnes, K. (1998), ‘Cognitive performance inrecreational users of MDMA or “ecstasy”: evidence for memory deficits’,Journal of Psychopharmacology12, pp.79–83.Petrie, J., Bunn, F. and Byrne, G. (2007), ‘Parenting programmes for preventing tobacco, alcohol or drugs misusein children <18: a systematic review’,Health Education Research22, pp. 177–91.Philliber, S., Williams, K., Herrling, S. and West, E. (2001), ‘Preventing pregnancy and improving health careaccess among teenagers: an evaluation of the Children’s Aid Society-Carrera Program’,Perspectives on Sexualand Reproductive Health34, pp. 244–51.Phillips, R. and Kinver, A. (2007),Know the score: cocaine wave 4 — 2006/07 post-campaign evaluation,ScottishExecutive Research Group, Edinburgh.Quinn, J. (1999), ‘Where need meets opportunity: youth development programs for early teens’,The Future ofChildren9, pp. 96–116.Randolph, W. and Viswanath, K. (2004), ‘Lessons learned from public health mass media campaigns: marketinghealth in a crowded media world’,Annual Review of Public Health25, pp. 419–37.Reynaud-Maurupt, C., Chaker, S., Claverie, O., et al. (2007),A Pratiques et opinions liées aux usages dessubstances psychoactives dans l’espace festif «musiques électroniques»,TRENDS, Observatoire Fran§ais des Drogueset des Toxicodependences.Ringwalt, C., Vincus, A. A., Hanley, S., et al. (2008), ‘The prevalence of evidence-based drug use preventioncurricula in U.S. middle schools in 2005’,Prevention Science9, pp. 276–87.
375
Harm reduction: evidence, impacts and challenges
Samdal, O., Nutbeam, D., Wold, B. and Kannas, L. (1998), ‘Achieving health and educational goals throughschool: a study of the importance of the school climate and the student’s satisfaction with school’,HealthEducation Research: Theory and Practice13, pp. 383–97.Sánchez, V., Steckler, A., Nitirat, P., et al. (2007), ‘Fidelity of implementation in a treatment effectiveness trial ofReconnecting Youth’,Health Education Research22, pp. 95–107.Schilt, T., Maartje, M., de Win, M. L., et al. (2007), ‘Cognition in novice ecstasy users with minimal exposure toother dugs: a prospective cohort study’,Archives of General Psychiatry64, pp. 728–36.Shildrick, T. (2002), ‘Young people, illicit drug use and the question of normalization’,Journal of Youth Studies5,pp. 35–48.Solowij, N. and Battisti, R. (2008), ‘The chronic effects of cannabis on memory in human: a review’,Current DrugAbuse Reviews1, pp. 81–98.Tait, R. J. and Hulse, G. K. (2003), ‘A systematic review of the effectiveness of brief interventions with substanceusing adolescents by type of drug’,Drug and Alcohol Review22, pp. 337–46.Tevyaw, T. O. and Monti, P. M. (2004), ‘Motivational enhancement and other brief interventions for adolescentsubstance use: foundations, applications and evaluations’,Addiction99, pp. 63–75.Thomas, J., Kavanagh, J., Tucker, H., et al. (2007),Accidental injury, risk-taking behaviour and the socialcircumstances in which young people (aged 12–24) live: a systematic review,EPPI-Centre, London.Thomas, R. E. and Perera, R. (2006), ‘School-based programmes for preventing smoking’,Cochrane Database ofSystematic Reviews3, Art. No. CD001293.Van Der Kreeft, P., Wiborg, G., Galanti, M. R., et al. (2009), ‘“Unplugged”: a new European school programmeagainst substance abuse’,Drugs: education, prevention and policy16, pp. 167–81.VCH (Vancouver Coastal Health) (2007),2006 Vancouver youth drug reporting system: first results,VancouverCoastal Health Authority, Vancouver.Wallin, E. and Andréasson, S. (2005), ‘Effects of a community action program on problems related to alcoholconsumption at licensed premises’, in Stockwell, T., Gruenewald, P. J., Toumbourou, J. W. and Loxley, W. (eds)Preventing harmful substance use: the evidence base for policy and practice,John Wiley, West Sussex.Wiggins, M., Bonell, C., Sawtell, M., et al. (2009), ‘Health outcomes of a youth-development programme inEngland: prospective matched comparison study’,British Medical Journal339, pp. 2534–43.Wood, D. W., Greene, S. L., Alldus, G., et al. (2008), ‘Improvement in the pre-hospital care of recreational drugusers through the development of club specific ambulance referral guidelines’,Substance Abuse Treatment,Prevention and Policy3, p. 14.WHO (World Health Organization) (1986),The Ottawa Charter for Health Promotion,World Health Organization,Copenhagen.WHO (1998),HEALTH21: an introduction to the Health For All policy framework for the WHO European Region(European Health for All Series No. 5), World Health Organization, Copenhagen.Yamaguchi, K. and Kandel, D. B. (1984), ‘Patterns of drug use from adolescence to young adulthood: predictorsof progression’,American Journal of Public Health74, pp. 673–81.Young, I. (2005), ‘Health promotion in schools: a historical perspective’,Promotion and Education12, pp. 112–17.Young, I. and Williams, T. (1989),The healthy school,Scottish Health Education Group, Edinburgh.
376
Chapter 14Criminal justice approaches to harm reduction in EuropeAlex Stevens, Heino Stöver and Cinzia Brentari
AbstractThis chapter reviews the spread of harm reduction services in European criminal justicesystems, and their evaluation. It begins with a discussion of the tensions and contradictionsinherent in providing harm reduction services (which may accept continued drug use) incriminal justice settings (that do not). It then draws on research carried out for theConnections project, for its predecessor the European Network on Drug and InfectionsPrevention in Prisons and on the information gathered by the European Monitoring Centrefor Drugs and Drug Addiction. It examines services such as needle and syringe exchange,opiate substitution and distribution of condoms and disinfectants in prisons. It alsoexamines harm reduction services that have been developed in the context of policecustody, and in the attempt to provide through-care and aftercare to drug users who passthrough the criminal justice system. The chapter concludes that the tensions between harmreduction and criminal justice aims can be overcome in providing effective services toreduce drug-related harms.Keywords:criminal justice systems, harm reduction, prison, decriminalisation, syringeexchange, opioid substitution treatment, arrest-referral.
IntroductionHarm reduction is often seen as conflicting with the use of law enforcement to reduce druguse, but there are ways in which policies and practice can develop in order to reduce harmsrelated to drugs within the criminal justice system. The principle of harm reduction may alsobe applied to law enforcement itself. Drug prohibition can inadvertently increase theharmfulness of drug use as it means that users rely on illicit forms of supply and consumedrugs of unknown purity and quality in a risky manner. It also creates artificially high prices,which stimulate acquisitive crime and facilitate corruption and violence. Given that drugmarkets cannot be eliminated, but may operate in ways that are more or less sociallyharmful, the key questions for law enforcement become: what sort of markets do we leastdislike and how can we adjust the control mix so as to push markets in the least harmfuldirection? In this chapter, we leave aside more detailed discussion of the wider impact of drug law enforcement or criminalisation on societal levels of drug-related harm. We focusinstead on the provision of services that aim to reduce harms done to drug users within thecriminal justice system.Many of the people who are caught up in the criminal justice system are highly exposed todrug-related harms (EMCDDA, 2009a; Singleton et al., 1997; Stöver, 2001; Rotily et al.,379
Harm reduction: evidence, impacts and challenges
2001; Møller et al., 2007; Stöver et al., 2008a; Dolan et al., 2007). These people do not losetheir right to adequate and effective healthcare when they enter the criminal justice system(Carter and Hall, 2010). The ideal criminal justice system would therefore protect their healthby offering the full range of healthcare approaches. Some European systems have beenmoving closer, in various ways, to achieving this, and we describe some of thesedevelopments in this chapter. We will examine how measures such as opioid substitutiontreatment (OST), needle and syringe exchange, and the provision of disinfectants andcondoms have worked in prison contexts. We will look at issues of through-care andaftercare and we will explore how processes that follow arrest can divert drug users intotreatment. Before looking at specific harm reduction measures we provide a short discussionof the inherent tensions between controlling drugs through the criminal law and efforts toreduce harms to drug users.
Tensions between law enforcement and harm reductionThere are at least two contradictions that hinder the effort to reduce harm through thecriminal justice system. The first is the fact that criminal justice systems themselves produceharms. Of course, the criminal justice system also produces benefits to the extent that itprotects people from crime and insecurity. But arrests, fines, community penalties,imprisonment and parole all infringe on individual freedoms and pleasures. The special painsof imprisonment have been a particular focus of criminological research (Sykes 1958;Mathiesen, 2006). The idea that these pains are justified by the need to reduce crime ischallenged by the lack of evidence for the effectiveness of imprisonment, the most painfulform of criminal justice intervention currently used in Europe (Tonry, 2004; Gendreau et al.,1999). It is well known, for example, that there is little relationship between imprisonment andcrime rates (Kovandzic and Vieraitis, 2006; Reiner, 2000). Countries do not use prison as adirect, rational measure to reduce crime. Rather, they choose — through a complex processof ideological, moral, political and juridical negotiation — the level of pain that they arewilling to inflict on their citizens (Christie 1982). If we choose the level of harm that we inflict,we can also choose to reduce it.The second contradiction in pursuing harm reduction in the criminal justice system is thatbetween the pursuit of abstinence and the acknowledgement of continuing drug use.Countries are obliged, through the UN drug conventions, to prohibit and to penalise thepossession of certain substances. The criminal justice system is the process that puts theseobligations into practice. It is very difficult for the same system to acknowledge that thepeople under its control continue to defy the law. Until the mid-1990s, for example, itwas common for prison governors to deny that drug use was going on within their walls(Duke, 2003). More recently, it has been suggested by Phillip Bean (2008) that treatmentagencies working with the criminal justice system should expect to subordinate their aimsto those of the criminal justice agencies. Harm reduction approaches have traditionallybeen developed to meet the needs of people who continue to use illicit drugs, andtherefore do not fit with the prescription that people under penal control should abstain.Some parts of the criminal justice system and some countries appear to negotiate thisconflict more easily than others. This may be due to the different perceptions of the ideal380
Chapter 14: Criminal justice approaches to harm reduction in Europe
goal of abstinence. Within the prison system, for example, abstinence has a relativelyhigh value, because it fits with the prison’s goal of incapacitating the prisoner fromcommitting further crimes (e.g. drug purchase and possession). Probation services, with agreater focus on rehabilitation and relatively less control of the person’s behaviour, seemto have less emphasis on absolute abstention, at least in Europe. In the United States,drug use while on probation often leads to imprisonment. It is more often tolerated inEuropean probation systems, as long as no other offences are committed (Stevens,forthcoming).So how do we deal with these contradictions? First, it seems axiomatic that the best way to reduce the amount of drug-related harm that occurs inside the criminal justice system is toreduce the number of drug users who enter it. Drug users cannot cause harm (or beharmed) in criminal justice settings if they are not actually in these settings. The number ofdrug users in criminal justice settings can be reduced through decriminalisation of drugs,which means that no drug users enter the criminal justice system for possession offences(though decriminalisation of drugs would not necessarily reduce the number of drug userswho enter the system for other offences, which could be reduced by developing diversionor alternative sanctions) (Stevens, forthcoming). Different European countries have triedvarious forms of decriminalisation. They include the Netherlands’ expedient non-prosecution of cannabis supply at the retail level, as well as the non-criminal offences ofpersonal drug use in the Czech Republic, Estonia, Italy, Spain and suspension ofprosecution of personal use offences in Germany and Austria.The most comprehensive process of decriminalisation so far has occurred in Portugal.From July 2001 people who are found by the Portuguese police to be in possession offewer than ten days’ personal supply of any drug have not been arrested, though thedrug is still confiscated. They have instead been referred to regional drug dissuasioncommittees, which have the option of imposing warnings, fines, administrative sanctions(such as taking away driving or firearms licences), or — in the case of dependent users— referring them to treatment. Since decriminalisation, and the simultaneous expansionof prevention, treatment and harm reduction services, there have been dramaticreductions in drug-related deaths and HIV. Rates of drug use seem to have fallen amongchildren, but risen slightly in adults, in line with pan-European trends. The respectiveroles of decriminalisation and the simultaneous expansion of drug treatment in producingthese changes can be debated (IDT, 2007; IDT, 2005; Hughes and Stevens, 2007;Greenwald, 2009). But Figure 14.1 shows clearly that decriminalisation reduced the useof imprisonment for drug offences and led to an overall reduction in the prisonpopulation (IDT, 2006, Table 62). This reduction has also been accompanied bysubstantial reductions in the number of people using drugs and living with HIV withinPortuguese prisons (Torres et al., 2009).The second contradiction is just a more extreme form of the long-standing argument thatharm reduction conflicts with the goal — still subscribed to by all UN members (ECOSOC,2009) — of eliminating illicit drug use. Over time, there has been a gradual acceptancethat harm reduction measures do not prevent people from achieving abstinence, butrather protect the health of people who will continue to use drugs, whether or not they381
Harm reduction: evidence, impacts and challenges
have the means to protect their health. This acceptance has been supported by decadesof evaluative research on harm reduction measures outside the criminal justice system,including opiate substitution treatment (using methadone, buprenorphine or heroin itself)and needle and syringe exchange programmes (Hunt, 2003; Ritter and Cameron, 2005;Tilson et al., 2007; Kimber et al., 2010). As evidence develops on the use of suchmeasures within the criminal justice system, we could expect that resistance to harmreduction within the criminal justice system will also subside. But we should not be toooptimistic. The negotiations at the high level segment of the Commission on NarcoticDrugs in Vienna in March 2009 showed that resistance to harm reduction remains strong,even outside the criminal justice system. A glimmer of hope from that meeting can beperceived, if we look hard enough, in the commitment to provide treatment and ‘relatedsupport services ... on a non-discriminatory basis, including in detention facilities’(ECOSOC, 2009).Figure 14.1:Number of prisoners under sentence for drug and other offences in Portugal,1997–200512 000Non-drug offences10 0008 0006 0004 0002 0000Drug offences
1997
1998
1999
2000
2001
2002
2003
2004
2005
Source:Hughes and Stevens, 2007.
Harm reduction in the criminal justice systemOur exploration of existing harm reduction services in criminal justice systems starts in theplace where drug-related harms of the criminal justice system are most acute: prisons.In a report on the implementation of the European Council Recommendation (of 18 June2003 (1)) on the prevention and reduction of health-related harm associated with drug(1) http://europa.eu.int/eur-lex/pri/en/oj/dat/2003/l_165/l_16520030703en00310033.pdf
382
Chapter 14: Criminal justice approaches to harm reduction in Europe
dependence (2) it was stated that a policy to provide drug users in prisons with servicesthat are similar to those available to drug users outside prisons exists in 20 EU MemberStates and was about to be introduced in four countries (van der Gouwe et al., 2006).However, recent European monitoring data show that that the implementation of harmreduction programmes is quite heterogeneous in European prisons (EMCDDA, 2009a).Availability and accessibility of many key harm reduction measures in prisons lag farbehind the availability and accessibility of these interventions in the community outsideprisons (EMCDDA, 2009b).Illustrating this gap most vividly is the provision — or lack thereof — of needle and syringeprogrammes (NSP), currently only implemented in five EU countries (EMCDDA, 2009c). Theavailability of opioid substitution treatment (OST) in prisons is low compared to the level ofOST provision in the community in most European countries (EMCDDA, 2009d; see Figure14.2). These findings support an earlier statement from the European Commission that:Harm reduction interventions in prisons within the European Union are still not in accordance withthe principle of equivalence adopted by UN General Assembly, UNAIDS/WHO and UNODC,which calls for equivalence between health services and care (including harm reduction) insideprison and those available to society outside prison. Therefore, it is important for the countries toadapt prison-based harm reduction activities to meet the needs of drug users and staff in prisonsand improve access to services.(European Commission, 2007, conclusion 5).
These findings also echo a 2008 WHO Regional Office for Europe report that monitoredState progress in achieving Dublin Declaration goals. The Dublin Declaration commits thesignatory States to take 33 specific actions — and in some cases meet specific targets — toaddress the HIV prevention, care, treatment and support situation across the region. Thereport found that, of the 53 signatory countries, condoms were available in prisons in only18, syringe exchange programmes available in six and substitution treatment available in 17(Matic et al., 2008). A more recent review (in 2009) by the International Harm ReductionAssociation (IHRA) found the situation has only marginally improved, with nine countries (outof 46) in Europe and Central Asia having syringe exchange in prisons and 28 substitutiontreatment (Cook, 2009; see also Cook et al., 2010).Calls for an urgent and comprehensive response to addressing health risks within prisonsettings, including harm reduction measures (WHO Regional Office for Europe, 2005) arenot new, and have been highlighted in international reports and policy documents spanningtwo decades (Parliamentary Assembly of the Council of Europe, 1988; UNODC et al., 2006;WHO, 1993; Matic et al., 2008). However, despite existing recommendations, guidelines andcommitments made by governments and many others (Lines, 2008), only very few countrieswithin the European region have come close to achieving the goals set out (Cook, 2009).There are four key harm reduction tools for the prison setting. We describe each of these,including an example of best practice, below.(2) http://ec.europa.eu/health/ph_determinants/life_style/drug/drug_rec_en.htm
383
Harm reduction: evidence, impacts and challenges
Figure 14.2:Provision of substitution/maintenance treatment (OST) in the community and availabilityof OST programmes in the prison system in 2007 in the EU (expert rating)BE, DK,PT, MT,LU, SI,HR
FullOST provision in the community
FR, UK
IT, NL
Extensive
BG, CY
CZ, DE
IE
ES, AT
Limited
EE, GR, LT,RO, SK
HU,FI, PL
NO
Rare
LV
Not available
TR
Not available
Rare
Limited
Extensive
Full
OST availability in the prison systemNotes:This figure is available at: http://www.emcdda.europa.eu/stats09/hsrfig2.Comments:Data were not available for Sweden.Rating scales:Prison: expert rating of the availability of OST programmes in prisons in the country (and does not reflect level ofOST provision in prison): • ull: substitution/maintenance treatment exists in nearly all prisons.F • xtensive: exists in a majority of prisons but not in nearly all of them.E • imited: exists in more than a few prisons but not in a majority of them.L • are: exists in just a few prisons.RCommunity: expert rating of the level of provision of OST in the community, in relation to the needs of target groupproblem opioid users: • ull: nearly all problem opioid users (POUs) in need would obtain OST.F • xtensive: a majority but not nearly all POUs in need would obtain OST.E • imited: more than a few but not a majority of POUs in need would obtain OST.L • are: just a few POUs in need would obtain OST.RSources:EMCDDA, 2009d. Structured questionnaire on ‘treatment programmes’ (SQ27/P1), submitted by NFPs in 2008.Data for Malta is from DG Health and Consumer Protection, ‘Final report on prevention, treatment, and harm reductionservices in prison, on reintegration services on release from prison and methods to monitor/analyse drug use amongprisoners’, SANCO/2006/C4/02.
Needle and syringe exchange programmes in prisonsA position paper of the United Nations system identifies NSP as one component of ‘acomprehensive package for HIV prevention among drug abusers’ (Commission on NarcoticDrugs, 2002). In prisons, NSPs have been operating successfully for more than 15 years. Ameta-analysis (based on 11 evaluations of the implementation of prison-based NSPs)revealed that none of the fears often associated with planned NSPs occurred in any project:syringe distribution was followed neither by an increase in drug intake nor in administration384
Chapter 14: Criminal justice approaches to harm reduction in Europe
by injection. Syringes were not misused as weapons against staff or other prisoners, anddisposal of used syringes was uncomplicated. Sharing of syringes among drug usersdisappeared almost completely or was apparent in very few cases. These studiesdemonstrate both the feasibility, safety and efficacy of harm reduction including NSP inprison settings (Meyenberg et al., 1999; Stöver and Nelles 2003).At present, NSPs have been established in prisons in nine countries worldwide (Lines et al.,2006), including six countries in Europe. Coverage of the national prison systems is, however,variable. In Spain, implementation of needle and syringe exchange is authorised in allprisons (see box below) and in 2006, programmes existed in 37 prisons (Acín García,2008). In Switzerland, NSPs are available in eight of 120 prisons, and in Germany,Luxembourg, Romania and Portugal such programmes operate in one or two prisons. Othercountries, including the United Kingdom (Scotland), are considering the implementation ofpilot projects (EMCDDA, 2009a; Lines et al., 2006). A review published in 2007 stated:Prison NSPs have been implemented in both men’s and women’s prisons, in institutions of varyingsizes, in both civilian and military systems, in institutions that house prisoners in individual cellsand those that house them in barracks, in institutions with different security ratings, and in differentforms of custody (remand and sentenced, open and closed).(Stöver et al., 2009, p. 83)
Prison-based needle and syringe exchange programmes in SpainSpanish prisons implement needle and syringe programmes (NSPs) via negotiated protocolsand frameworks based on consensus among all actors involved. Following the positiveexperience of pilot projects, the Spanish government made a commitment to expand availability,and in March 2001 the parliament approved a green paper recommending NSPs in all prisons.This was followed by a directive, in June 2001, from the Directorate General for Prisons requiringall prisons to implement NSPs. In October, there was a further similar directive from theSubdirectorate General for Prison Health setting January 2002 as the target. In March 2002,the Ministry of the Interior and the Ministry of Health and Consumer Affairs jointly publishedguidelines, policies, and procedures, and training and evaluation materials, for the nationalimplementation of prison-based NSPs. With these guidelines, every prison elaborates its ownNSPs. In order to implement, follow up and evaluate the programme:• Commission is created, with the Director and vice directors (including sanitary vice adirector) and representatives of security staff of the prison, as well as representatives of theDrug Dependence and AIDS Regional Programmes;• he needs of the prisoners and their patterns of drug use are assessed;t• he protocol for the NSP is developed; the attitudes of prisoners and staff are assessed;t• he implementation strategies are identified; and the evaluation designed.t(Stöver et al., 2007)The Ministry of Labour and Social Security endorsed this process with additional guidance onreducing potential harm to prison staff (Ministry of Labour and Social Security, 2002).
385
Harm reduction: evidence, impacts and challenges
Opioid substitution treatmentWhile opioid substitution treatment (OST) has become standard practice in community drugtreatment services in many European countries (EMCDDA, 2009a), the implementation ofOST in custodial settings in most European countries is still lagging behind the availabilityand quality of the treatment provision in the community (Kastelic et al., 2008; EMCDDA,2009d).Studies have indicated that OST initiated in the community is most likely to be discontinued inprisons (Stöver et al., 2004; Stöver et al., 2006; Michel, 2005; Michel and Maguet, 2003).This often leads to relapse both inside prisons and immediately after release, often withsevere consequences, as indicated by high mortality rates after release from prisons(Singelton et al., 2003). Many studies have also shown the benefits of OST for the health andsocial stabilisation of opioid-dependent individuals passing through the prison system(Stallwitz and Stöver 2007; Larney and Dolan, 2009).Substitution treatment has been widely recognised as an effective treatment for opioiddependence in the general community (Dolan et al., 1998; Farrell et al., 2001; Larney andDolan, 2009; UNODC et al., 2006) and as having crime reducing effects (Lind et al., 2005).Despite this and the fact that methadone and buprenorphine have been added to the WHOmodel list of essential medicines (WHO, 2005), it remains controversial for prisons,particularly in Eastern European countries where substitution treatment also only exists on alow level in the community (van der Gouwe et al., 2006). Nevertheless, experience hasclearly shown the benefits of this treatment in prisons (WHO et al., 2007; Heimer et al.,2005; Stöver et al., 2008b; Stöver and Michels, 2010).In countries that provide OST in prisons, it is most commonly used for short-termdetoxification, and less frequently as a maintenance treatment (Kastelic et al., 2008). In somecountries, such as Austria, England (see box on p. 387) and Spain, substitution treatment isprovided as standard therapy to many prisoners who began treatment in the community andare deemed likely to continue it after release (Stöveret al., 2004). In others it is either notavailable in prisons at all, although legally possible (Estonia and Lithuania), or only providedin very rare cases (Sweden). OST treatment that has been started in the community cannotlegally be continued in prisons in Slovakia, Latvia, Cyprus and Greece. New substitutiontreatments cannot be initiated in Slovakia, Latvia, Cyprus, Greece, Portugal, Finland andEstonia (EMCDDA, 2009a).Acknowledgement that the benefits of substitution treatment in the community might alsoapply to the prison setting has taken years. The sources of the controversy — and the slowand patchy manner of the intervention’s implementation thus far — can be traced first to theprisons’ general failure to provide adequate healthcare, with limited resources forpopulations with high concentrations of poor physical and mental health (Møller et al., 2007;Bertrand and Niveau, 2006). Second, due to the parallel prison healthcare system (separateto the national health services in most countries), responsibility for a prisoner’s medicaltreatment is often transferred to healthcare providers only after that prisoner has beenreleased. Third, the ethos of coercion and incapacitation manifests itself in a strict abstinence-
386
Chapter 14: Criminal justice approaches to harm reduction in Europe
based approach to drug use. Therefore, while opioid-dependent individuals in the communitymay be treated as patients and receive substitution treatment, in prison they continue to betreated as prisoners who are supposed to remain drug free. This double standard leads tofrequent interruptions in treatment and inconsistency in dosages, especially as many opioidusers spend substantial periods of time incarcerated.
Opioid substitution treatment (OST) in EnglandThe number of methadone maintenance (OST) treatments started in prisons in England hasincreased from 700 in 2003 (1) to 19 450 for the year 2008. All 130 adult prisons in thecountry are now funded to provide OST. Approximately 26 000 treatments are anticipatedfor 2009, rising to 39 000 for the year 2010 (Marteau and Stöver, 2010).Figure 14.3:Methadone maintenance treatments in prisons in England201020092008Year20072006200520042003051015202530354045
Number of prisoners treated (thousands)The massive expansion of OST in prisons is the result of: a shift of responsibility for prisonhealthcare from the Home Office to the National Health Service; political and professionalleadership and investment; and a strong investment in training and education of staff inprisons. With these efforts, the number of patients in prison-based OST has been increasedsubstantially over the past two years (Stöver et al., 2008b).This example shows that the Integrated Drug Treatment System (IDTS) has been welcomed bya large section of the health and criminal justice community. It has also helped the Britishgovernment to avoid repeated litigation by drug users who have been denied the appropriatetreatment (in the past, the government has had to settle cases on this) (Radcliffe and Stevens,2008; Marteau and Stöver, 2010). A large research programme will evaluate the processand outcomes of the IDTS.(1) Refers to the fiscal year 2003–04 which runs from 1 March 2003 until end February 2004. All dates cited in this boxfollow this pattern.
387
Harm reduction: evidence, impacts and challenges
Evidence shows that methadone maintenance treatment (MMT, the most studied form ofpharmacological drug treatment) can reduce risk behaviour in penal institutions, such asreduced frequency of illicit drug use in prison and reduced involvement in the prison drugtrade (Dolan et al., 1998; Kimber et al., 2010). Studies have also demonstrated thatmethadone maintenance treatment provision in a prison healthcare setting can be effective inreducing heroin use, drug injection and syringe sharing among incarcerated heroin users(Stöver and Marteau, 2010). A sufficiently high dosage also seems to be important forimproving retention rate, which helps in the provision of additional healthcare services (Dolanet al., 2002).There is evidence that continued MMT in prison has a beneficial impact on transferringprisoners into drug treatment after release. The initiation of MMT in prisons also contributes to asignificant reduction in serious drug charges and in behaviour related to activities in the drugsubculture. Offenders participating in MMT also had lower readmission rates and werereadmitted at a slower rate than non-MMT patients. For example, a 2001 evaluative study ofthe methadone programme of the Correctional Service of Canada (CSC) concluded thatparticipation in methadone programmes had positive post-release outcomes. The study foundthat opiate users accessing MMT during their incarceration were less likely to be readmitted toprison following their release — and were less likely to have committed new offences — thanwere those not accessing methadone. These findings have been supported by a more recentrandomised trial from the United States. It showed that prisoners who started methadonetreatment before release and continued after it were significantly more likely to stay away fromillicit drugs in the first year after release. Their outcomes were better than those achieved bysimilar prisoners who received only counselling in the prison, than if they were transferred tomethadone programmes on release (Kinlock et al. 2009; Stöver and Marteau 2010; Stöver andMichels, 2010).Studies have shown that prison staff tend to support the introduction of OST to a higherdegree than they support other harm reduction measures, such as syringe exchange (Allen,2001). Greater knowledge of substitution programmes is directly associated with morepositive attitudes towards it (McMillan and Lapham, 2005). This suggests that training forstaff on all levels may decrease resistance to substitution programmes and contribute topatient-oriented, confidential and ethical service delivery. Institutional constraints can also beovercome by highlighting the benefits of a substitution programme for the prison itself (Stöverand Marteau, 2010).Provision of bleach and disinfectantsMany prison systems have adopted programmes that provide disinfectants such as bleach toprisoners who inject drugs, as a means to clean injecting equipment before re-using it (seebox on p. 389). According to UNAIDS in 1997, the provision of full-strength bleach toprisoners as a measure had been successfully adopted in prisons in Europe, Australia, Africa,and Central America (UNAIDS, 1997). The WHO further reported that concerns that bleachmight be used as a weapon proved unfounded, and that this has not happened in any prisonwhere bleach distribution has been tried (WHO, 2007).388
Chapter 14: Criminal justice approaches to harm reduction in Europe
However, disinfection with bleach as a means of HIV prevention is of varying efficiency, andtherefore regarded only as a secondary strategy to syringe exchange programmes (WHO,2005). The effectiveness of disinfection procedures is also largely dependent upon themethod used. Before 1993, guidelines for syringe cleaning stipulated a method known as the‘2x2x2’ method. This method involved flushing injecting equipment twice with water, twicewith bleach and twice with water. Research in 1993 raised doubts about the effectiveness ofthis method in the decontamination of used injecting equipment, and recommended newcleaning guidelines where injecting equipment should be soaked in fresh full-strength bleach(5 % sodium hypochlorite) for a minimum of 30 seconds (Shapshank et al., 1993).All of these developments further complicate the effective use of bleach and disinfectants inprison settings, where fear of detection by prison staff and lack of time often means thathygienic preparation of equipment and drug use happens quickly, and that prisoners willoften not take the time to practise optimal disinfection techniques (WHO, 2005). Furthermore,bleach is effective in killing the HIV virus, but may be less effective for the hepatitis C virus.Training drug users to clean syringes with bleach may provide the user with false reassuranceregarding the risk of re-using injecting equipment. Despite these limitations, provision ofdisinfectants to prisoners remains an important option to reduce the risk of HIV transmission,particularly where access to sterile syringes is not available. The Royal College of GeneralPractitioners concluded that ‘[o]n current evidence it would be difficult to support a policy ofnot distributing bleach’ (2007, p. 13).By August 2001, bleach was provided in 11 of 23 pre-expansion EU prison systems (Stöver et al.,2004). Disinfectants are also made available to prisoners in Canada, England and Wales, Iran,Kyrgyzstan, Moldova, Turkmenistan, Switzerland, and some parts of the Russian Federation.
Provision of bleach in Austrian prisonsIn all 28 Austrian prisons, anonymous access (in most parts of the prison system) to disinfectantsin order to avoid the transmission of blood-borne viruses (BBV) via sharing of needles andequipment is provided. The Austrian Ministry of Justice stated in several orders (‘Erlass’) thatbeside condoms, the disinfectant Betaisadona should be made available freely andanonymously in all prisons. The primary purpose is the cleaning of injection equipment andthe treatment of injection punctures. In this context the target group are not only drug usersbut also those prisoners involved in tattooing. Implementation, however, is varied, with limitedstaff resources being a factor.
Provision of condoms, dental dams, and water-based lubricantsMany prisons globally provide condoms to prisoners as part of their institutional health andSTI prevention policies. This is in keeping with the recommendation of the WHO Guidelines,‘Since penetrative sexual intercourse occurs in prison, even when prohibited, condoms shouldbe made available to prisoners throughout their period of detention. They should also bemade available prior to any form of leave or release’ (WHO, 1993).389
Harm reduction: evidence, impacts and challenges
Multiple barriers exist to the use of condoms in many prisons, and there is often poorknowledge among prisoners of sexual risk behaviour and risk reduction (MacDonald, 2005;Todts et al., 1997; UNODC et al., 2006). These barriers include prison rape, the social stigmaattached to homosexuality and same-sex activities, and insufficient privacy to enable safersex. Furthermore, condoms, dental dams, and water-based lubricants are often theoreticallyavailable but often not easily and discreetly accessible, at least not available on a 24-hourbasis. Prisoners may be reluctant to access safer sex measures for fear of identifyingthemselves as engaging in such activities.Evidence suggests that the provision of condoms is feasible in a wide range of prisonsettings (WHO et al., 2007). No prison system enabling condom distribution has reversedthis policy, and none have reported security problems or any major negativeconsequences. Research also demonstrates the importance of identifying the factorsshaping resistance among stakeholders and prison officials to introducing harm reductionmeasures in custodial settings, including condom distribution (Jürgens et al., 2009; Stöveret al., 2007). The orientation of ministries of justice, public opinion, and prison systemfinancial constraints are all factors shaping staff acceptance or resistance to implementingharm reduction, and it is important to develop tailor-made strategies to address these(Marteau and Stöver 2010; Stöver et al., 2009).
Through-care and aftercarePrison may be the place where drug-related harms are most visible and acute, but the vastmajority of prisoners will one day be released. According to Williamson (Williamson, 2006)the major challenge for prison healthcare is:to enable continuity of care, within, between, on admission and upon release. Using the prisonerjourney from pre-arrest to post release as a template it will be possible for local health and socialcare, and criminal justice communities to better plan continuity of health and social care,alternatives to imprisonment and long term support services.(Williamson, 2006, p.5)
Several studies have shown that effective and rapid access to aftercare for drug-usingprisoners is essential to maintain gains made in prison-based treatment (e.g. Zurhold et al.,2005; Inciardi et al., 1997; Department of Health/National Offender Management Service,2009). Prisoners are marginalised in society and tend to fall into the gaps between caresystems and structures, which find it hard to deal with multiple needs. Care should be takento overcome this tendency. From previous studies on recidivism following in-prisontreatment (e.g. Inciardi et al., 1997), maintaining therapeutic relationships initiated in theprison into the post-release period would be likely to reduce recidivism and improve healthoutcomes. Prisons can be places of relative safety and health promotion for prisoners.Many people slip back into less healthy habits when they leave this structured environment.The box on p. 391 gives an example of a promising programme that seeks to avoid thisdanger.390
Chapter 14: Criminal justice approaches to harm reduction in Europe
The ‘Through the Gates’ serviceMany prisoners, including a high proportion of those with drug problems, leave prison with nohome to go to. This increases the likelihood that they will continue risky patterns of drug use andoffending. In response to this problem, the St Giles Trust (a non-governmental organisationbased in London) set up the ‘Through the Gates’ service. This service employs a team ofcaseworkers (half of whom are themselves ex-offenders) to work with individual prisoners. Thecaseworkers go to meet prisoners before they are released in order to assess their housing andother needs. They then meet the prisoner at the gate of the prison on the day of their release.The worker accompanies the client to initial meetings with the housing service, with probationofficers and, when necessary, drug treatment services. In the first year of this service, 70 % ofthe homeless clients it worked with were successfully placed in temporary or permanentaccommodation. Probation officers reported that the service dramatically increased the chancesof successful resettlement. Some clients reported that it was the first time that they had beenhelped to step off the repetitive treadmill of imprisonment, drug use and crime.
The following conclusions were drawn by a multi-country survey of key informants onaftercare programmes for drug-using prisoners in several European countries (Fox, 2000):• ftercare for drug-using prisoners significantly decreases recidivism and relapse rates and Asaves lives.• nteragency cooperation is essential for effective aftercare. Prisons, probation services, Idrug treatment agencies and health, employment and social welfare services must join upto meet the varied needs of drug-using offenders.• hort-sentence prisoners are the most poorly placed to receive aftercare and most likely to Sre-offend. These prisoners need to be fast-tracked into release planning and encouragedinto treatment.• x-prisoners need choice in aftercare. One size does not fit all in drug treatment.E• ftercare that starts in the last phase of a sentence appears to increase motivation and uptake.A• n aftercare, housing and employment should be partnered with treatment programmes. IUnemployed and homeless ex-prisoners are most likely to relapse and re-offend.• rug treatment workers must have access to prisoners during their sentence to encourage Dparticipation in treatment and to plan release.As the mortality risks due to overdose are most critical in the first week after release(Singleton et al., 2003; Farrell and Marsden, 2008), all harm reduction measures to preventoverdose or drug-related infections should be available and accessible.
Earlier stages of the criminal justice systemAs with prisons and through-care, the practice and policy of the police with regard to harmreduction varies throughout Europe, dependent on different legal backgrounds. What can befound all over Europe is a high level of formal or informal discretion (EMCDDA, 2002). The391
Harm reduction: evidence, impacts and challenges
police on the street can simply turn a blind eye towards illicit behaviour, or the officialstrategy of the police might pro-actively support harm reduction. The basis for these choicesis a growing awareness of the adverse effects of control and custody with regard to thehealth of drug users and thus an increasing acknowledgment of all forms of support,assistance, counselling and treatment for this target group.The introduction of policing practices that are more open to harm reduction interventions cancontribute substantially to reducing some of the negative consequences of police patrolling,such as a reluctance to carry syringes and unsafe disposal, hurried and unsafe preparationof injection, and the potential for police attention to deter drug users from going to treatmentcentres (MacDonald et al., 2008). The availability of an injection location that is safe frompolice interference is a significant harm reduction measure (Kerr et al., 2008). Drugconsumption rooms are an interesting model of accepting an unlawful behaviour (possessionand consumption of drugs) for the sake of the health of the drug users. In most countrieswhere they operate, these facilities are not only tolerated, but also demanded and supportedby the police, who also facilitate their use (DeBeck et al., 2008). Furthermore, the policemostly see drug consumption rooms as a ‘win–win’ situation, as they spend less of their timedealing with users, and therefore have more resources available to target dealers. Inaddition, drug consumption is no longer taking place in the local area and causing publicnuisance, but is taking place under hygienic and less visible circumstances (Stöver, 2002;Hedrich et al., 2010). The success of drug consumption rooms depends on the policeagreeing not to target drug users within and around them.There are other examples in Europe of structured combinations of harm reduction and crimeprevention approaches. Arrest referral programmes, which first appeared in the UnitedKingdom in the 1980s and were expanded at national level by the Home Office Circular in1999, are an example of a criminal justice-based programme that can introduce drug usersto treatment and harm reduction services (Seeling et al., 2001). Arrest referral placesspecially trained substance use assessment workers in police stations to counsel and referdrug-using arrestees who voluntarily request assistance with their drug-related problems.Arrest referral schemes provide an access point for new entrants to services. Data from thenational monitoring programme in England and Wales showed that half (51 %) of all thosescreened by an arrest referral worker had never accessed specialist drug treatment services(Sondhi et al., 2002). This implies that arrest referral is successful in contacting problem drug-using offenders at an earlier point than they might have otherwise considered using services.Outcomes of the arrest referral schemes included consistent reductions in drug use andoffending behaviour among problem drug-using offenders who have been engaged in thescheme (Sondhi et al., 2002).However, arrest referral often suffers from low rates of retention, with large proportions of thecontacted drug users not going on to contact services (Edmunds et al., 1998). In England andWales, the Drug Intervention Programme was supplemented by a system of casemanagement of drug-using offenders and, since 2005, testing on arrest and requiredassessments in order to address this problem. These latter measures enable the police torequire a person arrested for any one of a specific list of offences to undergo a drug test. Ifthe test is positive for cocaine or heroin, the person can then be ordered to attend an392
Chapter 14: Criminal justice approaches to harm reduction in Europe
assessment with a drug treatment worker. The effect of these measures has not beenevaluated. They have brought more drug users into treatment assessments, but many of themhave been recreational users of cocaine who see no need to enter treatment.At the stage of arrest, many drug users face risks associated with the seizure of their injectingequipment, as this increases the risks of syringe sharing the next time they use drugs. Theprovision of syringe exchange within police custody could reduce this risk. The revised 2007ACPO Drug Strategy for Scotland, as well as reaffirming the support of police forces forharm reduction interventions, also acknowledges the role of the introduction of syringeexchange schemes in custody suites. As MacDonald et al. (2008) have stated:Research has demonstrated that the police can have a role in harm reduction provision, withoutnecessarily compromising their legal and moral values. For example, they can encourage usersin detention to make use of local needle exchange sites and provide information on their location,and they can use discretion in not arresting users at such sites, while consulting with the communityon the need for such methods.(MacDonald et al., 2008, p. 6)
Early interventions have been implemented in many European states to avoid the negativeimpact of both continuous untreated drug addiction and conviction and possiblyincarceration. ‘FreD goes net’ is a European network of such early intervention projects,which are diverting young drug users from police to counselling agencies to avoid adverseeffects of the criminal justice system (LWL, 2009).In a number of European countries legislation expands the options available to the courts forthe diversion of drug-related offenders away from the criminal justice system to treatment, orfor court-mandated treatment to form part of a sentence (EMCDDA, n.d.). Although data onusage of these options remain rare (European Commission, 2008), it seems they havehistorically been under-used (Turnbull and Webster, 1997). Few have been formally evaluated(Hough et al., 2003). Those that have been evaluated have tended to show that treatment thatis entered through the legal system can be as effective as when people enter through othermodes (McSweeney et al., 2007; Stevens et al., 2005). The under-exploitation of opportunitiesto divert drug users from the criminal justice system through alternative measures toimprisonment remains a major problem — particularly in new Member States of the EuropeanUnion — which demands further investigation and action. In Cyprus in 2008, for example, alaw had existed since 1992 that enabled drug-using offenders to be diverted into treatment, butno suitable treatments were in place and so the law was not used (Fotsiou, 2008).
ConclusionThe evidence and examples provided in this chapter have shown that it is possible tonegotiate the tensions between law enforcement and harm reduction. Services have beensuccessfully implemented that have reduced the harms experienced by drug users in thecriminal justice system. However, implementation in many countries remains at the levelof discussion, or small pilot projects. It is rare that countries actually practice the principle393
Harm reduction: evidence, impacts and challenges
of equivalence between services inside and outside prisons to which they have signedup. And the chances of rapid extension of harm reduction in criminal justice systems mayseem to be low, given the current scale of economic uncertainty and strains on the publicpurse.Nevertheless, given the frequent contact between drug users and criminal justice systems,and ongoing epidemics of blood-borne viruses linked to problem drug use, there is an urgentneed for harm reduction services to be scaled-up. Reducing the numbers of drug users inprison will be the least costly means of increasing the proportion of prisoners who haveaccess to harm reduction. It would reduce demand for drug services in prison and would freeup resources to spend on harm reduction and other services, assuming that these resourcesare not diverted away from working with drug users.Additional challenges remain. These include the need to develop and expand services fornon-opiate users (such as methamphetamine users in parts of Eastern Europe, and cocaine/crack users in the United Kingdom; see Decorte, 2008; Hartnoll et al., 2010), as well as thechallenge of involving drug users themselves in the design and delivery of harm reductionservices (see Hunt et al., 2010), which are especially severe when those drug users aresubject to the criminal justice system.All elements of the criminal justice system have roles to play in the reduction of drug-relatedharm, including police officers, prosecutors, courts, prisons, probation services and non-governmental organisations that work with offenders. Harm reduction is a challenge for lawenforcement, and law enforcement is a challenge for harm reduction. The contradictionsbetween the aims of these two approaches cannot be wished away. However, we can protectboth public health and individual rights to healthcare by acknowledging these tensions andfinding ways to move beyond them to provide high-quality harm reduction services to allwho need them.
AcknowledgementsThe authors’ gratitude goes to the various reviewers of this chapter who helped us to improveit and to the EMCDDA for providing useful information.
ReferencesAcín García, E. J. (2008), ‘Unenfoque global sobre la prevención y el control del VIH en las prisiones de España’,Secretaría General de instituciones Penitenciarias, Ministerio del Interior, Gobierno de España, presentation atthe Internacional Harm Reduction Conference, Bangkok 2008.Allen, A-M. (2001),Drug-related knowledge and attitudes of prison officers in Dublin prisons,Thesis submitted forthe degree of M.Sc. in Community Health, Department of Community Health and General Practice, TrinityCollege, Dublin, October.
394
Chapter 14: Criminal justice approaches to harm reduction in Europe
Allwright, S., Bradley, F., Long, J., et al. (2000), ‘Prevalence of antibodies to hepatitis B, hepatitis C, and HIV andrisk factors in Irish prisoners: results of a national cross sectional survey’,British Medical Journal321 (7253), pp.78–82.Bean, P. (2008),Drugs and crime,3rd edition, Willan Publishing, Cullompton.Bertrand, D. and Niveau, G. (eds) (2006),Médecine, santé et prison,Editions Medecine & Hygiene, Chene-Bourg.Bravo, M. J., de la Fuente, L., Pulido, J., et al. (2009), ‘Spanish HIV/AIDS epidemic among IDUs and the policyresponse from an historical perspective’, Presentation at the 5th European Conference on Clinical and SocialResearch on AIDS and Drugs, Vilnius, 28–30 April 2009.Carter, A. and Hall, W. (2010, in press), ‘The rights of individuals treated for drug, alcohol and tobaccoaddiction’, in Dudley, M., Silove, D. and Gale, F. (eds) (2010),Mental health and human rights,Oxford UniversityPress, Oxford.Caulkins, J. P. and Reuter, P. (2009), ‘Towards a harm-reduction approach to enforcement’,Safer Communities8(1), pp. 9–23.Christie, N. (1982),Limits to pain,Martin Robertson, Oxford.Cook, C. (2009),Harm reduction policy and practice worldwide: an overview of national support for harm reductionin policy and practice,International Harm Reduction Association, Victoria and London. Available at http://www.ihra.net/HRWorldwide.Cook, C., Bridge, J. and Stimson, G. V. (2010), ‘The diffusion of harm reduction in Europe and beyond’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Commission on Narcotic Drugs (2002),Preventing the transmission of HIV among drug abusers: a position paper ofthe United Nations system, endorsed on behalf of ACC by the High-Level Committee on Programme (HLCP) at its firstregular session of 2001, Vienna, 26–27February 2001,document E/CN.7/2002/CRP.5 for participants at theForty-fifth session, Vienna, 11–15 March 2002. Available at http://www.cicad.oas.org/en/Resources/UNHIVaids.pdf.Crawley, D. (2007),Good practice in prison health,Department of Health, London.DeBeck, K., Wood, E., Zhang, R., et al. (2008), ‘Police and public health partnerships: evidence from theevaluation of Vancouver’s supervised injection facility’,Substance Abuse Treatment Prevention PolicyMay, 7 (3),p. 11. DOI: 10.1186/1747-597X-3-11.Decorte, T. (2008), ‘Problems, needs and service provision related to stimulant use in European prisons’,International Journal of Prisoner Health3 (1), pp. 29–42. Available at http://dx.doi.org/10.1080/17449200601149122.Department of Health/National Offender Management Service (2009),Guidance notes: prison healthperformance and quality indicators,Department of Health, London. Available at http://www.hpa.nhs.uk/web/HPAwebFile/HPAweb_C/1232006593707.Dolan, K. and Wodak, A. (1999), ‘HIV transmission in a prison system in an Australian State’,Medical Journal ofAustralia171 (1), pp. 14–17.Dolan, K. A., Wodak, A. D. and Hall, W. D. (1998), ‘Methadone maintenance treatment reduces heroin injectionin New South Wales prisons’,Drug and Alcohol ReviewJune, 17 (2), pp. 153–8.
395
Harm reduction: evidence, impacts and challenges
Dolan, K., Shearer, J., White, B. and Wodak, A. (2002),A randomised controlled trial of methadone maintenancetreatment in NSW prisons,National Drug and Alcohol Research Centre, Sydney.Dolan, K., Khoei, E. M., Brentari, C. and Stevens, A. (2007)Prisons and drugs: a global review of incarceration,drug use and drug services. Report 12. Discussion paper,The Beckley Foundation, Oxford. Available at http://kar.kent.ac.uk/13324/.Dorn, N. and South, N. (1990), ‘Drug markets and law enforcement’,British Journal of Criminology30 (2), pp.171–88.Dublin Declaration on HIV/AIDS in Prisons in Europe and Central Asia (2004),Prison health is public health,IrishPenal Reform Trust, Dublin.Duke, K. (2003),Drugs, prisons and policy-making,Palgrave, Basingstoke.ECOSOC (United Nations Economic and Social Council) (2009),Political declaration and plan of action oninternational cooperation towards an integrated and balanced strategy to counter the world drug problem,UnitedNations, Vienna.Edmunds, M., May, T., Hearnden, I. and Hough, M. (1998),Arrest referral: emerging lessons from research,HomeOffice, London.EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (n.d.),Treatment as an alternative toprosecution or imprisonment for adults,ELDD Topic overview, European Monitoring Centre for Drugs and DrugAddiction, Lisbon. Available at http://eldd.emcdda.europa.eu/html.cfm/index13223EN.html (accessed 3December 2009).EMCDDA (2002),Prosecution of drug users in Europe: varying pathways to similar objectives,Insights series number5, European Monitoring Centre for Drugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/html.cfm/index33988EN.html.EMCDDA (2005),Alternatives to imprisonment: targeting offending problem drug users in the EU,Selected issue,European Monitoring Centre for Drugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/html.cfm/index34889EN.html.EMCDDA (2009a),Annual report 2009: the state of the drugs problem in Europe,European Monitoring Centre forDrugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/publications/annual-report/2009.EMCDDA (2009b), Statistical bulletin 2009,Table HSR-7: availability and level of provision of selected healthresponses to prisoners in 26 EU countries, Norway and Turkey (expert ratings),European Monitoring Centre forDrugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/stats09/hsrtab7.EMCDDA (2009c), Statistical bulletin 2009, Table HSR-4: year of introduction of needle and syringe programmesand types of programmes (NSP) available in 2007, European Monitoring Centre for Drugs and Drug Addiction,Lisbon. Available at http://www.emcdda.europa.eu/stats09/hsrtab4.EMCDDA (2009d), Statistical bulletin 2009, Figure HSR-2: provision of substitution/maintenance treatment (OST)in the community and availability of OST programmes in the prison system in 2007 (expert rating), EuropeanMonitoring Centre for Drugs and Drug Addiction, Lisbon. Available at http://www.emcdda.europa.eu/stats09/hsrfig2.European Commission (2007), ‘Report from the Commission to the European Parliament and the Council on theimplementation of the Council Recommendation of 18 June 2003 on the prevention and reduction of health-related harm associated with drug dependence’, COM (2007) 199 final. Available at http://eur-lex.europa.eu/LexUriServ/site/en/com/2007/com2007_0199en01.pdf.
396
Chapter 14: Criminal justice approaches to harm reduction in Europe
European Commission (2008),Commission staff working document: accompanying document to the communicationfrom the Commission to the Council and the European Parliament on an EU drugs action plan 2009–2012. Report ofthe final evaluation of the EU drugs action plan (2005–2008),COM(2008) 567, SEC(2008) 2455, SEC(2008)2454, European Community, Brussels. Available at http://eur-lex.europa.eu/SECMonth.do?year=2008&month=09.Farrell, M. and Marsden, J. (2008), ‘Acute risk of drug-related death among newly released prisoners in Englandand Wales’,AddictionFebruary 103 (2), pp. 251–5.Farrell, M., Gowing, L. R., Marsden, J. and Ali, R. L. (2001), ‘Substitution treatment for opioid dependence: areview of the evidence and the impact’, in Council of Europe (ed.),Development and improvement of substitutionprogrammes: proceedings of a seminar organized by the Cooperation Group to combat Drug Abuse and IllicitTrafficking in Drugs (Pompidou Group),Strasbourg, France, 8–9 October 2001, pp. 27–54.Fazel, S., Bains, P. and Doll, H. (2006), ‘Substance abuse and dependence in prisoners:a systematic review’,Addiction101 (2), pp. 181–91.Fotsiou, N. (2008), Personal communication, Cyprus Anti-Drugs Council, Nicosia.Fox, A. (2000),Prisoners’ aftercare in Europe: a four countries study,European Network of Drug and HIV/AIDSServices in Prison (ENDHASP), Cranstoun Drug Services, London.Gendreau, P., Goggin, C. and Cullen, F. T. (1999),The effects of prison sentences on recidivism,Solicitor GeneralCanada, Public Works and Government Services Canada, Ottawa. Available at http://www.prisonpolicy.org/scans/gendreau.pdf.Greenwald, G. (2009),Drug decriminalization in Portugal: lessons for creating fair and successful drug policies,Cato Institute, Washington, DC. Available at http://www.cato.org/pub_display.php?pub_id=10080.Hagan, H. (2003), ‘The relevance of attributable risk measures to HIV prevention planning’,AIDS17, pp. 911–13.Hartnoll, R., Gyarmarthy, A. and Zabransky, T. (2010), ‘Variations in problem drug use patterns and theirimplications for harm reduction’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harmreduction: evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No.10, Publications Office of the European Union, Luxembourg.Hassim, A. (2006), ‘The “5 star” prison hotel: the right of access to ARV treatment for HIV positive prisoners inSouth Africa’,International Journal of Prisoner Health2 (3), pp. 157–72.Hedrich, D. (2004),European report on drug consumption rooms,European Monitoring Centre for Drugs and DrugAddiction, Lisbon. Available at http://www.emcdda.europa.eu/html.cfm/index54125EN.html.Hedrich, D., Kerr, T. and Dubois-Arber, F. (2010), ‘Drug consumption facilities in Europe and beyond’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Heimer, R., Catania, H., Zambrano, J. A., et al. (2005), ‘Methadone maintenance in a men’s prison in PuertoRico: a pilot program’,Journal of Correctional Health Care, The Official Journal of the National Commission onCorrectional Health Care11 (3), pp. 295–306.Hough, M., Clancy, A., McSweeney, T. and Turnbull, P. J. (2003), ‘The impact of drug treatment and testingorders on offending: two year reconviction results’,Home Office Research FindingsNo. 184, Home Office,London.
397
Harm reduction: evidence, impacts and challenges
Hughes, C. and Stevens, A. (2007),The effects of the decriminalization of drug use in Portugal,BeckleyFoundation, Oxford. Available at http://www.idpc.net/php-bin/documents/BFDPP_BP_14_EffectsOfDecriminalisation_EN.pdf.pdf.Hunt, N. (2003),A review of the evidence-base for harm reduction approaches to drug use,Forward Thinking onDrugs, London. Available at http://www.iprt.ie/contents/1328.Hunt, N., Albert, E. and Montañés Sánchez, V. (2010), ‘User involvement and user organising in harm reduction’,in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.IDT (Instituto da Droga e da Toxicodependência) (2005),Relatório anual 2004 — A situa§ão do país em matériade drogas e toxicodependências. Volume I - Informa§ão estatística,Instituto da Droga e da Toxicodependência,Lisbon. Available at http://www.idt.pt.IDT (2006),Relatório anual 2005 — A situa§ão do país em matéria de drogas e toxicodependências. Volume I -Informa§ão estatística,Instituto da Droga e da Toxicodependência, Lisbon. Available at http://www.idt.pt.IDT (2007),Portugal: new developments, trends and in-depth information on selected issues: 2006 National report(2005 data) to the EMCDDA by the Reitox National Focal Point,Instituto da Droga e da Toxicodependência, Lisbon.Available at http://www.idt.pt.Inciardi, J. A., Martin, S. S., Butzin, C. A., Hooper, R. M. and Harrison, L. D. (1997), ‘An effective model ofprison-based treatment for drug-involved offenders’,Journal of Drug Issues,27 (2), pp. 261–78.Jürgens, R., Ball, A. and Verster, A. (2009), ‘Interventions to reduce HIV transmission related to injecting drug usein prison’,Lancet Infectious Diseases9, pp. 57–66.Kastelic, A., Pont, J. and Stöver, H. (2008),Opioid substitution treatment in custodial settings: a practical guide,BIS-Verlag, Oldenburg. Available at http://www.unodc.org/documents/baltics/OST%20in%20Custodial%20Settings.pdf.Keppler, K., Nolte, F. and Stöver, H. (1996), ‘Übertragungen von Infektionskrankheiten im Strafvollzug —Ergebnisse einer Untersuchung in der JVA für Frauen in Vechta [Transmission of infectious diseases in prison:results of a study in the prison for women in Vechta]’,Sucht42 (2), pp. 98–107. Available at http://www.neuland.com/index.php?s=sxt&s2=inh&s3=1996204.Kerr, T., Macpherson, D. and Wood, E. (2008), ‘Establishing North America’s first safer injection facility: lessonsfrom the Vancouver experience’, in Stevens, A. (ed.),Crossing frontiers: international developments in the treatmentof drug dependence,Pavilion Publishing, Brighton, pp. 109–29.Kimber, J., Palmateer, N., Hutchinson, S., et al. (2010), ‘Harm reduction among injecting drug users: evidence ofeffectiveness’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction:evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10,Publications Office of the European Union, Luxembourg.Kinlock, T. W., Gordon, M. S., Schwartz, R. P., Fitzgerald, T. T. and O’Grady, K. E. (2009), ‘A randomizedclinical trial of methadone maintenance for prisoners: results at 12 months postrelease’,Journal of SubstanceAbuse Treatment37, pp. 277–85Kovandzic, T. V. and Vieraitis, L. M. (2006), ‘The effect of county-level prison population growth on crime rates’,Criminology and Public Policy5 (2), pp. 213–44.Larney, S. and Dolan, K. (2009), ‘A literature review of international implementation of opioid substitutiontreatment in prisons: equivalence of care?’,European Addiction Research15, pp. 107–12.
398
Chapter 14: Criminal justice approaches to harm reduction in Europe
Lind, B., Chen, S., Weatherburn, D. and Mattick, R. (2005), ‘The effectiveness of methadone maintenancetreatment in controlling crime: an Australian aggregate-level analysis’,British Journal of Criminology45 (2), pp.201–11.Lines, R. (2008), ‘The right to health of prisoners in international human rights law’,International Journal ofPrisoner Health4 (1), pp. 3–53.Lines, R., Jürgens, R., Betteridge, G., et al. (2006),Prison needle exchange: lessons from a comprehensive review ofinternational evidence and experience,2nd edition, Canadian HIV/AIDS Legal Network, Toronto. Available athttp://www.aidslaw.ca/publications/publicationsdocEN.php?ref=184.LWL (Landschaftsverband Westfalen-Lippe) (2009),Fred goes net: Early intervention for young drug users,Landschaftsverband Westfalen-Lippe, Münster. Available at http://www.lwl.org/LWL/Jugend/lwl_ks/Projekte_KS1/Fgn-english/.MacCoun, R. J. and Reuter, P. (2001),Drug war heresies: learning from other vices, times, and places,CambridgeUniversity Press, Cambridge.MacDonald, M. (2005),A study of health care provision, existing drug services and strategies operating in prisons inten countries from central and eastern Europe,Heuni, Helsinki. Available at http://www.heuni.fi/12542.htm.MacDonald, M., Atherton, S., Berto, D., et al. (2008),Service provision for detainees with problematic drug andalcohol use in police detention: a comparative study of selected countries in the European Union,Paper No. 27,European Institute for Crime Prevention and Control, affiliated with the United Nations (HEUNI), Helsinki.McMillan, G. P. and Lapham, S. C. (2005), ‘Staff perspectives on methadone maintenance therapy (MMT) in alarge southwestern jail’,Addiction Research and Theory13 (1), pp. 53–63.McSweeney, T., Stevens, A., Hunt, N. and Turnbull, P. (2007), ‘Twisting arms or a helping hand? Assessing theimpact of “coerced” and comparable “voluntary” drug treatment options’,British Journal of Criminology47 (3),pp. 470–90.Marteau, D. and Stöver, H. (2010, in press), ‘The introduction of the prisons “Integrated Drug Treatment System(IDTS)” in England’,International Journal of Prisoner Health.Mathiesen, T. (2006),Prison on trial,3rd edition, Waterside Press, Winchester.Matic, S., Lazarus, J. V., Nielsen, S. and Laukamm-Josten, U. (eds) (2008),Progress on implementing the DublinDeclaration on Partnership to Fight HIV/AIDS in Europe and Central Asia,WHO Regional Office for Europe,Copenhagen. Available at http://www.euro.who.int/document/e92606.pdf.Meyenberg, R., Stöver, H., Jacob, J. and Pospeschill, M. (1999),Infektionsprophylaxe im NiedersächsischenJustizvollzug — Abschlußbericht,BIS-Verlag, Oldenburg.Michel, L. (2005), ‘Substitutive treatments for major opionic dependance adapted to prison life’,InformationPsychiatrique81 (5), pp. 417–22.Michel, L. and Maguet, O. (2003),L’organisation des soins en matière de traitements de substitution en milieucarcéral, Rapport pour la Commisssion nationale consultative des traitements de substitution,Centre Régionald’Information et de Prévention du Sida Ile-de-France, Paris.Michel, L., Carrieri, P. and Wodak, A. (2008), ‘Harm reduction and equity of access to care for French prisoners:a review’,Harm Reduction Journal5, p. 17. DOI: 10.1186/1477-7517-5-17.Ministry of Labour and Social Security (2002),Instruction 101/2002 of the Directorate General on Labour Inspectionand Social Security on criteria of action in connection with the implementation in a number of prisons of the needleexchange program for injecting drug users, 23.August 2002, Ministry of Labour and Social Security, Madrid.
399
Harm reduction: evidence, impacts and challenges
Møller, L, Stöver, H., Jürgens, R., Gatherer, A. and Nikogosian, H. (eds) (2007),Health in prisons: a WHO guideto the essentials in prison health,WHO Regional Office for Europe, Copenhagen.Offender Health Research Network (2009), Website. Available at http://www.ohrn.nhs.uk (accessed 19 August2009).Parliamentary Assembly of the Council of Europe (1988),Recommendation 1080 on a co-ordinated Europeanhealth policy to prevent the spread of AIDS in prison,Council of Europe, Strasbourg. Available at http://assembly.coe.int/documents/AdoptedText/ta88/erec1080.htm.Pont, J. (2008), ‘Ethics in research involving prisoners’,International Journal of Prisoner Health4 (4), pp. 184–97.Radcliffe, P. and Stevens, A. (2008), ‘Are drug treatment services only for “thieving junkie scumbags”? Drug usersand the management of stigmatised identities’,Social Science and Medicine67 (7), pp. 1065–73.Reiner, R. (2000), ‘Crime and control in Britain’,Sociology: The Journal of the British Sociological Association,34(1), pp. 71–94.Ritter, A. and Cameron, J. (2005),Monograph no. 06: a systematic review of harm reduction,DPMP MonographSeries, Turning Point Alcohol and Drug Centre. Fitzroy.Rolles, S. and Kushlick, D. (2004),After the war on drugs,Transform, Bristol.Rotily, M., Weilandt, C., Bird, S. M., et al. (2001), ‘Surveillance of HIV infection and related risk behaviour inEuropean prisons: A multicentre pilot study’,European Journal of Public Health11 (3), 243–50.Royal College of General Practitioners (2007),Guidance for the prevention, testing, treatment and management ofhepatitis C in primary care,Royal College of General Practitioners, London. Available at http://www.smmgp.org.uk/download/guidance/guidance003.pdf.Seeling, C., King, C., Metcalfe, E., Tober, G. and Bates, S. (2001), ‘Arrest referral: a proactive multi-agencyapproach’,Drugs: Education, Prevention and Policy8, pp. 327–33.Shapshank, P., McCoy, C., Rivers, J. , et al. (1993), ‘Inactivation of Human Immunodeficiency Virus-1 at short timeintervals using undiluted bleach’,Journal of Acquired Immune Deficiency Syndromes6, pp. 218–19.Singleton, N., Meltzer, H. and Gatward, R. (1997),Psychiatric morbidity among prisoners: summary report,National Statistics, London. Available at http://www.statistics.gov.uk/downloads/theme_health/Prisoners_PsycMorb.pdf.Singleton, N., Pendry, E., Taylor, C., Farrell, M. and Marsden, J. (2003), ‘Drug-related mortality among newlyreleased offenders’,Findings 187,Home Office, London. Available at http://www.homeoffice.gov.uk/rds/pdfs2/r187.pdf.Sondhi, A., O’Shea, J. and Williams, T. (2002), ‘Arrest referral: emerging findings from the national monitoringand evaluation programme’,DPAS Briefing Paper 18,Home Office Drug Prevention Advisory Service, London.Stallwitz, A. and Stöver, H. (2007), ‘The impact of substitution treatment in prisons: a literature review’,International Journal of Drug Policy18, pp. 464–74.Stevens, A. (2008), ‘Alternatives to what? Drug treatment alternatives as a response to prison expansion andovercrowding’, Presentation at the 2nd Annual Conference of the International Society for the Study of DrugPolicy, 3–4 April 2008, Lisbon.Stevens, A. (forthcoming), ‘Treatment sentences for drug users: contexts, mechanisms and outcomes’, inHucklesby, A. and Wincup, E. (eds),Drug interventions and criminal justice,Milton Keynes.
400
Chapter 14: Criminal justice approaches to harm reduction in Europe
Stevens, A., Berto, D., Heckmann, W., et al. (2005), ‘Quasi-compulsory treatment of drug dependent offenders:an international literature review’,Substance Use and Misuse40, pp. 269–83.Stevens, A., Bewley-Taylor, D. and Dreyfus, P. (2009),Drug markets and urban violence: can tackling one reducethe other?,Beckley Foundation, Oxford.Stöver, H. (1994), ‘Infektionsprophylaxe im Strafvollzug’, in Stöver, H. (ed.),Infektionsprophylaxe im Strafvollzug.Eine Übersicht über Theorie und Praxis (Vol. XIV),Deutsche AIDS-Hilfe, Berlin, pp. 13–40.Stöver, H. (2001),An overview study: assistance to drug users in European Union prisons,EMCDDA, Lisbon.Stöver, H. (2002), ‘Consumption rooms: a middle ground between health and public order concern’,Journal ofDrug Issues32 (2), pp. 597–606.Stöver, H. (ed.) (2008),Evaluation of national responses to HIV/AIDS in prison settings in Estonia: evaluation carriedout on behalf of the UNODC Regional project ‘HIV/AIDS prevention and care among injecting drug users and inprison settings in Estonia, Latvia and Lithuania’,UNODC, New York. Available at http://www.unodc.org/documents/baltics/Report_Evaluation_Prisons_2008_Estonia.pdf.Stöver, H. and Marteau, D. (2010, in press), ‘Scaling-up of opioid substitution treatment in custodial settings:evidence and experiences’,International Journal of Prisoner Health.Stöver, H. and Michels, I. I. (2010, in press), ‘Drug use and opioid substitution treatment for prisoners’,Addiction.Stöver, H., and Nelles, J. (2003), ‘10 years of experience with needle and syringe exchange programmes inEuropean prisons: a review of different evaluation studies’,International Journal of Drug Policy,14 (5–6), 437–44.Stöver, H., Hennebel, L. and Casselman, J. (2004),Substitution treatment in European prisons: a study of policiesand practices of substitution treatment in prisons in 18 European countries,Cranstoun Drug Services, London.Stöver, H., Casselman, J. and Hennebel, L. (2006), ‘Substitution treatment in European prisons: a study of policiesand practices in 18 European countries’,International Journal of Prisoner Health2 (1), pp. 3–12.Stöver, H., MacDonald, M. and Atherton, S. (2007),Harm reduction for drug users in European prisons,BIS-Verlag, Oldenburg.Stöver, H., Weilandt, C., Zurhold, H., Hartwig, C. and Thane, K. (2008a),Final report on prevention, treatment,and harm reduction services in prison, on reintegration services on release from prison and methods to monitor/analyse drug use among prisoners (Drug policy and harm reduction, SANCO/2006/C4/02),European Commission,Directorate – General for Health and Consumers. Available at http://ec.europa.eu/health/ph_determinants/life_style/drug/documents/drug_frep1.pdf .Stöver, H., Weilandt, C., Huisman, A., et al. (2008b),Reduction of drug-related crime in prison: the impact ofopioid substitution treatment on the manageability of opioid dependent prisoners,BISDRO, University of Bremen,Bremen.Stöver, H., Lines, R. and Thane, K. (2009), ‘Harm reduction in European prisons: looking for champions and waysto put evidence-based approaches into practice’, in Demetrovics, Z., Fountain, J. and Kraus, L. (eds),Old and newpolicies, theories, research methods and drug users across Europe,European Society for Social Drug Research(ESSD), pp. 34–49. Available at http://www.essd-research.eu/en/publications.html.Sykes, G. M. (1958),The society of captives,Princeton University Press, Princeton, NJ.Taylor, A., Goldberg, D., Emslie, J., et al. (1995), ‘Outbreak of HIV infection in a Scottish prison’,British MedicalJournal310 (6975), pp. 289–92.
401
Harm reduction: evidence, impacts and challenges
Tilson, H., Aramrattana, A., Bozzette, S., et al. (2007),Preventing HIV infection among injecting drug users in highrisk countries: an assessment of the evidence,Institute of Medicine, Washington, DC. Available at http://www.nap.edu/catalog.php?record_id=11731.Todts, S., Fonck, R., Colebunders, R., et al. (1997), ‘Tuberculosis, HIV hepatitis B and risk behaviour in a Belgianprison’,Archives of Public Health55, pp. 87–97.Tonry, M. (2004),Punishment and politics: evidence and emulation in the making of English crime control policy,Willan Publishing, Cullompton.Torres, A. C., Maciel, D., Sousa, D. and Cruz, R. (2009),Drogas e Prisões — Portugal 2007,CIES/ISCTE, Lisbon.Turnbull, P. J. and Webster, R. (1997),Demand reduction activities in the criminal justice system in the EuropeanUnion, Final Report,EMCDDA, Lisbon.UNAIDS (Joint United Nations Programme on HIV/AIDS) (1997),Prisons and AIDS: UNAIDS technical update,UNAIDS Best Practice Collection, United Nations, Geneva.UNODC (United Nations Office on Drugs and Crime) and UNAIDS (2008),Women and HIV in prison settings,United Nations, Geneva/Vienna.UNODC, WHO and UNAIDS (2006),HIV/AIDS prevention, care, treatment and support in prison settings: aframework for an effective national response,United Nations Office on Drugs and Crime, World HealthOrganization and the Joint United Nations Programme on HIV/AIDS, Vienna and New York.van der Gouwe, D., Gallà, M., van Gageldonk, A., et al. (2006),Prevention and reduction of health-related harmassociated with drug dependence: an inventory of policies, evidence and practices in the EU relevant to the implementationof the Council Recommendation of 18 June 2003. Synthesis report,Contract nr. SI2.397049, Trimbos Instituut, Utrecht.Available at http://ec.europa.eu/health/ph_determinants/life_style/drug/documents/drug_report_en.pdf.WHO (World Health Organization) (1993),WHO guidelines on HIV infection and AIDS in prisons,WHO, Geneva.WHO (2005),Effectiveness of drug dependence treatment in preventing HIV among injecting drug users,Evidencefor action technical papers, WHO, Geneva.WHO (2007),Effectiveness of interventions to manage HIV in prisons: needle and syringe programmes and bleachand decontamination strategies,Evidence for action technical papers, WHO, Geneva.WHO (2005),WHO model list of essential medicines, 14th revision (March 2005),WHO, Geneva. Available athttp://www.who.int/medicines/publications/essentialmedicines/en/index.html.WHO Regional Office for Europe (2005),Status paper on prisons, drugs and harm reduction,WHO Office forEurope, Copenhagen.WHO Regional Office for Europe (2007), ‘WHO health in prisons project’,NewsletterDecember, WHO Office forEurope, Copenhagen. Available at http://www.euro.who.int/Document/HIPP/WHO_HIPP-Newsletter-dec07.pdf.WHO, UNAIDS and UNODC (2007),Effectiveness of interventions to manage HIV in prisons: provision of condomsand other measures to decrease sexual transmission,Evidence for action technical papers, World HealthOrganization, Geneva.Williamson, M. (2006),Improving the health and social outcomes of people recently released from prisons in the UK:a perspective from primary care,The Sainsbury Centre for Mental Health, London. Available at http://www.scmh.org.uk/pdfs/scmh_health_care_after_prison.pdf.Zurhold, H., Haasen, C. and Stöver, H. (2005),Female drug users in European prisons: a European study of prisonpolicies, prison drug services and the women’s perspectives,BIS-Verlag, Oldenburg.
402
Chapter 15Variations in problem drug use patterns and theirimplications for harm reductionRichard Hartnoll, Anna Gyarmathy and Tomas Zabransky
AbstractThis chapter describes the diversity of problem drug use patterns across Europe, the differentharms that may arise, and the implications for harm reduction responses. Harm reductiondeveloped in response to concern about heroin injecting in the 1980s in western Europe.Since then, other patterns of problem drug use have increased and the geographical contexthas expanded. While heroin continues to present challenges, the problematic use ofstimulants such as (meth-)amphetamine or cocaine, of other opioids such as home-madeopiates or synthetic opiates, and of multiple drug combinations calls for innovative responses.These responses need to be flexible and based on consensus and cooperation between keyactors, in particular from the health, social and law enforcement sectors.Keywords:problem drug use, Europe, harm reduction, drug use patterns, responses.
IntroductionHistorically, harm reduction has been heroin-focused and driven by concern over the risks ofinjecting. However, patterns of problem drug use vary widely across the European region.Different patterns of use can have different impacts on the burden of drug-related harms. Theaim of this chapter is to highlight this diversity and to discuss the implications for harmreduction priorities and interventions.The chapter does not provide an overview of drug use patterns in Europe but focuses onselected key themes together with illustrative case studies to underline the importance ofinnovative harm reduction responses that are adapted to the particular harms thatdifferent drug use patterns may incur. The emphasis is on health-related harms. Forreasons of space, social harms such as drug-related crime or public order, thoughimportant, are not covered.The Annual reports of the EMCDDA provide information on the broad differences in problemdrug use (1) observed across Europe.• istorically (from the 1970s/1980s) there has been a predominance of heroin in western and Hsouthern European countries compared to amphetamines in northern countries and home-made opiates and/or misuse of medicines in central and eastern Europe (Hartnoll, 2003).(1) Problem drug use is defined by the EMCDDA as ‘injecting drug use or long-duration/regular use of opioids, cocaine and/oramphetamines’. This definition is currently being reviewed in the context of changes in the drug situation in recent years.
405
Harm reduction: evidence, impacts and challenges
• ore recently (1990s to early 2000s) there has been an increase in heroin/opiates in Meastern and central countries compared to stabilisation or some decreases in westernand southern countries; after 2003, there are signs of heroin increasing again.• lso, more recently, there has been a significant increase in cocaine as the predominant Astimulant in south and west Europe compared to amphetamines in northern, central andeastern countries.• here has been a continuing high level of injecting (whether opioids or stimulants) in Tnorthern, central and eastern countries compared to relatively lower levels of injecting,together with increases in smoking or sniffing, in south and west Europe.Some exceptions to this general picture are described later in this chapter. In all countries,multiple drug use, especially of opiates and stimulants, often together with heavy alcohol useor pharmaceuticals such as benzodiazepines, is common amongst problem drug users.Unless otherwise referenced, information on patterns of problem drug use in the EU is basedon the Annual reports of the EMCDDA and national reports from the Reitox network of focalpoints in Member States.
Amphetamine and methamphetamineWhile heroin and more recently cocaine have been the main drugs of concern in many Europeancountries, in parts of northern and central Europe amphetamine use has been important amongproblem drug users for many years, either as a primary drug or in combination with opiates(Sweden, Finland, Norway, Czech Republic). Over recent years, relatively high levels ofamphetamine injecting have also been reported from other countries around the Baltic, as well asfrom Slovakia and Hungary. Some problematic use is reported from other northern and north-western countries, though only the United Kingdom reports a substantial proportion of injectors.The drugs involved are mainly amphetamines (amphetamine sulphate powder, or in some casestablets). Methamphetamine, which is more potent than amphetamine, is not common in EuropeanUnion (EU) countries, with the notable exception of pervitin in the Czech Republic and, quiterecently, Slovakia (EMCDDA, 2008; Griffiths et al., 2008). Reports of smoking crystalmethamphetamine are rare in Europe (in contrast to the United States).In the Czech Republic, methamphetamine has been the primary problem drug since the 1970s(see Case study 15.1). Recently, substantial increases have occurred in neighbouring Slovakia. Inaddition, increased availability and use of methamphetamine is reported from countries whereamphetamine use has traditionally been prevalent (Norway, Sweden, Finland). For example, inNorway methamphetamine has been increasingly found in blood samples from arrested drivers(21 % in 2007 compared to 10 % in 2003) while the trend for amphetamine appears to bedeclining (SIRUS, 2008). Latvia, Lithuania and Hungary also report some increases.Important levels of injecting home-made liquid forms of methamphetamine (‘vint’) ormethcathinone (‘jeff’ or ‘boltushka’) (2), derived from ephedrine or pseudoephedrine, arereported in parts of Russia, Ukraine and other former Soviet Union countries (Grund et al.,(2) Methamphetamine is produced by reduction of (pseudo)ephedrine, while methcathinone is produced by oxidation.The latter is a simpler process though methcathinone is less potent than methamphetamine.
406
Chapter 15: Variations in problem drug use patterns and their implications for harm reduction
2009). The (pseudo)ephedrine is usually extracted from common prescription medicines orover-the-counter cold preparations.Legal restrictions on the sale of ephedrine-containing medicaments have led to thedevelopment of alternative methods of producing stimulant-type drugs. For example, a recentstudy in Odessa, Ukraine describes young drug users injecting home-made drugs containingcathinone, a weaker, shorter-lasting stimulant obtained by mixing freely availablemedications containing phenylpropanolamine with vinegar and potassium permanganate(Chintalova-Dallas et al., 2009). However, Czech customs report seizures of larger shipmentsof pure pseudo/ephedrine thought to originate in Balkan and/or in former Soviet countries.This may signal a renewed interest of criminal groups in the Czech pervitin market followingfailed attempts to control it in the late 1990s and early 2000s (Zabransky, 2009).With some exceptions (e.g. the Czech Republic or Sweden) data on drug users in treatmentfacilities may underestimate the extent of problem use of amphetamines, and of stimulants ingeneral, perhaps because of limited treatment options for amphetamines or because users maynot have, or may not perceive, a need for treatment. For example, in Finland the estimatedprevalence of problem use of amphetamines in 2005 was four times that of opiates. Despite that,opiates were the most common primary drug for which treatment was sought (Stakes, 2008).Risks, harms, protective factorsEvidence on the risks and harms of injecting (meth)amphetamine, relative to heroin or otheropioids, is variable, with different studies showing different results (see also Grund et al.,2010). For example some studies have shown lower HIV prevalence among amphetamineusers, despite high levels of risk behaviour (e.g. Käll and Olin, 1990; Talu et al., 2010), whileothers report similar or higher HIV rates (e.g. Shaboltas et al., 2006; Zeziulin et al., 2008). Itis likely that differences in risk behaviours and rates of infection reflect differences in thepopulations involved, in the contexts of use, and in the forms in which the drugs are preparedand used more than they reflect the specific substance per se. It has also been suggested thatopiate-mediated immuno-suppression increases the likelihood of HIV infection in opioidcompared to amphetamine users (Vallejo et al., 2004).For example, a study of stimulant injectors in Ukraine (Booth et al., 2008) found a lowerprevalence of HIV among stimulant users compared to opiate users in some cities and thereverse in others. Furthermore, despite an overall lower HIV prevalence, stimulant injectorsshowed higher risk scores on composite measures of both injection and sex risk. Sincestimulant injectors were younger with shorter injecting histories, the study concluded thatwithout intervention HIV was likely to increase among stimulant injectors.Studies also suggest that the type of drug injected is associated with different profiles of riskbehaviour. For example Kruse et al. (2009) report that risks specific to stimulant-only users wererelated to direct syringe sharing (sharing needles and rinse water) while risks specific to heroinusers were related to sharing drugs while preparing for injection (front/backloading, sharingcotton and cookers). These differences only became apparent when geographical clustering byneighbourhood was included. The authors suggest that attention to neighbourhood differencesmight improve the impact of interventions for injectors of different drugs.407
Harm reduction: evidence, impacts and challenges
The frequency and intensity of injecting are also important aspects of infection risk (Colfaxand Shoptow, 2005; Braine et al., 2005). For example, in a cohort study of predominantlyheroin injectors in St Petersburg, frequent psychostimulant use was the main factor associatedwith HIV seroconversion (Koslov et al., 2006).In settings where amphetamines are used in small, private groups, or on an intermittent orbinge basis rather than daily, user groups may display lower levels of marginalisation andlower levels of risk behaviours than is often found among heroin using populations (see CaseStudy 15.1). In other populations of amphetamine users, health risks remain high, for examplewhere use is associated with social exclusion, marginalised lifestyles, working in the sexindustry, or imprisonment (March et al., 2006).There is consistent evidence of increased sexual risk behaviour among (meth)amphetamineusers, both injectors (Booth et al., 2008; Molitor et al., 1999; Käll and Nilsonne, 1995; Klee,2006) and non-injectors (Molitor et al., 1998).Overdose deaths appear to be relatively uncommon (EMCDDA, 2009a), in part becauseamphetamines are not central nervous system depressants and the range between effectiveand deadly dose is wider than with opiates. However overdoses can be more difficult tomanage since there is no equivalent to naloxone that might be distributed to street workers orusers — the only option is rapid, sophisticated medical help to deal with the threat of acuteheart failure (personal communication, T. Zabransky).The form of the drug preparation is also important regarding the risk of injection-relatedcomplications. Thus home-based methods of preparing central nervous system stimulantsleave traces of chemicals such as phosphorus, permanganate or sulphuric acid. The additivesmay cause damage to blood vessels and liver (Pavlenko, 2008) or neurological damage and,in the case of permanganate, irreversible Parkinson-like symptoms (de Bie et al., 2007).ImplicationsIf, as appears to be the case in Finland (see above, Stakes, 2008), amphetamine injectors areless likely than their opiate-using counterparts to contact services, then greater emphasis isneeded on outreach and peer education approaches targeted at amphetamine-using networksand groups. This is especially important where the populations involved are young. The highlevels of sexual risk behaviour associated with methamphetamine use mean that sexual riskeducation needs to be addressed systematically in service development and delivery, not only inservices targeting sex workers, and to go beyond providing condoms (Corski and Booth, 2008).The current lack of an equivalent low-cost and effective treatment such as substitution treatmentfor opiate addiction implies that higher priority should be given to developing treatments forstimulant users. Several studies are underway in this regard (Elkashef et al., 2008).In developing responses it may be useful to consider whether distinct approaches or servicesmight encourage stimulant users to seek help. Thus opening hours could take account of moresocially integrated users with regular jobs, or the locations and images projected of services408
Chapter 15: Variations in problem drug use patterns and their implications for harm reduction
could be more discrete in order to overcome barriers such as perceptions that drug servicesare for heroin addicts or ‘junkies’. The distribution of hard gelatine capsules for pervitin usersdescribed in Case study 15.1 is another example of a specific, targeted intervention.At the level of policy, several studies have noted that efforts to suppress home-production ofamphetamine-type stimulants may have paradoxical adverse consequences in terms of usersturning to potentially more risky patterns of drug production and consumption, or in terms ofproduction becoming more professionally organised, leading to an expansion in the market(Grund et al., 2009; Chintalova-Dallas et al., 2009; see also Case study 15.1). This implies aneed for discussions between those responsible for different aspects of drug policy.
Case study 15.1: Methamphetamine (pervitin) injecting in the Czech RepublicIn contrast to other EU countries, the major drug used by problem drug users in the CzechRepublic is crystal methamphetamine, locally known as pervitin (3). The predominance ofpervitin has persisted from the early 1970s to the present.Hard gelatine capsulesQuite recently, a remarkable harm reduction intervention specifically for pervitin users wasintroduced in the Czech Republic and is quickly spreading through the country.Distribution of empty hard gelatine capsules was introduced in 2006 in South Moravia (personalcommunication, B. Janiková). The inspiration for providing capsules was the practice of somemethamphetamine users of swallowing the drug in a bolus, wrapped in paper or a plastic bag,when they were experiencing severe problems with injecting due to injured veins. In English, thisis nicknamed ‘parachuting’ (Hendrickson et al., 2006).According to the only Czech study to date (Škařupová et al., 2009) in 2008 almost 29 000capsules were distributed by at least 17 harm reduction organisations in different parts of thecountry (4). A further 20 facilities plan to introduce capsule distribution shortly. Drug usersusually fill the capsules with pervitin powder before swallowing, though some report usingliquid pervitin (dissolved powder) after failed attempts to inject.The study reports that drug users perceive the effects of ‘piko’ used in this way as comparable inintensity to injecting the same amount of the drug. Administered rectally, the onset is perceived aseven more intense. Oral use in capsule form reduces the intolerably bitter taste of methamphetamineand, compared to intravenous administration, has an exiguous onset of effect. The study identifiedthat in addition to drug users switching to capsules from injecting, other groups were successfullytargeted: sniffers looking for enhanced drug experience, and relatively stable, employed injectingdrug users (IDUs) wishing to reduce injecting at work in order to avoid discovery.
(3) Originally a German label name for industrially produced methamphetamine. Commonly known as ‘piko’ (pronouncedas ‘pee-koh’) in the Czech drug subculture.4( ) This is quite low compared to approximately 4 500 000 needles and hypodermic sets distributed by Czech needleand syringe programmes (NSPs) in the same year, and another 1 500 000 needles and sets sold to drug users bypharmacies in 2007 (Mravčík, et al., 2008).
409
Harm reduction: evidence, impacts and challenges
Overall, providing hard gelatine capsules is perceived as a successful harm reduction intervention,averting risks of injecting (and sniffing) pervitin. However, professionals are concerned thattitration of dosages can be difficult for inexperienced users, and that gastric ulcers may developafter long-term daily oral use of methamphetamine. Further studies are needed.Drug markets and harm reductionMany drug-related harms arise more from the characteristics of drug markets than fromdrug use per se (e.g. MacCoun and Reuter, 2001; Join Together, 2007). A specific aspectof pervitin in the Czech Republic is its mode of production. Most of what is consumed islocally produced and distributed in very small quantities (Mravčík et al., 2008). Theproducers (‘cooks’) use simple tools, freely available industrial chemicals andpseudoephedrine extracted from anti-cough medications that until recently were readilyavailable from pharmacies. Production and subsequent use usually occurs in small groupsof three to eight people who share the logistics of production (5). There is little communicationbetween these groups in terms of drug distribution and, most importantly, in terms of use(Miovský et al., 2007) — an aspect that probably contributes to the very low prevalence ofHIV (<0.01 %) and hepatitis C (HCV (<35 %) among Czech users of pervitin. Finally, theatomised Czech pervitin market is comparatively non-violent since ‘turf fights’ associatedwith criminalised drug distribution are rare, and recruitment of new drug users is low due tothe social seclusion of the ‘squads’.However, this relatively low-harm (‘balanced’ in economic terms) situation could rapidlychange if small production patterns were destroyed — for example by restrictingpseudoephedrine-containing medications to prescription only or by a complete ban (6).Disrupting the ‘balanced’ drug market could well result in increased violence and healthharms (e.g. Goldstein, 1989; Rasmussen et al., 1993; Rasmussen and Benson, 1997). Thetransition from atomised drug production and use into a ‘standard’ pyramidal drug marketwith marketing driven by high monetary profits could have long-term negativeconsequences.Harms resulting from unintended consequences of drug policies — especially legal and lawenforcement interventions — represent an area of harm reduction that needs to be furtherexplored and the room for manoeuvre assessed.The other important issue in terms of reducing the harms of homemade drugs is the productionprocess and quality of the final product. For the Czech ‘cooks’, it is imperative to evaporate thefinal methamphetamine liquid into crystals and to share only the powder between the squad(Grund et al., 2009). From the public health point of view, sharing powder (that is subsequentlydissolved and injected by each individual) is, compared to communal sharing of the liquid,substantially less risky in terms of disseminating blood borne diseases within the group.
(5) Procuring the pseudoephedrine-containing pharmaceuticals and other chemicals, providing the house or apartment forpreparing the drug, sharing the necessary know-how.(6) Both options were recently discussed by the Czech decision makers together with less severe forms of regulation suchas electronic ID registration of buyers of pseudoephedrine products.
410
Chapter 15: Variations in problem drug use patterns and their implications for harm reduction
Cocaine and crackIn western and southern Europe the predominant stimulant is cocaine rather thanamphetamines, though there are large differences in the extent of problematic use, with highrates reported from Italy, Spain, the Netherlands and the United Kingdom. Different sub-groups of problem cocaine users can be distinguished (EMCDDA, 2007).One common pattern among socially integrated groups involves escalating use of cocaine,mainly by snorting, alongside heavy alcohol consumption, cannabis, benzodiazepines and,less commonly, heroin. In other groups, cocaine is more closely associated with heroin use aseither a primary or secondary drug. Cocaine-injecting is mostly reported among heroininjectors (including clients of methadone programmes who were primary heroin injectorsbefore entering treatment). In countries where heroin is mostly smoked rather than injectedthen cocaine is mainly either snorted or smoked. Crack appears to be mostly restricted toareas of some large cities and, as in the United States and Canada, is concentrated amongmore marginalised groups of heroin users, sex workers and certain minorities (Fischer et al.,2006). As shown in Case study 15.2, in the United Kingdom crack use appears to be moreprevalent and widespread than in the rest of Europe, though still concentrated in major cities,especially London (GLADA, 2004) and other large metropolitan centres. While crack isusually smoked, the injection of crack in crack-heroin speedballs has been reported fromseveral cities in the United Kingdom (Rhodes et al., 2007) and in a few cases from Dublin(Connolly et al., 2008).As with amphetamines, cocaine-related problems may be less visible in services, especially indrug treatment, partly because of limited treatment options (no equivalent to methadone orbuprenorphine), partly because of the more socially integrated profile of many primary cocaineusers. This is reflected in long lag-times reported between first cocaine use and first treatmentdemand (9–12 years). Despite this, countries such as Spain, Italy or the Netherlands reportrelatively high numbers of cocaine users entering treatment. In Spain and the Netherlands,cocaine is more prevalent than heroin in treatment demand data (EMCDDA, 2009a). In Spain,the number of cocaine-related incidents seen in hospital emergency departments exceeds thosefor heroin or other drugs (Ministerio de Sanidad y Consumo, 2007).Risks, harms, protective factorsInjecting cocaine, whether as a primary drug or in addition to heroin or methadone,involves more frequent injection than other drugs, including (meth)amphetamine, becauseof cocaine’s shorter duration of action. This high frequency of injecting may carry higherrisks of infections related to injecting (Tyndall et al., 2003; Chaisson et al., 1989; van Beeket al., 1994). The compulsive nature of crack use combined with user profiles also implieshigher-risk use patterns (Edlin et al.; 1994, McCoy et al., 2004; van Beek et al., 2001). Theuse of both powder cocaine and crack is also linked to health risks such as medicalemergencies and cardiovascular problems (Egred and Davis, 2005; Pozner et al., 2005).Smoking crack cocaine involves particular risks and harms, including mouth ulcers and thepotential for transmission of HCV via sharing of crack pipes (Tortu et al., 2004; Fischer et411
Harm reduction: evidence, impacts and challenges
al., 2008; Neaigus et al., 2007). The possibility that crack smoking methods mightconstitute risk factors for HIV infection had been suggested in the mid-1990s (Porter et al.,1994). Crack use is also associated with increased sexual risk behaviours (Booth et al.,2000). Cocaine injecting or crack use can also adversely affect opiate substitutiontreatment outcomes (Williamson et al., 2006).Snorting cocaine, though less risky than injecting in terms of mortality or transmission ofinfectious diseases through sharing paraphernalia, also has risks, including dependence,damage to nasal membranes or escalating financial problems among heavy users (Smith etal., 2002; Grund et al., 2010). Sexual risk behaviours are also relevant. For example, a studycomparing young cocaine users with young heroin users in three Spanish cities found thatcocaine users were less marginalised, reported much lower levels of injecting or borrowingsyringes, and were much less likely to be HIV or HCV positive than heroin users. However,cocaine users reported higher levels of unprotected sex with occasional partners, and higherrates of sniffing through tubes used by more than 10 persons (Brugal et al., 2009).ImplicationsProblem cocaine users may be harder to reach than users of opiates. Socially integratedusers may be slow to acknowledge problems and may not perceive drug services for‘junkies’ as relevant to them. This implies the need for different approaches and messages forsocially integrated users, for example as tried in Italy (Ministerio della Salute, 2007) andIreland. The Irish pilot project suggested that cocaine users’ reluctance to approach heroin-oriented programmes could be reduced through separate access during evenings, orimmediately before and after the weekend (Horgan, 2007). However, the social networksand economic resources of more socially integrated users may also enable them to resolveproblems without contacting services (Cohen and Sas, 1993; Decorte, 2000), though usersdo not consider recovery to be easy (Cunningham, 2000).Highly marginalised heroin/cocaine/crack users may also be reluctant to contact regulartreatment or harm reduction services, or may lead such chaotic lives that services are unable(or unwilling) to attract or retain them in treatment or facilitate reductions in risk behaviour(Prinzleve et al., 2004). This has several implications.Intensive, targeted outreach projects are needed to access and deliver treatment or harmreduction interventions to such populations. Examples are found in the Netherlands andIreland (Henskens et al., 2008; Connolly et al., 2008). The high-frequency injection needs ofcocaine users have important implications for the number and manner of distribution ofsyringes/needles by NSPs, the capacity and opening hours for consumption rooms, and thetype of health education and prevention messages (e.g. regarding syringe re-use). Crack useimplies reviewing needs regarding provision of relevant paraphernalia and information onthe risks associated with using and sharing crack pipes. For example, in several Canadiancities ‘safer crack use kits’ are distributed (Haydon and Fischer, 2005; Boyd et al., 2008;O’Byrne and Holmes, 2008). The distribution of materials for crack or heroin smoking orfreebasing — such as aluminium foil and straws or crack pipes — takes place in low-412
Chapter 15: Variations in problem drug use patterns and their implications for harm reduction
threshold centres in Austria, Belgium, the Czech Republic, France, Luxembourg and Spain(EMCDDA national reports, 2008). An evaluation of the impact of distributing crack-smokingequipment at the needle exchange programme in Ottawa found that not only did infection-related risk behaviours associated with crack smoking diminish, but that there was also a shiftfrom injecting to smoking the drug (Leonard et al., 2008).Cocaine-injecting methadone clients may be seen as a group for whom substitution treatmentis not working effectively (Williamson et al., 2006; Tyndall et al., 2003; Booth et al., 2003;Audit Commission, 2002). This points to the need to reinforce links between treatment, harmreduction sectors and the wider care system (e.g. joint case management of individual cases)and to the need to improve the quality of treatment services. Marginalisation, serious physicaland mental health problems and the acute effects of crack such as paranoia and aggressionimpose special demands on staff and imply specific strategies for training staff as well as forcontacting and delivering services to crack users.
Case study 15.2: The diffusion of crack-based speedball injection in the United KingdomWhereas only 1 % of heroin injectors in London reported crack injecting in 1990, over 50 %regularly did so by 2003, usually as part of a crack-heroin ‘speedball’ (Rhodes et al., 2006).In some metropolitan centres of the United Kingdom, such as Bristol and Manchester, over70 % of injectors regularly inject crack-heroin speedball (Health Protection Agency et al.,2006). Patterns of injection in some United Kingdom cities have changed dramatically overthe last decade. There is an emerging culture of crack-based speedball injection among manyinjectors that is quite distinct from injecting opiates alone, and almost unique to the UnitedKingdom (Rhodes et al., 2007).In the United Kingdom, the odds of having HCV infection are elevated among injectors of crackand crack-based speedball (Hickman et al., 2007). The regular injection of crack-heroinspeedball also appears linked to increased vein damage, including abscesses and bacterialinfections. Qualitative research links such vein damage to ‘missed hits’ related to the localanaesthetic action of crack, the excess use of citric in the preparation of speedball injections,‘flushing’ when making a hit, and the interplay of homelessness and crack injecting (Rhodes etal., 2007). Importantly, various data sources in the United Kingdom link speedball injection withshifts towards groin (femoral vein) injection, articulated by speedball injectors as an ‘acceptablerisk’ and not merely as a ‘last resort’ in the face of increased vein deterioration (Rhodes et al.,2007). Surveys show that almost half (45 %) of injectors in England report groin injecting in thelast month, with crack injectors significantly more likely than opiate-only injectors to inject intotheir femoral vein (Rhodes et al., 2006; Hickman et al., 2007). Groin injection may persistdespite awareness of increased health risks and medical complications. Groin injectors are morelikely to report open wounds at their injection sites and to have had deep vein thrombosis.This emphasises an urgent need to review how harm reduction services respond in relation tovein care. Shifts to crack-based speedball and groin injection highlight a need for interventionsto consider how to promote safer speedball injecting alongside emphasising basic vein careand injecting hygiene. Interventions also need to focus on preventing transitions towardsgroin and crack injection among users of heroin.
413
Harm reduction: evidence, impacts and challenges
Opiates and opioidsOver the past decade or so, heroin injecting appears to have decreased, at least to someextent, in many western European countries, and its use by other routes, notably smoking orchasing (7), has increased. This is especially notable in the Netherlands, Spain and Denmark,and to a lesser extent in some other countries such as Ireland, Portugal, Germany and theUnited Kingdom. Sniffing heroin has increased in countries such as Austria, France andGreece. In some areas, this has led to decreases in demand on needle and syringeprogrammes.However, despite the trend towards smoking or sniffing in some countries, there are largedifferences between countries, and injecting remains the predominant route ofadministration of opiates in most of the newer Member States as well as in some oldermembers such as Finland, Italy and Luxembourg. Even in countries where injecting hasdecreased, important proportions of heroin users still inject and new groups of injectorscontinue to emerge. In France, for example, where injecting had decreased substantially inearlier years, increased injecting has been reported since 2005 among some groups ofyoung people (Cadet-Taïrou et al., 2008; CEIP de Marseille, 2006). In Italy, the estimatedincidence rate of new heroin use has not decreased over this decade and injecting remainsthe most common route of administration despite some increases in heroin smoking (DrugPolicy Department, 2008). This is in marked contrast to Spain, where estimated incidenceof new heroin use has dropped sharply, especially regarding use by injection (Sánchez-Niubò et al., 2009).Although public and professional attention is often focused on recent trends, the legacy ofthe past may impose heavy burdens on current services. In many western Europeancountries, the aftermath of the heroin ‘epidemics’ of the 1980s/90s and the heritage of twodecades of harm reduction can be seen in cumulative populations of ageing addicts,especially in substitution programmes, with increasing needs for care, chronic healthproblems, co-morbidity, unemployment, and service dependency (EMCDDA, 2010b).Heroin is not the only illicit opiate used in Europe. Market conditions sometimes limit orinterrupt the availability of heroin leading to the use of a variety of other opiates or syntheticopioids.Injecting home-produced liquid opiates has been observed in many central and easternEuropean countries since the 1980s (e.g. Poland, the Baltic States, Hungary, CzechRepublic, Slovakia) (Grund, 2005). Since the disintegration of the Soviet Union and theopening up of previously closed economies, drug markets have also changed and heroinhas become the predominant opiate. However, in parts of Russia, Ukraine, Belarus,(7) Technically, smoking and chasing are not the same. Smoking is mixing heroin with, for example, tobacco ormarijuana, or both, and smoking it in cigarettes. Chasing is inhaling the evaporated fumes of heroin from a metal foilthat is heated from underneath. In many studies and sources of data, however, these are not distinguished. In thischapter, the term ‘smoking’ is used in a generic sense to cover both meanings. With smoking, combustion occurs athigh temperatures (about 1 000�C), which destroys many organic substances. With chasing, vaporisation occurs atlower temperatures (about 200�C), resulting in much lower levels of destruction.
414
Chapter 15: Variations in problem drug use patterns and their implications for harm reduction
Moldava and other former Soviet Union countries, as well as in the Baltic States, injectingliquid opiates remain an important component of problem drug use patterns (Grund, 2001;Abdala et al., 2006).Since 1985 there has been a substantial expansion of methadone substitution treatmentacross the EU (Hedrich et al., 2008). This expansion has been accompanied by theemergence of an illicit market in diverted or stolen methadone. This is reflected, for example,in increasing mentions of methadone in fatal overdose cases, often in combination with otherdrugs or alcohol (EMCDDA, 2008). Methadone tablets are also sometimes crushed andinjected.In recent years the use of buprenorphine for substitution treatment has grown as analternative to methadone. Initially implemented on a large scale in France (OFDT, 2003;Canarelli and Coquelin, 2009), other countries have also introduced it, and by 2007buprenorphine accounted for 20 % of substitution treatment in the EU (Hedrich et al., 2008).Alongside this therapeutic use illicit markets have also developed, with the tablets often beingcrushed for snorting or injecting (Roux et al., 2008; Cadet-Taïrou et al., 2008).For example, since 2000 the injection of buprenorphine tablets (which are intended for oraladministration) has become an increasingly important pattern of problem use in Finland(Aalto et al., 2007) and in 2007 was reported as primary drug by a third of clients enteringtreatment (Stakes, 2008). Counselling centres report similar patterns among their clients, withbuprenorphine often used in combination with amphetamines. Buprenorphine is also themost commonly reported substance found in drug-induced deaths (Alho et al., 2007). In bothtreatment and mortality data buprenorphine has almost entirely replaced heroin as the mainproblem opiate. Buprenorphine-naloxone and buprenorpine alone account for over half ofthe substitution treatment provided in Croatia, Cyprus, Finland, France, Latvia and Sweden(EMCDDA, 2009d).Combined buprenorphine-naloxone tablets were introduced in 2006 in an attempt to reducethe risks of misuse, particularly by injection, and increased controls on prescribing wereimposed in countries such as France. Despite this, buprenorphine remains available on theillicit market in many countries through diversion, theft from pharmacies or importation.Apart from Finland and France, these include the Czech Republic (Mravčík et al., 2008),Sweden (Hakansson et al., 2007) and Georgia (Otiashvili et al., 2009).The illicit use of fentanyl (8), as well as overdose deaths, has been reported in parts of theUnited States since the 1980s (Henderson, 1988). Since 2002, following a heroinshortage, fentanyl powder, marketed as ‘China White’ or ‘White Persian’, has become themost widely used drug along with amphetamine among injecting drug users in Estonia(Talu et al., 2008). Some availability and use of fentanyl has also been reported fromFinland, Lithuania and Sweden (EMCDDA, 2008) as well as from Russia and Belarus(Lelevich et al., 2008).(8) Fentanyl is a potent synthetic opioid widely used in surgery for anaesthesia and analgesia, and sometimes to managechronic pain. In medical use it is administered via injection, transdermal patch or as a lozenge.
415
Harm reduction: evidence, impacts and challenges
Risks, harms, protective factorsThe different patterns of opiate use outlined above affect the balance of risks and harms.Relative to injecting, smoking (or sniffing) heroin carries lower risks in terms of injection-related damage, transmission of infections and overdose, though health risks remainincluding, of course, dependence. However, new groups of users and injectors noted abovemay emerge among populations who have not been exposed to harm reduction messagesand interventions like the previous generation, putting them at higher risk of harms such asHIV/HCV or overdose.Regarding chronic heroin users, there is a risk that the scenario of growing populations ofinstitutionalised users with a low quality of life will be repeated in countries currentlyexpanding substitution programmes. This may reflect a diminished (political) priority for oldheroin users who become seen as less ‘attractive’.The injecting of home-produced opiates, which are found largely in countries bordering theEU, brings its own risks, as described in Case study 15.3.
Case study 15.3: Health risks of drugs purchased in liquid vs. solid formIn most of western and central Europe, drugs that are injected are purchased almostexclusively in powder form, whereas in most of the Baltic States, while drugs in powderform are also available for street purchase, a large proportion of IDUs inject home-madeopiates purchased in liquid form (EMCDDA, 2008). The types of drugs injected by injectingdrug users have several implications for harm reduction. Issues of concern are syringe typeand related infection probability, drug injecting hygiene, and sharing of other injectingequipment.Different types of syringes may be used for injecting different types of drugs. Drugs purchasedin powder form (such as heroin) are most often injected using one-piece syringes, while drugspurchased in liquid form (such as ‘shirka’ or ‘kompot’ ) are nearly always injected using two-piece syringes (Gyarmathy et al., 2009b). The one-piece syringe, also called the low dead-space syringe, has minimal dead space between the needle and the depressed plunger, andhas a very small, thin needle (Grund and Stern, 1991; Zule et al., 1997; Zule et al., 2002;Zule and Bobashev, 2009; Gyarmathy et al., 2009b). The two-piece syringe, also called thehigh dead-space syringe, has a detachable needle, and the syringe is attached to a hollowhub at the end of the needle. When the plunger of a two-piece syringe is completelydepressed, there is still considerable space between the syringe and the needle. Two-piecesyringes have larger, thicker needles. The larger space in the two-piece syringe enables it tohold more blood than the one-piece syringe, and studies have shown that those IDUs thatinject with two-piece syringes are more likely to be infected with HIV (Zule et al., 1997; Zuleet al., 2002; Zule and Bobashev, 2009), and possibly with HCV (Gyarmathy et al., 2009b).In addition, there is an indication that thorough cleaning of one-piece syringes may reducethe probability of HCV infection in low HCV-prevalence populations where syringe sharing isuncommon (Gyarmathy et al., 2009b), although this association has yet to be confirmed in
416
Chapter 15: Variations in problem drug use patterns and their implications for harm reduction
longitudinal studies. The harm reduction implication of this is that in countries where drugusers inject (almost) exclusively drugs purchased in powder form, syringe exchangeprogrammes should offer only one-piece syringes, and in countries where both liquid andpowder drugs are available for street purchase, syringe exchange programmes should offerboth types of syringes. Providing drug users who inject drugs purchased in powder form withone-piece instead of two-piece syringes will have implications of reduced HIV and possiblyHCV infection prevalence on the population level.Infection prevalence is not the only harm reduction implication of one- and two-piecesyringes and drugs purchased in powder vs. liquid form. Another aspect is drug injectinghygiene and infections related to lack of hygiene. As two-piece syringes have largerneedles than one-piece syringes, injecting wounds caused by them are also larger. Thismay lead to more infections and abscesses among IDUs who use two-piece syringes.Furthermore, injecting liquid drugs usually involves purchasing the drugs in a large syringeand sharing the content of the large syringe with other drug injectors by means of syringe-mediated drug sharing (Jose et al., 1993; Grund et al., 1996). Drug users cannot be surewhether the syringes that they purchased that were pre-loaded with the liquid drug, or theother syringes used for syringe mediated drug sharing, are sterile or not. This constitutes arisk of drug-related infections for all drug users injecting the liquid drug. Furthermore, asdrugs sold in liquid form are produced and sold under very unhygienic circumstances (J.Kulsiene, personal communication), there is a heightened risk of infections related tohygiene, such as, for example, hepatitis A (Perevoscikovs et al., 2009; O’Donovan et al.,2001). Lastly, the reason why injectors of drugs purchased in liquid form use two-piecesyringes is that these liquid drugs have a lot of floating larger particles (J. Kulsiene, personalcommunication), and the thin needles of one-piece syringes get clogged with the particles.The combination of larger puncture wounds by two-piece syringes, unhygienic drugpreparation and distribution practices, and large floating particles in the drugs may explainthe larger sized and more common abscesses, skin lesions and skin infections among IDUsin Baltic countries compared to IDUs in western and central European countries (V. A.Gyarmathy, unpublished ethnographic findings). Harm reduction efforts in countries wheredrugs are sold in liquid form should also address injecting hygiene, provide filters andteach IDUs how to use and dispose of them properly, and teach users how to treat abscessesand infected injecting wounds.Sharing injecting equipment other than syringes (e.g. filters and cookers) may also be associatedwith infection with drug-related infectious diseases (Hagan et al., 2001). In populations with lowHCV and HIV prevalence where mostly sterile syringes are used by IDUs, no such associationwas found (Gyarmathy et al., 2009a). When two-piece syringes are used to inject liquid drugsin populations where syringes are often re-used, sharing other injecting equipment may also bea source of infection risk. Harm reduction efforts in such populations may include promoting theuse of non-injectable sterile syringes for drug distribution.
Crushing and injecting buprenorphine tablets is linked to higher health risks than heroin interms of vein and tissue damage, endocarditis and limb amputations, since it is difficult togrind the tablets finely enough (Mravčík et al., 2007; Partanen et al., 2009). Similar risks mayarise from injecting other pharmaceutical products intended for oral administration, such ascrushed methadone tablets.417
Harm reduction: evidence, impacts and challenges
The risks arising from the high potency and rapid onset of action of fentanyl is reflected inmortality data, with 117 fatal fentanyl overdoses reported in Estonia in 2005–06(Ojanperä et al., 2008). Furthermore, fentanyl injectors reported higher-risk behavioursand were three times more likely to be HIV positive compared to amphetamine injectors(Talu et al., 2010).ImplicationsThe increase in the smoking of heroin may imply a greater need for facilities for heroinsmokers at drug consumption rooms and for interventions that may discourage smokers fromstarting to inject (Hedrich et al., 2010). It has also prompted interventions to encourageinjectors to reduce risks by switching to smoking. For example, a study at four needle andsyringe programmes in the United Kingdom suggested that distributing foil packs toattendees can be a useful means of engaging clients in discussions of ways to reduceinjecting risks and can reduce injecting in settings where there is a pre-established culture ofheroin chasing (Pizzey and Hunt, 2008).For countries with existing populations of older, long-term users, there is the need for moredignified options and ‘normalised’ conditions for living, in line with efforts to improve qualityof life for elderly or handicapped elderly people in general (e.g. protected housing), ordiscussions on the changing role of drug consumption rooms in Switzerland(Sozialdepartement der Stadt Zürich, 2008).For countries dealing with more recent ‘epidemics’ it would be valuable to anticipate thelonger-term consequences of implementing harm reduction programmes that are concernedwith keeping people alive and reducing infectious diseases and other harms now. This mightinclude emphasising the importance of linking programmes to social reintegration options,education, training or work schemes in order to reduce the number of long-term‘institutionalised’ users in the future.The injection of synthetic opioids such as buprenorphine or methadone raises a general issueabout the formulation of drugs used in substitution treatment (the composition of tablets,syrup, gel, etc.) and how to reduce the likelihood of them being injected, or at the very leasthow to reduce the risks if they are injected. For example, in the Czech Republic increasingnumber of doctors are asking for injectable buprenorphine, which they believe is better thaninjectable methadone because of a much lower risk of overdose, but at the same time theywant to prevent disorders arising from particles that corrode the endothelium in blood vesselsand heart (T. Zabransky, personal communication).Heroin prescription therapy, which has existed in the United Kingdom since the earlytwentieth century (Bean, 1974), is becoming increasingly accepted in several Europeancountries following clinical trials in different countries (EMCDDA, 2009c). For example, inrecent years it has become an established treatment programme in Germany, theNetherlands and Switzerland. In clinical trials, heroin prescription has been shown to behighly effective among IDUs who are resistant to other forms of treatment, such as418
Chapter 15: Variations in problem drug use patterns and their implications for harm reduction
methadone. Not only are there higher rates of treatment retention among heroin patientsthan among methadone clients, but they also have higher proportions of improved mentalhealth, decreased use of illicit drugs, and reductions in criminality (Frick et al., 2006; Drucker,2001; Rehm et al., 2001; Hartnoll et al., 1980).
Discussion: cross-cutting issuesMultiple drug useAmong problem drug users multiple drug use is the norm. While users may have a preferredor primary drug, ‘pure’ users of only one type of drug are relatively uncommon. Separatingusers into categories such as amphetamine-type stimulants, cocaine, opiates, is thussomewhat artificial. Common combinations include stimulant and opiate (e.g. ‘speedball’ —cocaine and heroin, ‘Czech speedball’ — methamphetamine and buprenorphine) orstimulant and sedative (cocaine and alcohol and benzodiazepines). Injection drug use raisesparticular concerns whatever drugs are involved. Some combinations are especiallyassociated with elevated health risks, for example opiate and alcohol (overdose) or heroinand cocaine injecting (infectious diseases) (Best et al., 2000). Other patterns of problem druguse (not covered in this chapter) that are reported by some treatment centres and counsellingservices for young people include heavy use of various combinations of cannabis, ecstasy,amphetamines, alcohol and benzodiazepines.While those working in drug services are aware that problem drug use often involvesmultiple substances, it is possible that this is not fully appreciated by policymakers, the mediaor the public who tend to focus on ‘the drug of the moment’, with the implicit accompanyingassumption that previous drug use patterns are now less important. The diversity of multipledrug use patterns, including the role of legal drugs such as benzodiazepines and alcohol,reinforces the importance of ongoing information exchange between researchers,practitioners and the political level.Individual and public health harmsAs noted at the beginning of this chapter, harm reduction evolved as a reaction to harmsarising from heroin injecting. The substantial expansion of harm reduction policies andresponses observed in the EU since the mid-1980s, especially substitution treatment andneedle and syringe programmes, has been a major pillar of policies to reduce riskbehaviours and contain serious harms such as HIV infection and overdose deaths. At the endof the 2000s, where do harm reduction responses stand in relation to the diversity ofproblem drug use patterns described in this chapter?The incidence of new cases of HIV among injecting drug users is low or declining in manycountries, but still relatively high in some countries including Portugal, Estonia and Latvia, andvery high in Russia and Ukraine. In central European countries HIV prevalence remains lowor relatively low, despite high levels in some neighbouring countries. However, some as yetsmall increases in incidence are observed in a few countries (e.g. Bulgaria, Sweden), and419
Harm reduction: evidence, impacts and challenges
ongoing transmission among young injectors is reported in several localities, for example inFrance, Spain, Estonia, Lithuania and Poland. Risk behaviours too, though reduced, are stillreported from many countries (EMCDDA, 2009a).HCV prevalence among IDUs is high or relatively high in many European countries, even insome with low HIV levels. High rates of infection found among samples of new IDUs inseveral countries suggest that incidence also continues at significant levels (EMCDDA, 2010).Tuberculosis (including drug-resistant strains) is re-emerging as a potentially serious healththreat (Deiss et al., 2009).Drug overdose deaths in the EU as a whole decreased somewhat from a peak around 2000,though recent years show some increases (Vicente et al., 2008). However, trends, both long-term and short-term vary considerably between countries (EMCDDA, 2008).That acute drug deaths have not continued to decrease overall in the EU might be thoughtpuzzling in view of the trend of reduced injecting in many countries, and the introduction orexpansion of substitution treatment and other harm reduction measures. Possible reasons include:• he capacity and coverage of treatment and harm reduction services, including Tsubstitution treatment, have not yet reached a threshold in enough countries to maintain anobservable impact (in terms of continued decreases) at population level.• he high risk of overdose after release from prison (Seaman et al., 1998; Farrell and TMarsden, 2008) or at the end of treatment (Davoli et al., 2007), which together couldaccount for 15–25 % of all acute drug-related deaths, has not been adequately addressed.• ncreases in the use of high-risk drug combinations have counteracted the positive impact Iof other changes.• geing and health deterioration of long-term users may increase the risk that opiate Aoverdoses are fatal (Darke et al., 2006).• ncreased availability of heroin reflects increasing opium production in Afghanistan I(following shortages in 2001–03) and has contributed to renewed rises in heroin use andmore deaths.It is also possible that without increased levels of substitution treatment and otherinterventions, overdose deaths would have been higher.Apart from overdoses, other drug-related deaths continue to occur, for example among olderusers due to multiple morbidity, HCV and alcohol liver damage (McDonald et al., 2009). Anincreasing number of deaths due to AIDS among IDUs are reported from a few countries, forexample Latvia and Estonia where a high proportion of IDUs are unaware of their HIV status,raising questions about policies regarding access to both testing and treatment (Abel-Ollo etal., 2009).Thus, despite some success in containing and reducing individual and public health harms,harm reduction responses face a variety of challenges in terms of continuing risk behavioursand changing drug use patterns.420
Chapter 15: Variations in problem drug use patterns and their implications for harm reduction
New drug injecting populations and local increases in HIV incidence underline the importanceof continuing preventive and educational measures regarding HIV. In some newer MemberStates and countries bordering the EU this remains a major public health challenge.It is recognised that HIV preventive measures are not adequate for HCV and that additionalefforts are required. Examples given in this chapter reinforce the conclusion that not all riskbehaviours regarding sharing of injecting equipment or other paraphernalia are dealt withadequately, for example specific practices such as syringe mediated drug sharing (Grund etal., 1996), syringe types (Gyarmathya et al., 2009a; Zule and Bobashev, 2009) straws orcrack pipes (Haydon and Fischer, 2005).Other health measures to reduce harms associated with infectious diseases include hepatitisB vaccination, hepatitis C treatment, and TB prevention (especially in high-risk environments,e.g. prisons).Regarding deaths, a range of measures has been used in various countries, including pre-release counselling for prisoners, overdose prevention education for drug injectors or take-home naloxone (Strang et al, 2008; EMCDDA, 2009b). With all these measures, as withthose seeking to prevent HIV/HCV, coverage of the relevant high-risk populations is critical,as is the need for evidence on the effectiveness of possible interventions.Health harms such as vein and other tissue damage associated with injecting crushed tabletsor home-made drugs, groin injection of crack/heroin, or smoking of crack in home-mademetal pipes point to the continuing importance of delivering health and hygiene education indifficult contexts to often-marginalised populations.Mental health harms associated with problem drug use present a further challenge to harmreduction responses in the future. It is well established that there is extensive psychiatric co-morbidity among clients with diagnoses of drug dependency (EMCDDA, 2004). Harmreduction interventions have tended to focus on somatic health harms such as infectiousdiseases, but are increasingly confronted by mental health and behavioural disturbances, insome contexts including violence, accentuated by heavy stimulant use. Prisons are anothersetting where mental health and drug use problems are especially severe (e.g. Hannon et al.,2000). It is unrealistic to expect frontline services to offer more than prophylactic assistanceregarding drug-related harms to clients with serious mental health problems. It makes moresense to establish links and procedures such as joint case management with specialisedmental health services.Injecting and transitions to or from other routesThe majority of serious drug-related health harms arise from injecting. The shift towards otherroutes of administration observed in some countries is not incompatible with continuing levelsof high risk. Many factors affect the preferred route of administration, for example the formand purity of a drug on the market (Bravo et al., 2003), or cultural attitudes and taboosabout injecting. These can change.421
Harm reduction: evidence, impacts and challenges
The implications are that it is important to avoid complacency because trends suggestdecreasing injecting. It does not mean that current, younger non-injectors will not inject in thefuture. Prevention of transitions to injecting, and encouragement of transitions to other routesamong injectors should be a priority for those unwilling or unable to cease drug use altogether.Several examples of interventions to encourage transitions from injecting to less harmfulroutes of administration have been noted in this chapter, including the distribution of foilpacks for heroin chasing, safer crack use kits for crack cocaine smoking, and hard gelatinecapsules for oral or rectal use of pervitin. In all of these examples, non-injecting drug userswere also attracted to the services, suggesting possibilities for an expanded role forinterventions such as needle and syringe programmes. The design and development of harmreduction interventions would benefit from the inclusion of qualitative/anthropologicalmethods that take account of the perspectives of users themselves.Geography, persistence and changeGeographical differences and changes in drug use reflect many dimensions: long-standinghistorical and cultural patterns; recent developments in politics, economy and youth cultures;drug markets and trafficking routes; drug policies, enforcement policies, prescribing policies.Changes can be rapid, for example the emergence of the use of fentanyl in Estonia followingreduced opium production in Afghanistan and a subsequent heroin shortage in the early2000s. However, the specific nature of such changes is hard to predict, for example the sameshortage of heroin appears to have been associated with increased injection of buprenorphinetablets in nearby Finland. In other situations, for example in Australia, a heroin shortage wasassociated with increases in benzodiazepine use and injection of stimulants (cocaine in NewSouth Wales where a cocaine market already existed, methamphetamine in other states) (Toppet al., 2003; Degenhardt et al., 2005). In the Australian example, heroin injection diminished,especially among younger users, and fatal and non-fatal heroin overdoses decreased bybetween 40–85 %, but incidents of psychosis and violence attributed to stimulant use increased,as did requests for treatment of stimulant-related problems (Degenhardt et al., 2004). It is alsohard to anticipate where rapid change will occur, or not. Thus explosive HIV epidemics havebeen observed over the last decade in the Baltic States (Uusküla et al., 2008), Russia and otherformer Soviet Union countries (Rhodes et al., 2002; Grund, 2001), but not in other areas ofcentral Europe, despite high levels of risk behaviour among injectors.Diffusion to neighbouring areas can also occur. For example, since 2000 the use of pervitin(methamphetamine) spread from the Czech Republic to Slovakia, but otherwise evidence of thediffusion of pervitin is more limited. Some pervitin is reported in border areas in Germany(Pfeiffer-Gerschel et al., 2008), among some sub-populations in Hungary (Griffiths et al., 2008)and Austria (VWS, 2008). An increase in methamphetamine in Nordic and Baltic countriesappears to be associated with trafficking from Lithuania, not with export from Slovakia or theCzech Republic (EMCDDA–Europol, 2009). The increase in imported heroin observed in manynewer Member States could be seen as a logical concomitant of EU membership and theharmonisation of markets in general, of which the drug market is a special case.422
Chapter 15: Variations in problem drug use patterns and their implications for harm reduction
At the same time there is also continuity in differences, for example methamphetamine in theCzech Republic and amphetamine in Nordic countries. The predominance of cocaine as themain stimulant in southern and western Europe compared to amphetamines in northern andcentral Europe is another example. Sustained differences are also found within countries oreven within cities (personal experience of author).While it is feasible to monitor long-term trends through instruments such as those used by theEMCDDA, it is more difficult to identify rapidly emerging problems in time to reactappropriately. The French TREND scheme provides one model (OFDT, 2007). Ethnographicand quantitative data are collected through a network of local co-ordination groups in sevencities, focusing on population groups with high drug use prevalence.Contexts: implications for harm reductionMany of the studies cited in this monograph make clear that problem drug use and drug-related harms are often closely associated with social dislocation and social exclusion and withfactors such as unemployment, unstable living conditions, minority status, imprisonment, sexwork, migration. Social exclusion and stigma are key contextual factors that exert a powerfulinfluence on patterns of problem drug use and often hinder attempts to implement effectiveharm reduction measures. Attitudes towards human rights and problem drug users are a keyelement influencing how far harm reduction policies can be implemented. It is possible that thissituation is further exacerbated by recession and economic crisis. A further dimension relatedto implementation of harm reduction policies concerns the importance of understanding thecontexts, priorities and needs of problem drug users themselves when designing interventions.It may be difficult for those working at the local level in specific areas of drug policy or serviceprovision to change the broader structural context referred to above. However, it may be morefeasible to influence local situational factors and risk environments. Studies focusing on micro-environmental factors are starting to provide insight into how local injecting environments andrisk behaviours can be highly sensitive to public health, law enforcement and policing policies(Rhodes, 2002). In particular, policing practices can have a considerable effect on injectingbehaviours and health harms at both individual and group level as well as a detrimentalimpact on the coverage and effectiveness of interventions such as needle exchange (Maher andDixon, 1999; Wood et al., 2002). For example, Rhodes and colleagues report that policepractices in Russia can encourage a fear of arrest, fine or detention among drug users thatleads to reluctance to carry needles and syringes and in turn to paraphernalia sharing atpoints of drug sale (Rhodes et al., 2003). The implications of these studies point clearly to theimportance of including law enforcement agencies in local harm reduction policies.
ConclusionThe specific implications of the variety of drug use patterns and health harms described inthis chapter depend on local circumstances, but the broader message, especially topolicymakers and service managers, is that changing conditions on the illicit market as wellas the form and conditions in which substitute drugs are prescribed can have considerable423
Harm reduction: evidence, impacts and challenges
impacts on local drug use patterns. Similarly, the balance within drug policies, especially interms of policing approaches vis-à-vis treatment and harm reduction responses, caninfluence the risk environments in which drug use occurs. Local responses thus not onlyneed to be flexible and adjust to changing needs, but also need to be based on consensusand cooperation between key actors. The rate at which risky drug use patterns can changesuggests that brief rapid needs assessments and monitoring is needed to target informationand health education at new user groups, and to identify new drug use patterns, risks andrisk situations.
ReferencesFor EMCDDA annual reports and other publications, see www.emcdda.europa.eu. For national reports to theEMCDDA, see www.emcdda.europa.eu/publications/national-reports.Aalto, M., Halme, J., Visapaa, J. P., and Salaspuro, M. (2007), ‘Buprenorphine misuse in Finland’,Substance Useand Misuse42, pp. 1027–8.Abdala, N., Grund, J-P., Tolstov, Y., Kozlov, A. and Heimer, R. (2006), ‘Can home-made injectable opiatescontribute to the HIV epidemic among injection drug users in the countries of the former Soviet Union?’,Addiction101, pp. 731–7.Abel-Ollo, K., Rahu, M., Rajaleid, K., et al. (2009), ‘Knowledge of HIV serostatus and risk behaviour amonginjecting drug users in Estonia’,AIDS Care,21, pp. 851–7.Alho, H., Sinclair, D., Vuori, E. and Holopainen, A. (2007), ‘Abuse liability of buprenorphine-naloxone tablets inuntreated IV drug users’,Drug and Alcohol Dependence88, pp. 75–8.Audit Commission (2002),Changing habits: the commissioning and management of community drug treatmentservices for adults,Audit Commission, London.Bean, P. (1974),The social control of drugs,Martin Robertson, London.Best, D., Man, L-H., Zador, D., et al. (2000), ‘Overdosing on opiates. Part I: causes’,Drug and Alcohol Findings,4,pp. 4–21.Booth, R., Kwiatkowski, C. and Chitwood, D. (2000), ‘Sex-related HIV risk behaviors: differential risks amonginjection drug users, crack smokers, and injection drug users who smoke crack’,Drug and Alcohol Dependence58, pp. 219–26.Booth, R., Corsi, K. and Mikulich, S. (2003), ‘Improving entry to methadone maintenance among out-of-treatmentinjection drug users’,Journal of Substance Abuse Treatment24, pp. 305–11.Booth, R., Lehman, W., Kwiatowski, C., et al. (2008), ‘Stimulant injectors in Ukraine: the next wave of theepidemic’,AIDS and Behaviour12, pp. 652–61.Boyd, S., Johnson, J. and Moffat, B. (2008), ‘Opportunities to learn and barriers to change: crack cocaine use inthe Downtown Eastside of Vancouver’,Harm Reduction Journal5, p. 34.Braine, N., Des Jarlais, D., Gikdbkattm C., et al. (2005), ‘HIV risk behaviour among amphetamine injectors at USsyringe exchange programs’,AIDS Education and Prevention17, pp. 515–24.Bravo, M., Barrio, G., de la Fuente, L., et al. (2003), ‘Reasons for selecting an initial route of heroinadministration and for subsequent transitions during a severe HIV epidemic’,Addiction98, pp. 749–60.
424
Chapter 15: Variations in problem drug use patterns and their implications for harm reduction
Brugal, T., Pulido, J., Toro, C., et al. (2009), ‘Injecting, sexual risk behaviours and HIV infection in young cocaineand heroin users in Spain’,European Addiction Research15, pp. 171–8.Cadet-Taïrou, A., Gandilhon, M., Toufik, A. and Evrard, I. (2008), ‘Eighth national report from the TRENDsystem’,Tendances58, OFDT, Paris.Canarelli, T. and Coquelin, A. (2009), ‘Données récentes relatives aux traitements de substitution aux opiacés’,Tendances65, OFDT, Paris.Carrieri, M., Amass, L., Lucas, G., et al. (2006), ‘Buprenorphine use: the international experience’,ClinicalInfectious Diseases43, pp. S197–S215.CEIP (Centre d’évaluation et d’information sur la phamacodépendance) de Marseille (2006),OPPIDUM, résultatsde l’enquête 17 (octobre 2005),AFSSAPS, Saint-Denis.Chaisson, R., Bachetti, P., Osmond, D., et al. (1989), ‘Cocaine use and HIV infection in IDUs in San Francisco’,Journal of the American Medical Association261, pp. 652–61.Chintalova-Dallas, R., Case, P., Kitsenko, N. and Lazzarini, Z. (2009), ‘A home-made amphetamine-type stimulantand HIV risk in Odessa, Ukraine’,International Journal of Drug Policy20, pp. 347–51.Cohen, P. and Sas, A. (1993),Ten years of cocaine: a follow-up study of 64 cocaine users in Amsterdam,Department of Human Geography, University of Amsterdam, Amsterdam. Available at www.cedro-uva.org/lib/cohen.ten.pdf.Colfax, G. and Shoptow, S. (2005), ‘The methamphetamine epidemic: implications for HIV prevention andtreatment’,Current HIV/AIDS Reports2, pp. 194–9.Connolly, J., Foran, S., Donovan, A., Carew, A. and Long, J. (2008),Crack cocaine in the Dublin region: anevidence base for a Dublin crack cocaine strategy,HRB Research Series 6, Health Research Board, Dublin.Available at http://www.hrb.ie/uploads/tx_hrbpublications/HRB_Research_Series_6.pdf.Corski, K. and Booth, R. (2008), ‘HIV sex risk behaviours among heterosexual methamphetamine users: literaturereview from 2000 to present’,Current Drug Abuse Reviews1, pp. 292–6.Cunningham, J. (2000), ‘Remissions from drug dependence: is treatment a prerequisite?’,Drug and AlcoholDependence,59, pp. 211–13.Darke, S., Degenhardt, L. and Mattick, R. (2006),Mortality amongst illicit drug users: epidemiology, causes andintervention,Cambridge University Press, Cambridge.Davoli, M., Bargagli, A., Perucci, C., et al. (2007), ‘Risk of fatal overdose during and after specialised drugtreatment: the VEdeTTE study, a national multi-site prospective cohort study’,Addiction102, pp. 1954–9.de Bie, R., Gladstone, R., Strafella, A., Ko, J. and Lang, A. (2007), ‘Manganese-induced Parkinsonism associatedwith methcathinone (ephedrone) abuse’,Archives of Neurology,64, pp. 886–9.Decorte, T. (2000),The taming of cocaine: cocaine use in European and American cities,VUB University Press,Brussels.Degenhardt, L., Day, C. and Hall, W. (eds) (2004),The causes, course and consequences of the heroin shortage inAustralia,NDLERF Monograph 3, National Drug Law Enforcement Research Fund, Commonwealth of Australia.Available at http://www.ndlerf.gov.au/pub/Monograph_03.pdf.Degenhardt, L., Day, C., Dieze, P., et al. (2005), ‘Effects of a sustained heroin shortage in three Australian States’,Addiction,100, pp. 908–20.
425
Harm reduction: evidence, impacts and challenges
Deiss, R., Rodwell, T. and Garfein, R. (2009), ‘Tuberculosis and illicit drug use: review and update’,ClinicalInfectious Diseases48, pp. 72–82.Drucker, E. (2001), ‘Injectable heroin substitution treatment for opioid dependency’,Lancet27 October, 358, p.1385.Drug Policy Department (2008),2008 national report to the EMCDDA on the drug situation in Italy,Presidency ofthe Council of Ministers, Rome.Edlin, B., Irwin, K., Faruque, S., et al. (1994), ‘Intersecting epidemics: crack cocaine use and HIV infection amonginner-city young adults’,New England Journal of Medicine331, pp. 1422–7.Egred, M. and Davis, G. (2005), ‘Cocaine and the heart’,Postgraduate Medical Journal81, pp. 568–71.Elkashef, A., Vocci, F., Hanson, G., et al. (2008), ‘Pharmacotherapy of methamphetamine addiction: an update’,Substance Abuse29, pp. 31–49. See also EMCDDA Annual Report 2009.EMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2004),Co-morbidity,Selected issue,European Monitoring Centre for Drugs and Drug Addiction, Lisbon.EMCDDA (2007),Cocaine and crack cocaine: a growing public health issue,Selected issue, European MonitoringCentre for Drugs and Drug Addiction, Lisbon.EMCDDA (2008),Annual Report 2008: the state of the drugs problem in Europe,European Monitoring Centre forDrugs and Drug Addiction, Lisbon.EMCDDA (2009a),Annual report 2009: the state of the drugs problem in Europe,European Monitoring Centre forDrugs and Drug Addiction, Lisbon.EMCDDA (2009b), Tables HSR-7 and HSR-8, Statistical bulletin. Available at http://www.emcdda.europa.eu/stats09/hsrtab7 and http://www.emcdda.europa.eu/stats09/hsrtab8.EMCDDA (2009c), Table HSR-1, Statistical bulletin. Available at http://www.emcdda.europa.eu/stats09/hsrtab1.EMCDDA (2009d), Table HSR-3, part ii, Statistical bulletin, Available at http://www.emcdda.europa.eu/stats09/hsrtab3b.EMCDDA (2010a),Trends in injecting drug use in Europe,Selected issue, European Monitoring Centre for Drugsand Drug Addiction, Lisbon.EMCDDA (2010b),Ageing drug users,Selected issue, Publications Office of the European Union, Luxembourg,forthcoming.EMCDDA–Europol (2009),Methamphetamine: a European Union perspective in the global context,EMCDDA–Europol joint publications 1, Office for Official Publications of the European Communities, Luxembourg.Farrell, M. and Marsden, J. (2008), ‘Acute risk of drug-related death among newly released prisoners in Englandand Wales’,Addiction103, pp. 256–7.Fischer, B., Rehm, J., Patra, J., et al. (2006), ‘Crack across Canada: comparing crack users and crack non-users ina Canadian multi-city cohort of illicit opioid users’,Addiction101, pp. 1760–70.Fischer, B., Powis, J., Cruz, M., Rudzinski, K. and Rehm, J. (2008), ‘Hepatitis C virus transmission among oralcrack users: viral detection on crack paraphernalia’,European Journal of Gastroenterology and Hepatology20,pp. 29–32.Frick, U., Rehm, J., Kovacic, S., Ammann, J. and Uchtenhagen, A. (2006), ‘A prospective cohort study on orallyadministered heroin substitution for severely addicted opioid users’,Addiction101, pp. 1631–9.
426
Chapter 15: Variations in problem drug use patterns and their implications for harm reduction
GLADA (Greater London Alcohol and Drug Alliance) (2004),An evidence base for the London crack cocainestrategy,Greater London Authority, London.Goldstein, P. (1989), ‘Drugs and violent crimes’, in Weiner, N. and Wolfgang, M. (eds),Pathways to criminalviolence,Sage Publications, Newbury Park, CA.Griffiths, P., Mravcik, V., Lopez, D. and Klempova, D. (2008), ‘Quite a lot of smoke but very limited fire: the use ofmethamphetamine in Europe’,Drug and Alcohol Review27, pp. 236–42.Grund, J-P. (2001), ‘A candle lit from both sides: the epidemic of HIV infection in central and eastern Europe’, inMcElrath, K. (ed.),HIV and AIDS: a global view,Greenwood Press, Wesport, Ct.Grund, J-P. (2005), ‘The eye of the needle: an ethno-epidemiological analysis of injecting drug use’, in Pates, R.,McBride, A. and Arnold, K. (eds),Injecting illicit drugs,Addiction Press, Blackwell, Oxford, pp. 11–32.Grund, J-P. and Stern, L. (1991), ‘Residual blood in syringes: size and type of syringe are important’,AIDS5, pp.1532–3.Grund, J-P., Friedman, S., Stern, L., et al. (1996), ‘Syringe-mediated drug sharing among injecting drug users:patterns, social context, and implications for transmission of blood-borne pathogens’,Social Science and Medicine42, pp. 691–703.Grund, J-P., Zabransky, T., Irvin, K. and Heimer, R. (2009), ‘Stimulant use in central and eastern Europe: howrecent social history shaped current drug consumption patterns’, in Pates, R. and Riley, D. (eds),Interventions foramphetamine misuse,Wiley Blackwell, Oxford.Grund, J-P., Coffin, P., Jauffret-Roustide, M., et al. (2010), ‘The fast and furious: cocaine, amphetamines and harmreduction’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence,impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, PublicationsOffice of the European Union, Luxembourg.Gyarmathy, A., Neaigus, A., Mitchell, M. and Ujhelyi, E. (2009a), ‘The association of syringe type and syringecleaning with HCV infection among IDUs in Budapest, Hungary’,Drug and Alcohol Dependence100, pp. 240–7.Gyarmathy, A., Li, N., Tobin, K., et al. (2009b), ‘Correlates of unsafe injecting among injecting drug users in StPetersburg, Russia’,European Addiction Research15, pp. 163–70.Hagan, H., Thiede, H., Weiss, N., et al. (2001), ‘Sharing of drug preparation equipment as a risk factor forhepatitis C’,American Journal of Public Health91, pp. 42–6.Hakansson, A., Medvedeo, A., Andersson, M. and Berglund, M. (2007), ‘Buprenorphine misuse among heroinand amphetamine users in Malmo, Sweden: purpose of misuse and route of administration’,European AddictionResearch13, pp. 207–15.Hannon, F., Kelleher, C., Friel, S., et al. (2000),General healthcare study of the Irish prison populations,NationalUniversity of Ireland, Galway.Hartnoll, R. (2003) ‘Overview of the drugs situation in the CEECs: situation and responses’, in EMCDDA,The stateof the drugs problem in the acceding and candidate countries to the European Union,European Monitoring Centrefor Drugs and Drug Addiction, Lisbon, pp. 13–33.Hartnoll, R., Mitcheson, M., Battersby, A., et al. (1980), ‘Evaluation of heroin maintenance in a controlled trial’,Archives of General Psychiatry,37, pp. 877–84.Haydon, E. and Fischer, B. (2005), ‘Crack use as a public health problem in Canada: call for an evaluation of“safer crack use kits”’,Canadian Journal of Public Health96, pp. 185–8.
427
Harm reduction: evidence, impacts and challenges
Health Protection Agency, Health Protection Scotland, National Public Health Service for Wales and Centre forResearch on Drugs and Health Behaviour (2006),Shooting up: infections among injecting drug users in the UnitedKingdom 2005,Health Protection Agency, London.Hedrich, D., Pirona, A. and Wiessing, L. (2008), ‘From margin to mainstream: the evolution of harm reductionresponses to problem drug use in Europe’,Drugs: Education, Prevention and Policy15, pp. 503–17.Hedrich, D., Kerr, T. and Dubois-Arber, F. (2010), ‘Drug consumption facilities in Europe and beyond’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Henderson, G. (1988), ‘Designer drugs: past history and future prospects’,Journal of Forensic Science,33, pp.569–75.Hendrickson, R., Horowitz, Z., Norton, R. and Notenboom, H. (2006), ‘“Parachuting” meth: a novel deliverymethod for methamphetamine and delayed-onset toxicity from “body stuffing”’,Clinical Toxicology44, pp. 379–82.Henskens, R., Garretsen, H., Bongers, I., Van Dijk, A. and Sturmans, F. (2008), ‘Effectiveness of an outreachtreatment program for inner city crack abusers: compliance, outcome and client satisfaction’,Substance Use andMisuse,43, pp. 1464–75.Hickman, M., Hope, V., McDonald, T., et al. (2007), ‘HCV prevalence and injecting risk behaviour in multiplesites in England in 2004’,Journal of Viral Hepatitis,14, pp. 645–52.Horgan, J. (2007),An overview of cocaine use in Ireland,National Advisory Committee on Drugs and NationalDrugs Strategy Team, Dublin.Join Together (2007), ‘Oregon’s tough meth laws may have unintended consequences’,In the News.Available athttp://www.jointogether.org/news/headlines/inthenews/2007/oregons-tough-meth.html (accessed 15 June2009).Jose, B., Friedman, S., Neaigus, A., et al. (1993), ‘Syringe-mediated drug sharing (backloading): a new riskfactor for HIV among injecting drug users’,AIDS7, pp. 1653–60.Käll, K. and Nilsonne, A. (1995), ‘Preference for sex on amphetamine: a marker for HIV risk behaviour amongmale intravenous amphetamine users in Stockholm’,AIDS Care7, pp. 171–88.Käll, K. and Olin, R. (1990), ‘HIV status and changes in risk behaviour among intravenous drug users inStockholm’,AIDS4, pp. 153–7.Klee, H. (2006), ‘HIV risks for women injectors: heroin and amphetamines compared’,Addiction88, pp. 1055–62.Koslov, A., Shaboltas, A., Toussova, O., et al. (2006), ‘HIV incidence and factors associated with HIV acquisitionamong injection drug users in St. Petersburg, Russia’,AIDS20, pp. 901–06.Kruse, G., Barbour, R., Heimer, R., et al. (2009), ‘Drug choice, spatial distribution, HIV risk, and prevalenceamong injection drug users in St. Petersburg, Russia’,Harm Reduction Journal6 (22). Available at http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2731096/.Lelevich, V., Vintskaya, A., Lelevich, S., et al. (2008),Annual report: Republic of Belarus drug abuse and illicit drugstrafficking in 2007,BUMAD Programme, Minsk.Leonard, L., DeRubeis, E., Pelude, L., et al. (2008), ‘“I inject less as I have easier access to pipes”: injecting, andsharing of crack-smoking materials, decline as safer crack-smoking resources are distributed’,International Journalof Drug Policy19, pp. 255–64.
428
Chapter 15: Variations in problem drug use patterns and their implications for harm reduction
MacCoun, R. and Reuter, P. (2001),Drug war heresies: learning from other vices, times, and places,CambridgeUniversity Press, Cambridge and New York.McCoy, C., Shenghan, L., Metsch, L., Messiah, S. and Zhao, W. (2004), ‘Injection drug use and crack cocainesmoking: independent and dual risk behaviours for HIV infection’,Annals of Epidemiology14, pp. 535–42.McDonald, S., Hutchinson, S., Bird, S., et al. (2009), ‘A population-based record linkage study of mortality inhepatitis C-diagnosed persons with or without HIV coinfection in Scotland’,Statistical Methods in Medical Research18, pp. 271–83.Maher, L. and Dixon, D. (1999), ‘Policing and public health: law enforcement and harm minimisation in a street-level drug market’,British Journal of Criminology39, pp. 488–511.March, J., Oviedo-Joekes, E. and Romero, M. (2006), ‘Drugs and social exclusion in ten European cities’,European Addiction Research12, pp. 33–41.Ministerio de Sanidad y Consumo (2007),2007 National Report to the EMCDDA,Ministerio de Sanidad yConsumo, Spain.Ministero della Salute (2007),Proposta di Progetto Nazionale Cocaina, Dipartimento delle Dipendenze,RegioneLombardia, Italia. Available at http://www.indipendenze.org/sx_canale/dettaglio.asp?sez=Cocaina&id_sezione=1&id_subSez=110&id_articolo=1397.Miovský, M. (2007), ‘Changing patterns of drug use in the Czech Republic during the post-communist era: aqualitative study’,Journal of Drug Issues37, pp. 73–102.Molitor, F., Truax, S., Ruiz, J., et al. (1998), ‘Association of methamphetamine use during sex with risky sexualbehaviours and HIV injection among non-injection drug users’,Western Journal of Medicine168, pp. 93–7.Molitor, F., Ruiz, J., Flynn, N., et al. (1999), ‘Methamphetamine use and sexual and injection risk behaviorsamong out-of-treatment injection drug users’,American Journal of Drug and Alcohol Abuse25, pp. 475–93.Mravčík, V., Chomynová, P., Orlíková, B., et al. (2008),Výroční zpráva o stavu ve věcech drog vČeskérepublice vroce 2007[The Czech Republic: drug situation 2007], Úřad vládyČR,Praha [Office of the Czech Government,Prague].Neaigus, A., Gyarmathy, A., Zhao, M., et al. (2007), ‘Sexual and other noninjection risks for HBV and HCVseroconversions among noninjecting heroin users’,Journal of Infectious Diseases195 (7), pp. 1052–61.O’Byrne, P. and Holmes, D. (2008), ‘Evaluating crack pipe distribution in Canada: a systems change case study’,Addiction Research and Theory16, pp. 181–92.O’Donovan, D., Cooke, R., Joce, R., et al. (2001), ‘An outbreak of hepatitis A amongst injecting drug users’,Epidemiology and Infection127, pp. 469–73.OFDT (2003),Substitution aux opiacés en France, synthèse des informations disponibles de 1996 à 2001 en France,OFDT, Paris.OFDT (2007),2007 national report to the EMCDDA on the drug situation in France,OFDT, Paris.Ojanperä, I., Gergov, M., Liiv, M., Riijokoja, A. and Vuori, E. (2008), ‘An epidemic of fatal 3-methylfentalnylpoisoning in Estonia’,International Journal of Legal Medicine122, pp. 395–400.Otiashvili, D., Zabransky, T., Kirtadze, I., et al. (2009), ‘Why do the clients of Georgian needle exchangeprograms inject buprenorphine?’European Addiction Research16 (1), pp. 1–8.
429
Harm reduction: evidence, impacts and challenges
Partanen, T., Vikatmaa, P., Tukiainen, E., Lepantalo, M. and Vuola, J. (2009), ‘Outcome after injections of crushedtablets in intravenous drug abusers in the Helsinki University Central Hospital’,European Journal of Vascular andEndovascular Surgery37, pp. 704–11.Pavlenko, V. (2008), ‘Peculiarities of stimulant use in Ukraine: the example of Donetsk region’, 1st globalconference on methamphetamine: Science, Strategy and Response, 15 September, Prague.Perevoscikovs, J., Lucenko, I., Magone, S., et al. (2009), ‘Community-wide outbreak of hepatitis A in Latvia in2008: an update’,Eurosurveillance14 (3).Pfeiffer-Gerschel, T., Kipke, I., Lang, P., et al. (2008),2008 national report to the EMCDDA on the drug situationin Germany,DBDD, Munich.Pizzey, R. and Hunt, N. (2008), ‘Distributing foil from needle and syringe programmes (NSPs) to promotetransitions from heroin injecting to chasing: an evaluation’,Harm Reduction Journal5 (24). Available at http://www.harmreductionjournal.com/content/5/1/24.Porter, J., Drucker, E., Hammond, J. and Lax, L. (1994), ‘Crack smoking methods as risk factors for HIV infection’,International Conference on AIDS7–11 August, 10 (1), p. 391 (abstract no. PD0170).Pozner, C., Levine, M. and Zane, R. (2005), ‘The cardiovascular effects of cocaine’,Journal of EmergencyMedicine29, pp. 173–8.Prinzleve, M., Haasen, C., Zurhold, H., et al. (2004), ‘Cocaine use in Europe — a multicentre study: patterns ofuse in different groups’,European Addiction Research10, pp. 147–55.Rasmussen, D., and Benson, B. (1997), ‘Reducing the harms of drug policy: an economic perspective’,SubstanceUse and Misuse3, pp. 49–68.Rasmussen, D., Benson, B. and Sollars, D. (1993), ‘Spatial competition in illicit drug markets: the consequences ofincreased drug law enforcement’,Review of Regional Studies,123, pp. 219–36.Rehm, J., Gschwend, P., Steffen, T., et al. (2001), ‘Feasibility, safety, and efficacy of injectable heroin prescriptionfor refractory opioid addicts: a follow-up study’,Lancet,27 October, 358, pp. 1417–23.Rhodes, T. (2002), ‘The “risk environment”: a framework for understanding and reducing drug-related harm’,International Journal of Drug Policy13, pp. 85–94.Rhodes, T., Lowndes, C., Judd, A., et al. (2002), ‘Explosive spread and high prevalence of HIV infection amonginjecting drug users in Togliatti City, Russia’,AIDS16, pp. F25–31.Rhodes, T., Mikhailova, L., Sarang, A., et al. (2003), ‘Situational factors influencing drug injecting, risk reductionand syringe exchange in Togliatti City, Russian Federation: a qualitative study of micro risk environment’,SocialScience and Medicine57, pp. 39–54Rhodes, T., Stoneman, A., Hope, V., Hunt, N. and Judd, A. (2006), ‘Groin injecting in the context of crackcocaine and homelessness: from “risk boundary” to “acceptable risk”?’International Journal of Drug Policy17, pp.164–70.Rhodes, T., Briggs, D., Kimber, J., Jones, S. and Holloway, G. (2007), ‘Crack–heroin speedball injection and itsimplications for vein care: qualitative study’,Addiction102, pp. 1782–90.Roux, P., Villes, V., Bry, D., et al. (2008), ‘Buprenorphine sniffing as a response to inadequate care in substitutedpatients: results from the Subazur survey in south-eastern France’,Addictive Behaviors33, pp. 1625–9.Sánchez-Niubò, A., Fortiana, J., Barrio, G., et al. (2009), ‘Problematic heroin incidence trends in Spain’,Addiction104, pp. 248–55.
430
Chapter 15: Variations in problem drug use patterns and their implications for harm reduction
Seaman, S., Brettle, R. and Bied, S. (1998), ‘Mortality from overdose among injecting drug users recentlyreleased from prison’,BMJ316, pp. 426–8.Shaboltas, A., Toussova, O., Hoffman, I., et al. (2006), ‘HIV prevalence, sociodemographic and behaviouralcorrelates and recruitment methods among injection drug users in St. Petersburg, Russia’,Journal of AcquiredImmune Deficiency Syndrome41, pp. 657–63.Škařupová, K., Mravčík, V., and Orlíková, B. (2009), ‘Hard gelatine capsules as a harm reduction drug deliveryalternative to injecting’ (in press).Smith, J., Kacker, A. and Anand, V. (2002), ‘Midline nasal and hard palate destruction in cocaine abusers andcocaine’s role in rhinologic practice’,Ear, Nose and Throat Journal81, pp. 172–4, 176–7.SIRUS (Norwegian Institute for Alcohol and Drug Research) (2008),2008 national report to the EMCDDA on thedrug situation in Norway,SIRUS, Oslo.Sozialdepartement der Stadt Zürich (2008),Ein Ort wo man sein kann. Dir Zukunft der „Harm Reduction“ amBeispiel der Kontakt- und Anlaufstellen der Stadt Zürich,Edition Sozialpraxis Nr. 3, Zürich: Stadt Zürich.Stakes (2008),2008 national report to the EMCDDA on the drug situation in Finland,Stakes, Helsinki.Strang, J., Sheridan, J. and Barber, N. (1996), ‘Prescribing injectable and oral methadone to opiate addicts:results from the 1995 national postal survey of community pharmacies in England and Wales’,BMJ3 August,313, pp. 270–2.Strang, J., Manning, V., Mayet, S., et al. (2008), ‘Overdose training and take-home naloxone for opiate users:prospective cohort study of impact on knowledge and attitudes and subsequent management of overdoses’,Addiction103, pp. 1648–57.Talu, A., Abel-Ollo, K., Vals, K. and Ahven, K. (2008),2008 national report to the EMCDDA on the drug situationin Estonia,National Institute for Health Development, Tallinn.Talu, A., Rajaleid, K., Abel-Ollo, K., et al. (2010), ‘HIV infection and risk behaviour of primary fentanyl andamphetamine injectors in Tallinn, Estonia: implications for intervention’,International Journal of Drug Policy21, pp.56–63.Topp, L., Day, C. and Degenhardt, L. (2003), ‘Changes in patterns of drug injection concurrent with a sustainedreduction in the availability of heroin in Australia’,Drug and Alcohol Dependence70, pp. 275–86.Tortu, S., McMahon, J., Pouget, E. and Hamid, R. (2004), ‘Sharing of noninjection drug-use implements as a riskfactor for hepatitis C’,Substance Use and Misuse,39, pp. 211–24.Tyndall, M., Currie, S., Spittal, P., et al. (2003), ‘Intensive injection cocaine use as the primary risk factor in theVancouver HIV-1 epidemic’,AIDS17, pp. 887–93.Uusküla, A., Kals, M., Rajaleid, K., et al. (2008), ‘High-prevalence and high-estimated incidence of HIV infectionamong new injecting drug users in Estonia: need for large scale prevention programs’,Journal of Public Health30,pp. 119–25.Vallejo, R., de Leon-Casasola, O. and Benyamin, R. (2004), ‘Opioid therapy and immuno-suppression: a review’,American Journal of Therapeutics11, pp. 354–65.van Beek, I., Buckley, R., Stewart, M., MacDonald, M. and Kaldor J. (1994), ‘Risk factors for hepatitis C virusinfection among injecting drug users in Sydney’,Genitourin Med70, pp. 321–4.van Beek, I., Dwyer, R. and Malcom, A. (2001), ‘Cocaine injecting: the sharp end of drug-related harm’,Drugand Alcohol Review20, pp. 333–42.
431
Harm reduction: evidence, impacts and challenges
Vicente, J., Giraudon, I., Matias, J., Hedrich, D. and Wiessing, L. (2009), ‘Rebound of overdose mortality in theEuropean Union 2003–2005: findings from the 2008 EMCDDA Annual Report’,EurosurveillanceEdition, 14 (2).Available at http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19088.VWS (2008),Tätigkeitsbereicht 2007,ChEckiT!, Verein Wiener Sozialprojekte, Vienna. See ÖBIG (2008), 2008national report to the EMCDDA on the drug situation in Austria, Österreichisches Bundesinstitut fürGesundheitswesen, Vienna, Table A20.Williamson, A., Darke, S., Ross, J. and Teesson, M. (2006), ‘The association between cocaine use and short-termoutcomes for the treatment of heroin dependence: findings from the Australian Treatment Outcome Study (ATOS)’,Drug and Alcohol Review25, pp. 141–8.Wood, E., Tyndall, M., Spittal, P., et al. (2002), ‘Needle exchange and difficulty with needle access during anongoing HIV epidemic’,International Journal of Drug Policy,13, pp. 95–102.Zabransky, T. (2009), unpublished qualitative research on drug producers and police officers.Zeziulin, O., Dumchev, K. and Schumacher, J. (2008), ‘Injection stimulant use and HIV risk in Ukraine’, 1st GlobalConference On Methamphetamine: Science, Strategy And Response, 15 September, Prague.Zule, W. and Bobashev, G. (2009), ‘High dead-space syringes and the risk of HIV and HCV infection amonginjecting drug users’,Drug and Alcohol Dependence100, pp. 204–13.Zule, W., Ticknor-Stellato, K., Desmond, D. and Vogtsberger, K. (1997), ‘Evaluation of needle and syringecombinations’,Journal of Acquired Immune Deficiency Syndrome and Human Retrovirology14, pp. 294–5.Zule, W., Desmond, D. and Neff, J. (2002), ‘Syringe type and drug injector risk for HIV infection: a case study inTexas’,Social Science and Medicine55, pp. 1103–13.
432
Conclusions
Chapter 16Current and future perspectives on harm reduction in theEuropean UnionMarina Davoli, Roland Simon and Paul Griffiths
The drift to evidence-based European drug policiesOver the last 20 years, whether as an overarching concept, or as shorthand for specificinterventions, ‘harm reduction’ has changed the way we think about and respond to drugproblems in Europe. Debates continue today about what sort of interventions legitimately fallunder the heading of harm reduction, and what value they bring. However, measures thatreduce harm, but do not specifically attempt to reduce drug use, are an important element ina drug strategy and harm reduction is now a largely uncontested component of Europeandrug policy. Indeed, practice is ahead of political rhetoric in this respect, with governmentssometimes being more cautious in their public pronouncements than they are in their actions.How Europe got to today’s pragmatic approach, where the balance is tipped to what can beshown to work,rather than what policymakers mightwish would work,is addressed by manyof the contributors to this monograph. It would be naive to suggest that modern drug policiesare solely directed by a cold assessment of the scientific evidence for effectiveness. Manyexamples can be cited to demonstrate that this is not the case — for instance, the investment oflarge sums of money in anti-drug mass media campaigns where there is growing evidence thatthis approach is at best ineffective, and at worst counter-productive. Drug policies, like othersocial policies, are shaped by many factors, and Herring and colleagues’ (2010) statement onalcohol is true for other substances as well: ‘Evaluation and research findings are only oneelement in decisions to adapt or reject harm reduction as a legitimate goal for policy’.Nonetheless, the development of harm reduction as a mainstream concept in Europe doesdemonstrate that over time, and when faced with a serious public health threat, evidence-basedargument can result in the adoption of policy options that are initially viewed as controversial. Itis beyond the scope of this chapter to discuss how the mainstreaming of harm reduction intodrug policy was possible in the European Union (EU) and some other countries, whilst in otherparts of both the developed and developing world harm reduction has remained largely outsideof the mainstream. The diffusion of harm reduction in Europe was brought about initially bypublic health concerns related to HIV. It seems likely it has also been facilitated by structuralfactors, including a strong public health ethos, a culture of independence within the medical andhealth professions, activism and user involvement, and advocacy by affected individuals andcommunities. At the EU level, a growing political culture of sharing experiences of what worksand moving towards common positions may have also played a part and, importantly, removedsome of the anxiety felt by policymakers that they were moving alone into uncharted waters. It isinteresting to note that many of the Member States joining the EU in 2004 very rapidly adoptedrelatively sophisticated drug policies that reflected Community norms, and in which harm437
Harm reduction: evidence, impacts and challenges
reduction was a component. Arguably, a key factor contributing to these countries’ avoidance ofmajor HIV epidemics among their injecting populations is their rapid adoption of the Europeanmodel in which HIV prevention was an integral element.
The question of definitionInterventions towards substance use and dependence have always been topics of discussionwell beyond the public health arena. Ethical issues relating to the use of drugs have influencedthe objectives and aims of interventions, both preventive and therapeutic. Indeed, the historicaldevelopment of drug policy is often represented as an ongoing debate between amoralpositionin which drug use is portrayed as ‘criminal’ and ‘deviant’ and apublic health positionwhere drug users are seen as in need of treatment and help. Harm reduction gives clearprimacy to a public health perspective in which the imperative is to reduce immediate harms,and the question of long-term abstinence from drug use is either unaddressed or left open.Moreover, many of those who advocate for a harm reduction approach also point out that theregulatory control system itself can contribute to harm, and some regard it as a majorcontributing factor. Furthermore, some, on both sides of the drugs debate, would equate harmreduction as running in close parallel to an anti-prohibitionist perspective. However, it isimportant to note that the mainstreaming of harm reduction within political policy debate at theEuropean level has taken place overwhelmingly within a context of concern about the health ofthe public and has not be linked with the issue of drug prohibition.From a European policy perspective, where Member States’ domestic policies differ, thequestion of definition is an important one; or conversely, an important area for flexibility ininterpretation. A fundamental position of current European drug policy is support for theinternational drug control conventions, and no European country would regard its policies asout of step with the leeway given to States to interpret their obligations in this respect. Harmreduction as mainstream in Europe is therefore viewed by policymakers as compatible with abalanced approach, which also includes support for vigorous supply reduction measures.This is not to say that policymakers have ignored the argument that harms can result from thedrug control system. Recognition of this fact can be seen, for instance, in a shift in emphasisin which a distinction is now commonly made between those who traffic and trade in drugs,and those who consume them. It is reflected in policies that attempt to divert those with drugproblems from the criminal justice system towards treatment or that introduce more lenientpenalties for the personal use of drugs. These developments have, however, largely takenplace within a policy debate on how the costs of drug control can be minimised and thebenefits maximised. The reduction of harm is clearly part of this agenda, but this is usuallyimplicit rather than explicit and harm reduction is most commonly discussed in the context ofHIV risk reduction, not criminal justice policies. A strong argument can be made that theabsence of an explicit common definition of what constitutes ‘harm reduction’ at the EU levelhas facilitated the mainstreaming of the concept against a background where there isconsiderable diversity in respect to national and local policies and actions. And when eventshave forced the adoption of a working definition the approach has usually been a relativelyrestricted one: for example, explicitly listing measures targeting HIV risk behaviour amongdrug injectors.438
Chapter 16: Current and future perspectives on harm reduction in the European Union
The question of evidenceThe mantra for the European approach to drugs is for comprehensive, balanced andevidence-based policies. The importance given to evidence in this perspective can becontrasted with policies that are more ideologically driven. This raises two importantquestions. First, what constitutes sufficient evidence for policy formation? And second, to what extent are policies skewed towards the easily measurable, at the expense of the potentiallymost desirable? It is probably fair to say that in many areas of drug policy the evidence base for supportingcurrent approaches is often weak, and where evidence does exist it is rarely unequivocal.That said, the situation is considerably better than it once was and research and evaluationstudies provide a growing base of evidence for informing policy decisions. It isunderstandable that policymakers will be more concerned with the quality and availability ofevidence for politically controversial measures than they are for actions that have broad-based support. This is likely to be why harm reduction has come under greater scrutiny thanmany other areas of drug policy, although this is arguably changing in light of a moregeneric concern to fund only interventions that can be shown to be effective.Appraisal of the available evidence for an intervention is a complex process requiringmethodological rigour, particularly in conducting a comprehensive search of the literature,evaluating quality of primary studies and summarising the results (Higgins and Green, 2008).The credibility of this process depends on a rigorous approach to the evaluation exercise. Thegold standard for the evaluation of medical research is the randomised control trial (RCT).This model is often applied to drug interventions, especially in the more medically orientatedareas such as treatment. Interventions can be considered effective if there is evidencederiving from multiple well-conducted studies. In the last 15 years, considerable efforts havebeen made to ensure that all conducted RCTs are registered and their findings madeaccessible. This is not the case for most other types of research and comprehensively auditingand accessing the evidence base for other types of study design is consequently moredifficult. The efforts made to improve the quality of reporting for RCTs has also to some extentresulted in an improvement in quality of the studies published in the scientific literature(Moher et al., 2001; Plint et al., 2006). Only recently have guidelines for reporting results ofstudy designs other than RCTs also been published (von Elm et al., 2007).For good reason, RCTs therefore represent a gold standard for research evidence as, whenreplicated and properly applied, they provide a robust evidence base for demonstrating witha high probability of certainty that a given intervention has resulted in a measurable effect.They do, however, have some obvious weaknesses that have important implications for theiruse in the drugs field. RCTs work best with simple study designs and where extraneousvariables can easily be controlled for. This model fits well for testing the effectiveness of anew medicine where the condition to be treated is well described and the desired action ofthe drug can be easily measured. However, harm reduction interventions usually take placein real world settings, in which other interventions may also be taking place. Furthermore,confounding variables are difficult to control for, subject characteristics are often highlyheterogeneous, and outcomes may be complex to interpret and difficult to measure. Practical,439
Harm reduction: evidence, impacts and challenges
methodological and ethical challenges exist to developing convincing RCT study designs thatare applicable to many areas of social policy evaluation. This is a particular problem forcontroversial social policy options as it may be in practice very difficult using other studydesigns to provide policymakers with the high level of certainty that properly conducted RCTscan provide. The number of RCT study designs in the harm reduction area is growing butremains limited. Not surprisingly RCTs are most commonly found in the treatment area, asthis setting is most amenable to this kind of approach. In considering other areas, theevidence is largely drawn from more observational studies and ecological ones. Such studiesprovide a weaker evidence base for drawing conclusions and can be more challenging tointerpret. These kind of studies are probably also at higher risk of publication bias, wherethere is a greater likelihood of getting positive rather than negative results published,although RCTs are not immune to this problem.This monograph has provided the reader with a systematic review of the evidence regardingharm reduction among injecting opiate users. In other areas, the lack of studies makes asystematic appraisal more difficult but the contributions elaborate the evidence that exists. Inorder to consider future priorities for the European research agenda, we provide below anoverview, using strict assessment criteria, of the current state of the art with respect to theevidence for effectiveness of harm reduction activities. The reader should note that lack ofrobust evidence means that the research conducted so far is not sufficient to make confidentjudgements, negative or positive, on the effectiveness of the intervention in question.Harm reduction among injecting drug usersThere is sufficient evidence to support the role of opioid substitution treatment (OST) inreducing HIV transmission, while the evidence in support of needle and syringe distributionprogrammes is more tentative, and the evidence that drug consumption reduces transmissionis insufficient at present. All three interventions appear to reduce self-reported injecting riskbehaviour. The evidence on the impact of drug consumption rooms and peer naloxonedistribution in reducing overdose deaths at the community level remains insufficient, althoughthe studies that have been conducted suggest the potential that these approaches may haveand therefore both interventions remain important areas for further study. No strongevidence exists to support the concern that any of these interventions, when well managed,leads to increased harms for those using them, or encourages drug use in the widercommunity. However, a problem with the diversion of drugs from substitution treatment intothe illicit market has been reported in some countries.In terms of research priorities, methodologically robust primary studies on the impact of harmreduction interventions on the incidence of HIV and HCV are needed as are studies on whatmeasures may reduce drug overdose deaths. In the EU, drug overdose now represents themajor cause of avoidable morbidity associated with illegal drug use and therefore must beregarded as a priority area for the identification of effective interventions. In general, futurestudies of interventions designed to reduce drug-related infectious diseases would be wise tofocus on primary biological outcomes rather than behavioural ones, as this is a key weaknessin current evidence. Where possible, randomised designs should be employed and compare440
Chapter 16: Current and future perspectives on harm reduction in the European Union
the impact of additional or increased intensity of interventions against current or low level ofactivity. A number of studies have suggested that the impact of interventions may beenhanced by, or even dependent upon, providing the target population with a package ofdifferent services. This implies the need to research how different interventions work togetherto provide benefit. Although this approach is analogous to some standard medical researchquestions — the provision of multi-drug therapy, for example — for interventions conductedin the real world settings, in which most harm reduction approaches are employed, suchresearch questions pose real methodological challenges. More innovative approaches,including natural experiments, large-scale modelling and carefully evaluated case studies,may prove to be the way forward here.Harm reduction policies for cocaine and other stimulantsThere is now greater understanding of the mental and physical health consequencesassociated with the use of cocaine and other stimulants. However, to date, most harmreduction interventions have largely focused on risks related to infectious diseasestransmission and assumptions are built largely on the evidence of HIV prevention amongheroin injectors.Although some studies have looked at crack cocaine users overall, there is little evidencefrom published studies on the effectiveness of harm reduction interventions among users ofcocaine or other stimulants. This population is often considered a subset of a study, ratherthan the target population, and most research has exclusively focused on intravenous druguse. Interventions for crack users have been developed based on the assumption thatproviding material for safer crack smoking will reduce the risk of viral transmission, but thesehave not yet been systematically evaluated.No convincing evaluations, and very limited service development, has targeted the majorityof stimulant users who neither inject nor smoke their drugs. Some limited experimentationwith pill testing initiatives has been conducted in some countries, but it has not beensystematically evaluated, and recently the limited support for this kind of programmeappears to be waning further.‘Safer dancing’ programmes have looked at environmental risks such as fire safety anddrinking water availability along with information-giving. Impact evaluations are notavailable in this area but as these measures are not viewed as particularly controversial andgenerally considered to represent sensible public health and safety measures, this may not bea priority as long as investment in researching more controversial measures is lacking.In terms of research priorities, the extent of stimulant-related harm in Europe remains largelyunmeasured. Around 400 deaths per year are thought to be associated with cocaine use butthis may be an underestimate, as the extent to which cocaine use is an aggravating factor indeaths related to cardiovascular problems remains unknown. Treatment demands forstimulants are growing however, and some countries have long-established amphetamineinjection populations that are probably not directly comparable to opioid injectors.441
Harm reduction: evidence, impacts and challenges
The pattern of polydrug use consumption, especially the co-use of alcohol, is also likely to bea major issue both for assessing the harm of different consumption patterns and for targetinginterventions. Put simply, despite the growing importance of stimulant use with the Europeandrug field, there is very little research evidence to permit an informed analysis of theeffectiveness of harm reduction interventions and therefore even informed speculation onwhat approaches might prove successful currently remains difficult.Harm reduction policies for cannabisDespite a growing interest in, and evidence base for, harms attributed to cannabis use thereis very limited evidence of effectiveness of the proposed harm reduction strategies in thisarea. There is not sufficient evidence that roadside drug-testing reduces mortality due to carcrashes. Screening and brief interventions for excessive cannabis users have been proposedas adaptations of similar interventions for alcohol abuse, but no sufficient evidence isavailable yet on their effects. Vaporisers and other developing technology may reduce therisks associated with smoking cannabis products but the extent to which this is so remainsunclear. The question also remains open on the extent to which vaporisers are likely to beviewed by consumers as acceptable alternatives to current modes, especially given the linkbetween tobacco smoking and cannabis use that exists in Europe. There is therefore a widerange of important questions to be addressed by well-constructed primary research in thisarea. These include, but are not limited to: the extent to which roadside testing would reducemotor vehicle accident fatalities; whether informing cannabis users about related harms canreduce the actual levels of problems experienced; to what extent brief interventions canreduce harm; and how new technologies, or behavioral changes, reduce risks associatedwith smoking.Harm reduction policies for tobaccoThere is good evidence that public smoking bans and mandatory reduced ignitionpropensity standards for cigarettes reduce tobacco-related harms to non-smokers andimprove health at the population level. There is no evidence that modified smokedtobacco products and cigarette-like devices substantially reduce harm, and limitedevidence that pharmaceutical nicotine or low nitrosamine smokeless tobacco productsmight reduce tobacco-related harm in those who are unable or unwilling to quit but arewilling to switch to such products. Nonetheless, given the high probability of healthdamage for those who continue to smoke there remains a considerable need for primaryresearch into the extent to which innovative new products would be attractive to currentsmokers and to what extent they can reduce harm to users who are unable to quit. Aparallel research question would be the extent to which ‘safer smoking technologies’,should they become available, would undermine smoking reduction policies at thepopulation level. This is, however, an area in which multi-site RCTs to evaluate bothbenefits and risks of new products are clearly feasible. Studies in this area will need toidentify biomarkers that are sensitive to short-term changes in smoking behaviour and arealso predictive of long-term harm.442
Chapter 16: Current and future perspectives on harm reduction in the European Union
Alcohol harm reductionThere is sufficient evidence on the effectiveness for some outcome measures of a total ban onsales, minimum legal purchase age, government monopoly and restrictions of retail sales,alcohol taxes, lowered limits of blood alcohol concentration (BAC) for car drivers and lowBAC limits for young drivers. There are several studies on public service messages andalcohol education in school but no evidence of effectiveness. There are too few studies in theareas of voluntary codes of bar practice, promoting alcohol-free activities, warning labels,college student education, designated drivers and ride services to allow comment on theireffectiveness, although all these areas appear interesting topics for further research. Ingeneral there is a growing interest in interventions that can reduce the harm accruing fromalcohol use, and across Europe alcohol problems are becoming an area of greater policyconcern. As drugs and alcohol are often consumed together in recreational settings thechallenge will be to develop research designs that are adequate to the complexities ofassessing interventions targeting poly substance consumption patterns. Finally, in this area aclear need exists for a thorough systematic review to identify the key gaps in the currentknowledge base and provide a better road map for setting future research priorities.
Pragmatism, policy and the evidence baseThe value of taking a strict approach to assessing the quality of evidence concerning the impactof harm reduction interventions is that it allows policymakers to make decisions with greatercertainty. The problem, however, is that this may set the bar too high, given that in the ‘realworld’ there are practical, methodological and ethical reasons that mean that it may beextremely difficult or even impossible to generate such a high level of evidence. Moreover, if RCTdesigns are employed it may be necessary to control the parameters of the study so strictly thatany findings may have limited applicability to the real world setting in which harm reductioninterventions typically take place. This problem is not restricted to harm reduction but is commonto many areas of social policy. Models are being developed that try to incorporate the availableevidence to inform policy formation even if this has to be based on a lower level of certainty.An interesting development in this field is the guidelines produced by the GRADE methodgroup (Guyatt et al., 2008). This approach clearly opens the way towards considering otherstudy designs in appraising the evidence. An example of this can be found in the recentlypublished WHO guidelines for substitution treatment, which used non-randomised studies toevaluate the evidence supporting recommendations for the use of substitution treatment inreducing HIV infection and mortality (WHO, 2009).In reality, policymakers are often faced with making choices in areas in which a high level ofcertainty is lacking and pragmatic choices are required. But how can pragmatic policy choicebe supported? Evidence that interventions are not producing harm to those that receive them or to the wider community is likely to be important. As is evidence that they are reaching theirintended recipients, who are appearing to benefit from well-constructed measures. If there is noevidence of harm, and some evidence of benefit, it can help to provide sufficient justification forpragmatic policy choices to be made, even when clear evidence of effectiveness is lacking.443
Harm reduction: evidence, impacts and challenges
This can be seen in the area of needle and syringe exchange where the evidence can still beregarded as tentative in respect of demonstrating that HIV transmission is reduced. However,numerous studies do show that reported risk behaviour is lowered and/or are suggestive thatprovision of syringe exchange can be associated with low, or reduced, rates of new HIVinfections at the population level. Moreover, no strong evidence exists that this type ofintervention delivers harm, although this concern has been repeatedly raised by those whowere hostile to the development of this kind of service.When faced with this evidence policymakers in Europe have made a pragmatic choice thatthere is sufficient data to include this sort of provision in a comprehensive package of servicesfor drug injectors, even if it is still not possible to show conclusively that such services reduceby themselves rates of new infections. In practice needle and syringe programmes (NSPs) areusually not isolated services, but are typically implemented by agencies who offer a range ofother services, operate in a variety of settings, and in the context of diverse epidemic andbehavioral scenario. A multitude of mediating factors therefore have to be accounted forwhen assessing their impact, which complicate both the collection and interpretation ofevidence.
Future perspectives: harm reduction and contemporary patterns of druguse in EuropeThis monograph has provided a state-of-the-art reflection on the development of harmreduction services in Europe and considered what we know about their effectiveness. It hasprovided historical context and an analytical framework for understanding how harmreduction approaches have moved into the mainstream in Europe. It has also launched adiscussion on the potential role for harm reduction in addressing the problems caused by theconsumption of alcohol and tobacco. The EMCDDA’s role is to monitor and report on druguse in Europe and the policies and responses Member States have developed to respond tothe drug situation. It is from this perspective that we offer some concluding remarks on thefuture challenges that changing patterns of drug use will bring to the debate in Europe onhow best to reduce the harm associated with drug consumption.Drug policy at the European level is not only concerned with understanding the situationwithin the EU. An explicit element of the EU drug strategy and accompanying action plans isto enable the EU to have a strong and united voice in the international debate on drugs. Thisis important for many reasons, not least because the future drug problem faced by the EUwill be influenced by the situation and policies of other countries. Drug problems transcendnational boarders and are becoming increasingly global in nature. In this context, thesituation in countries bordering the EU is clearly an important factor for consideration.The issues for the diffusion of harm reduction practice look somewhat different when lookingout from Europe rather than within. In many non-EU countries HIV epidemics among injectorsappear to be a growing problem, the availability of services of all types is often limited, andconsiderable political and professional resistance can exist to introducing harm reductionapproaches, even where the evidence base is robust. In international debates and in funding444
Chapter 16: Current and future perspectives on harm reduction in the European Union
for development programmes, Europe has supported the role of harm reduction as animportant part of a comprehensive HIV prevention strategy. This battle is far from won.Globally the problem of HIV infections acquired through drug injection remains a criticallyimportant public health issue and one in which Europe is likely to want to remain a strongadvocate for evidence-based approaches.Within the EU, preventing HIV infections related to drug injection remains an importantobjective for drug policies and there is a need to develop services and responses further.However, it no longer has the primacy it once had. Overall, the long-term trend appears tobe for a stabilisation, or fall, in both levels of injecting, and opiate use, and despite somelocalised problems the assessment of the situation in respect to drug related HIV infections isgenerally a positive one (EMCDDA, 2009). Despite this, morbidity and mortality associatedwith drug injecting remains considerable. There is a need to develop treatment regimes thatare attractive to those that are currently hard to treat. There is a need to develop effectiveapproaches to HCV infection — which is found virtually universally at high prevalenceamong drug injectors across Europe. Finally, there is a pressing need to find effectivemeasures to address opioid-associated drug overdose. This is now the major avoidable causeof morbidity amongst injectors. To date, in each of these areas some innovative harmreduction approaches have been developed, but the evidence base for informingpolicymakers remains inadequate.At points throughout this monograph it has been argued that harm reduction interventionsmay sometimes be most effective when provided as part of a ‘package’ of care, rather thanas a stand-alone approach. If this is the case, a challenge for the future will be to developresearch and evaluation designs that are adequate to the task of exploring the impact ofprogrammes delivered consequently, and across different levels of intensity. Methodologicallythis is no trivial task. Nonetheless, progress in this direction is required to gain a more holisticunderstanding of how interventions work in order to inform spending choices on what sort ofprogramme mixes are likely to be most appropriate.During the 1980s, and 1990s, the concept of problem drug use in Europe was virtuallysynonymous with opioid use and drug injection. It was recognised that some, mainly Nordic,countries had long-established amphetamine injecting populations, that smoking wasbecoming a common mode of administration among some heroin using groups, and thatdrugs like ecstasy were becoming more important on the recreational drug scene. However,the focus for discussions on drug problems remained very much on the chronic use of heroinusually by injection. The perspective today looks very different. Heroin and injectingproblems remain with us, but policymakers are equally concerned by what can be seen as abroader, more complex and faster moving drug situation.Today’s concerns are as likely to focus on the widespread use of cocaine and otherstimulants, the misuse of medicinal products, polydrug use including the use of licit substancesor even intensive cannabis use, as they are to focus on heroin injecting. To some extent theharm reduction agenda has failed to keep pace with the political one in this respect. Achallenge for the future growth of harm reduction services in Europe will be to developintervention models that address the harms associated with a broader set of consumption445
Harm reduction: evidence, impacts and challenges
patterns. This monograph helps to chart where developments are needed in these areas.Here, the boundaries between drug prevention, drug treatment and harm reduction becomeincreasingly fluid. This can be seen at the service level, for example in brief interventions forcannabis users, and at the individual level, for example where practitioners develop clientcare plans that include prevention, treatment and harm reduction services simultaneously.Finally, this monograph has concentrated on the topic of evidence and how it should beassessed. Yet it is important to remind ourselves that the absence of evidence does notnecessarily justify the absence of action. As Fry (2010) argues in his discussion on the ethicalaspects of harm reduction, ‘values’ have to be taken into account, especially when disputesand uncertainty about ‘facts’ exist. In this policy field, ‘evidence’ can be a preciouscommodity. The challenge for the research community is to provide policymakers with ahigher degree of certainty that the policies and actions they pursue are more likely to reducerather than augment harm.
ReferencesEMCDDA (European Monitoring Centre for Drugs and Drug Addiction) (2009),Annual report 2009: the state ofthe drugs problem in Europe,Publications Office of the European Union, Luxembourg.European Union (2008), ‘EU drugs action plan for 2009–2012’, 2008/C 326/09,Official Journal of the EuropeanUnion,20 December, C326/7–25.Fry, C. (2010), ‘Harm reduction: an “ethical” perspective’, in Chapter 4, ‘Perspectives on harm reduction: whatexperts have to say’, in European Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction:evidence, impacts and challenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10,Publications Office of the European Union, Luxembourg.Guyatt, G. H., Oxman, A. D., Kunz, R., et al. for the GRADE Working Group (2008), ‘Going from evidence torecommendations,BMJ10 May, 336 (7652), pp. 1049–51.Herring, R., Thom, B., Beccaria, F., Kolind, T. and Moskalewicz, J. (2010), ‘Alcohol harm reduction in Europe’, inEuropean Monitoring Centre for Drugs and Drug Addiction (EMCDDA),Harm reduction: evidence, impacts andchallenges,Rhodes, T. and Hedrich, D. (eds), Scientific Monograph Series No. 10, Publications Office of theEuropean Union, Luxembourg.Higgins, J. P. T. and Green, S. (eds) (2008),Cochrane handbook for systematic reviews of interventions,version5.0.1 (updated September 2008), The Cochrane Collaboration. Available at www.cochrane-handbook.org.Moher, D., Schulz, K. F. and Altman, D. G. (2001), ‘The CONSORT statement: revised recommendations forimproving the quality of reports of parallel-group randomised trials’,Lancet357 (9263), pp. 1191–4.Plint, A. C., Moher, D., Morrison, A., et al. (2006), ‘Does the CONSORT checklist improve the quality of reportsof randomised controlled trials? A systematic review’,Medical Journal of Australia185 (5), pp. 263–7.von Elm, E., Altman, D. G., Egger, M., Pocock, S. J., Gøtzsche, P. C. and Vandenbroucke, J. P. (2007), ‘STROBEinitiative: the strengthening the reporting of observational studies in epidemiology (STROBE) statement —guidelines for reporting observational studies’,Lancet20 October, 370 (9596), pp. 1453–7.WHO (World Health Organization) (2009),Guidelines for the psychosocially assisted pharmacological treatment ofopioid dependence,WHO, Geneva. Available at http://www.who.int/substance_abuse/publications/opioid_dependence_guidelines.pdf.
446
ContributorsEditorsTim RhodesProfessor of Public Health Sociology, andDirector, Centre for Research on Drugsand Health Behaviour, London School ofHygiene and Tropical Medicine,University of London, UKDagmar HedrichSenior Scientific Analyst, Health andSocial Responses, European MonitoringCentre for Drugs and Drug Addiction,Lisbon, Portugal
AuthorsEliot AlbertDrug user activist and researcher, London,UKINPUD Membership SecretaryRifat AtunProfessor of Evaluation, and Director ofStrategy, Performance and Evaluation,Global Fund to Fight AIDS, Tuberculosisand Malaria, Geneva, SwitzerlandAndrew BallSenior Strategy and Operations Advisor,Department of HIV/AIDS, World HealthOrganization, Geneva, SwitzerlandFranca BeccariaResearcher and Partner, Eclectica(research and communications agency),Turin, and Teacher Fellow, University ofTurin, ItalyPeter BlankenSenior Researcher, Parnassia AddictionResearch Centre, The Hague, theNetherlands, and Central CommitteeHeroin Addiction Treatment (CCBH),Utrecht, NetherlandsCinzia BrentariEuropean Institute of Social Services,University of Kent, UKJamie BridgeSenior Coordinator: Events andCommunications, International HarmReduction Association, UKDick de BruinDirector, Addiction Research Centre,Utrecht, NetherlandsAmador CalafatPresident, European Institute of Studies onPrevention, SpainPhilip CoffinInfectious Diseases Fellow, Division ofAllergy and Infectious Diseases, Universityof Washington, USACatherine CookSenior Analyst: Public Health and Policy,International Harm ReductionAssociation, UK449
Harm reduction: evidence, impacts and challenges
Marina DavoliDirector of Clinical Epidemiology,Department of Epidemiology, ASL, Rome,ItalyMinke DijkstraProject Director, Addiction ResearchCentre, Utrecht, NetherlandsFran§oise Dubois-ArberHead, Unit for the Evaluation onPrevention Programmes, Institute of Socialand Preventive Medicine (IUMSP),University Hospital Centre and Universityof Lausanne, SwitzerlandBenedikt FischerProfessor, Centre for Applied Research inMental Health and Addictions (CARMHA),Faculty of Health Sciences, Simon FraserUniversity, Vancouver, and Centre forAddiction and Mental Health (CAMH),Toronto, CanadaAdam FletcherLecturer, Centre for Research on Drugsand Health Behaviour, London School ofHygiene and Tropical Medicine, Universityof London, UKCraig FryMurdoch Childrens Research Institute(Children’s Bioethics Centre) and Universityof Melbourne (Centre for AppliedPhilosophy and Public Ethics), AustraliaCoral GartnerPost-doctoral Fellow, School of PopulationHealth, University of Queensland,Australia450
David GoldbergProfessor of Public Health, HealthProtection Scotland, Glasgow, UKPaul GriffithsScientific Coordinator and Head ofEpidemiology, Crime and Markets Unit,European Monitoring Centre for Drugsand Drug Addiction, Lisbon, PortugalJean-Paul GrundSenior Researcher, CVO — Research &Consultancy, Utrecht, Netherlands.Epidemiology Section, Department ofHealth, City of The Hague, theNetherlandsV. Anna GyarmathyScientific Writer, European Monitoring Centrefor Drugs and Drug Addiction, Lisbon,Portugal, and Adjunct Assistant Professor,Johns Hopkins Bloomberg School of PublicHealth, Baltimore, MD, USAWayne HallProfessor of Public Health Policy andNHMRC Australia Fellow, School ofPopulation Health, University ofQueensland, AustraliaRichard HartnollConsultant, formerly Head of Departmentof Epidemiology, European MonitoringCentre for Drugs and Drug Addiction,Lisbon, PortugalDagmar HedrichSenior Scientific Analyst, Health andSocial Responses, European MonitoringCentre for Drugs and Drug Addiction,Lisbon, Portugal
Contributors
Rachel HerringSenior Research Fellow, School of Healthand Social Sciences, Middlesex University,UKMatthew HickmanReader in Public Health, Department ofSocial Medicine, University of Bristol, UKNeil HuntDirector of Research, KCA; HonorarySenior Research Associate, University ofKent; Honorary Research Fellow, LondonSchool of Hygiene and Tropical Medicine,University of London, UKSharon HutchinsonSenior Research Fellow, Department ofStatistics and Modelling, University ofStrathclyde, Glasgow, UKMarie Jauffret-RoustideSociologist and Public Health Researcher,Centre for Research in Psychotropics,Health, Mental Health and Society,University of Paris-Descartes, Paris, andNational Institute for Public HealthSurveillance, Saint-Maurice, FranceMichel KazatchkineProfessor, and Executive Director, GlobalFund to Fight AIDS, Tuberculosis andMalaria, Geneva, SwitzerlandThomas KerrDirector, Urban Health ResearchInitiative, BC Centre for Excellence inHIV/AIDSAssistant Professor, Dept. of Medicine,Division of AIDS, University of BritishColumbia, Vancouver, Canada
Jo KimberResearch Fellow, Centre for Research onDrugs and Health Behaviour, LondonSchool of Hygiene and Tropical Medicine,University of London, UKNHMRC Postdoctoral Fellow, NationalCentre in HIV Epidemiology and ClinicalResearch, University of New South Wales,AustraliaTorsten KolindAssociate Professor, Centre for Alcoholand Drug Research, Aarhus University,DenmarkSusanne MacGregorProfessor and Leverhulme Emeritus Fellow,London School of Hygiene and TropicalMedicine, University of London, UKAnn McNeillProfessor of Health Policy and Promotion,UK Centre for Tobacco Control Studies,University of Nottingham, UKVirginia Montañés SánchezDrug user activist and researcher, Institute ofWomen Studies, University of Granada,Granada; FAUDAS Technical Coordination,Spain; ENCOD Membership European LevelJacek MoskalewiczHead of Department of Studies onAlcoholism and Drug Dependence,Institute of Psychiatry and Neurology,Warsaw, PolandDeborah OlszewskiSenior Scientific Analyst, EuropeanMonitoring Centre for Drugs and DrugAddiction, Lisbon, Portugal451
Harm reduction: evidence, impacts and challenges
Norah PalmateerEpidemiologist, Health Protection Scotland,Glasgow, UKAlessandro PironaScientific Analyst, Health and SocialResponses, European Monitoring Centrefor Drugs and Drug Addiction, Lisbon,PortugalJürgen RehmProfessor of Addictions, TechnischeUniversität, Dresden, Germany and Centrefor Addiction and Mental Health, Toronto,CanadaTim RhodesProfessor of Public Health Sociology, andDirector, Centre for Research on Drugsand Health Behaviour, London School ofHygiene and Tropical Medicine, Universityof London, UKRobin RoomProfessor of Social Alcohol Research,School of Population Health, University ofMelbourne, Australia and Centre forSocial Research on Alcohol and Drugs,Stockholm University, SwedenRoland Simon,Deputy Scientific Coordinator and Head ofInterventions, Law and Policies Unit,European Monitoring Centre for Drugsand Drug Addiction, Lisbon, PortugalMat SouthwellProject Manager, International Network ofPeople who Use Drugs, Bath UK
Alex StevensSenior Lecturer in Criminology, School ofSocial Policy, Sociology and SocialResearch, University of Kent, UKGerry V. StimsonProfessor of Sociology, and ExecutiveDirector, International Harm ReductionAssociation, UKHeino StöverProfessor, University of Applied Sciences,Frankfurt, GermanyBetsy ThomProfessor of Health Policy, School ofHealth and Social Sciences, MiddlesexUniversity, UKPeter VickermanSenior Lecturer in MathematicalModelling, HIV Tools and Centre forResearch on Drugs and Health Behaviour,London School of Hygiene and TropicalMedicine, University of London, UKMarcus WhitingESRC Post-doctoral Research Fellow, SocialPolicy, University of Birmingham, UKTomas ZabranskyCentre for Addictology, Charles University,Prague, Czech Republic
452
AbbreviationsAACACSADHDAIVLASSISTASUDAUDITBACBBNBBVBMTCASECBTCE markCEEHRNCMCNDCOPDCRESTCSCCSCDCRDfIDDPFUDWIECDPEMCDDAAmsterdam Addiction CohortAmsterdam Cohort Studyattention-deficit hyperactivity disorderAustralian Injecting and Illicit Drug Users LeagueA Stop Smoking in Schools TrialAuto-support parmi les Usagers de DroguesAlcohol Use Disorder Identification Testblood alcohol concentrationBest Bar Noneblood-borne virusbuprenorphine maintenance treatmentcannabis and smoking educationcognitive behaviour therapyConfirmatory European markCentral and Eastern European Harm Reduction Networkcontingency managementCommission on Narcotic Drugschronic obstructive pulmonary diseaseCocaine Rapid Efficacy Screening TrialCannabis Social ClubCorrectional Service of Canadadrug consumption roomDepartment for International Development (UK)Drug Policy Foundation — Usersdriving while intoxicatedEuropean Cities on Drug PolicyEuropean Monitoring Centre for Drugs and Drug Addiction455
Harm reduction: evidence, impacts and challenges
ENCODENHPSESPADEUFACFAUDASHBVHCVHDGHIVHubCAPPICNIDTSIDUIDUNIHRAINCBINPUDISHNLMPLNSLTLSDLTPLYPMDMAMIMMTMSICNDUDA456
European Coalition for Just and Effective Drug PoliciesEuropean Network of Health Promoting SchoolsEuropean School Survey Project on Alcohol and Other DrugsEuropean UnionSpanish Federation of Cannabis AssociationsSpanish Nationwide Network of People Affected by Drugs and HIVhepatitis Bhepatitis CHorizontal Drugs Grouphuman immunodeficiency virusHub of Commissioned Alcohol Projects and PoliciesInternational Coalition of NGOs for Just and Effective Drug PoliciesIntegrated Drug Treatment Systeminjecting drug userInternational Drug Users NetworkInternational Harm Reduction AssociationInternational Narcotics Control BoardInternational Network of People who Use DrugsInternational School Health Networklast month prevalencelow nitrosamine smokeless tobaccoLandelijk Steunpunt Druggebruikerslifetime prevalencelast year prevalence3,4-methylenedioxy-N-methamphetamine (ecstasy)motivational interviewingmethadone maintenance treatmentMedically Supervised Injecting Centre (Sydney)National Drug Users Development Agency
Abbreviations
NGONIDANIDUNSPNTAOSTPICPITCPLWHAPNPNDPNSPPOUQALYSRBSRCTRIPRIOTTRJBSDMSIFSLTSR-IRBSSTISTADSTDTASCTBTHC
non-government organisationNational Institute on Drug Abusenon-injection drug useneedle and syringe programmeNational Treatment Agencyopioid substitution treatmentPazienti Impazienti Cannabis (Cannabis Impatient Patients)provider-initiated HIV testing and counsellingpeople living with HIV/AIDSpharmaceutical nicotinpeer naloxone distributionprison needle and syringe exchange programmeproblem opioid userquality adjusted life yearsresponsible beverage servicerandomised control trialreduced ignition propensityRandomised Injectable Opiate Treatment TrialRotterdam Junkie Unionsyringe dispensing machinesupervised injection facilitysmokeless tobaccoself-reported injecting risk behaviourskin and soft tissue infectionStockholm Prevents Alcohol and Drug Problemssexually transmitted diseaseTackling Alcohol Related Street Crimetuberculosistetrahydrocannabinol457
Harm reduction: evidence, impacts and challenges
THRTobRegUKCAPPUNUNAIDSUNDCPUNGASSUNODCVANDUWHOYHLL
tobacco harm reductionWorld Health Organization Study Group of Tobacco Product RegulationUnited Kingdom Community Alcohol Prevention ProgrammeUnited NationsJoint United Nations Programme on HIV/AIDSUnited Nations Office on Drugs and Crime PreventionUnited Nations General Assembly Special SessionUnited Nations Office on Drugs and CrimeVancouver Area Network of Drug UsersWorld Health Organizationyears of healthy life lost
458
Further readingEMCDDA publications and studies in the field of harm reductionMonographs Series— http://www.emcdda.europa.eu/publications/monographsHarm reduction: evidence, impact and challenges—N� 10Available in English — ISBN: 92-9168-419-9 (April 2010)Hepatitis C and injecting drug use: impact, costs and policy options—N� 7Available in English — ISBN: 92-9168-168-7 (December 2004)Insights Series— http://www.emcdda.europa.eu/publications/insightsInjecting drug use, risk behaviour and qualitative research in the time of AIDS—N� 4Available in English — ISBN: 92-9168-124-5 (June 2002)Reviewing current practice in drug-substitution treatment in the European Union—N� 3Available in English — ISBN: 92-9168-104-0 (November 2000)Drugs in focus— http://www.emcdda.europa.eu/publications/drugs-in-focusCocaine use in Europe: implications for service delivery—N� 17Available in all EU languages — Catalogue number: TD-AD-07-003-EN-C (November 2007)Overdose: a major cause of avoidable death among young people — N� 13Available in all EU languages — Catalogue number: TD-AD-04-002-EN-C (January 2005)Hepatitis C: a hidden epidemic—N� 11Available in all EU languages — Catalogue number: TD-AD-03-005-EN-C (November 2003)Drug injecting challenges public health policy—N� 4Available in all EU languages — Catalogue number: TD-AD-02-004-EN-C (January 2002)Other studiesEuropean report on drug consumption roomsAvailable in English – Only electronic – http://www.emcdda.europa.eu/themes/harm-reduction/consumption-rooms(January 2004)461
Harm reduction: evidence, impacts and challenges
Guidelines for the evaluation of outreach work: a manual for outreach practitionersAvailable in English – Only electronic – http://www.emcdda.europa.eu/publications/manuals/outreach(December 2001)
Annual report and Statistical bulletinEMCDDA Annual report— http://www.emcdda.europa.eu/publications/annual-reportThe state of the drugs problem in the EU – analysis and statisticsEMCDDA Statistical bulletin— http://www.emcdda.europa.eu/stats/homeData tables and commentary
Web pages to related projectsHarm reduction:http://www.emcdda.europa.eu/themes/harm-reductionBest practice portal:http://www.emcdda.europa.eu/themes/best-practiceEpidemiological key indicators:http://www.emcdda.europa.eu/themes/key-indicatorsDeaths and mortality, Infectious diseases, Demand for treatment
462
European Monitoring Centre for Drugs and Drug AddictionEMCDDA Scientific Monograph Series No 10Luxembourg: Publications Office of the European UnionHarm reduction: evidence, impacts and challenges2010 — 462 pp. — 16 x 24 cmISBN 978-92-9168-419-9doi: 10.2810/29497Price (excluding VAT) in Luxembourg: EUR 25
How to obtain EU publicationsOur priced publications are available from the EU bookshop (http://bookshop.europa.eu), where you can place an order with the sales agent of your choice.The Publications Office has a worldwide network of sales agents. You can obtaintheir contact details by sending a fax to +352 292942758
About the EMCDDA
The European Monitoring Centre for Drugs and Drug Addiction(EMCDDA) is one of the European Union’s decentralised agencies.Established in 1993 and based in Lisbon, it is the central source ofcomprehensive information on drugs and drug addiction in Europe.The EMCDDA collects, analyses and disseminates factual, objective,reliable and comparable information on drugs and drug addiction. Indoing so, it provides its audiences with an evidence-based picture of thedrug phenomenon at European level.The Centre’s publications are a prime source of information for awide range of audiences including policymakers and their advisers;professionals and researchers working in the drugs field; and, morebroadly, the media and general public.EMCDDA monographs are comprehensive scientific publicationscontaining thematic papers prepared in the context of the Centre’sresearch studies and seminars. Topics include a wide range of issuesrelating to science, policy, theory and method.TD - A L- 10010- E N- C
Price (excluding VAT) in Luxembourg: EUR 25ISBN 978-92-9168-419-9